Management of Chronic Ankle Instability
Top Contributors - Ewa Jaraczewska, Jess Bell, Kim Jackson and Matt Huey
Definition of Chronic Ankle Instability (CAI)[edit | edit source]
Chronic ankle instability (CAI) has been defined as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.”[1] Chronic instability refers to feeling of apprehension in the ankle, “giving way” and recurrent ankle sprains, persisting for a minimum of 6 months after the initial sprain.[2]Symptoms include:[2]
- Lateral ankle pain
- Chronic swelling
- Difficulty walking on uneven terrain
Based on the International Classification of Function, Health and Disability (ICF) model, the effects of CAI on function and health include:
- In terms of impairments:[3]
- increased ligamentous laxity
- proprioceptive deficits
- In terms of activity limitations:[3]
- inability to walk
- inability to jump
- In terms of participation:[3]
- cessation of sport
- withdrawing from or decreasing occupational involvement
- decreasing the level of exercise
- change in type of sport
Long Term Outcomes[edit | edit source]
Patients with CAI have a loss of physical quality of life. Treatments may improve stability but are taking a long time and may require specialised equipment. [2]Seven years post-ankle inversion trauma study by Konradsen et al[4] revealed the following:
- 32% of patients reported chronic complaints of pain, swelling or recurrent sprains
- 72% of the subjects with residual disability reported that they were functionally impaired by their ankle
- 4% of patients experienced pain at rest and were severely disabled
- 19% were bothered by repeated inversion injuries
- 43% of these subjects felt that they could compensate by using an external ankle support
- 85% of people who develop CAI after unilateral sprain reported problems in the contralateral ankle.
According to Hertel [5]one sprain guarantees another. [5][2]Struijs and Kerkhoffs[6]indicated that 30% recurrence of sprain happened within the first year after the injury.[2]
Additional reported long-term outcomes include:
- Articular cartilage defects on the medial side of the joint due to:[2]
- Tearing of ATFL and CFL
- Altering and increasing peak cartilage strain
- Leading to tibiotalar cartilage degeneration (OA)
- Anterior talar positional fault [7]
- Altered movement patterns in unstable ankles:[2]
- Landing in more dorsiflexion in an attempt to minimise reliance on lateral ligaments and increase bony stability
- In drop jump: greater maximum calcaneal eversion and frontal displacement of the body
- Faster time to peak ground reaction force in drop landing
- Greater medial ground reaction force.
- Metatarsal height is lowered during a terminal swing of gait
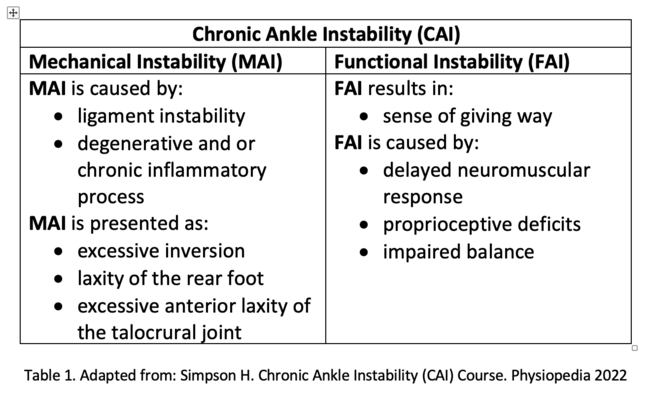
Mechanical and Functional Instability[edit | edit source]
There are two commonly accepted subgroups of CAI: mechanical instability and functional instability. [2][3]In Hertel's model [8] of ankle stability, mechanical and functional instability are part of a continuum. Recurrent sprain occurs when both conditions are present. [8]
Mechanical Instability[edit | edit source]
Mechanical instability is referred to as pathological ligamentous laxity about the ankle-joint complex[9]Mechanical instability may result from various anatomic changes that are present in isolation or in combination. They can lead to pathologies that are responsible for ankle instability. [3]
Functional Instability[edit | edit source]
There is no universally approved definition of functional ankle instability.[10] Based on definition established by Evans et al.,[11] functional instability is a subjective complaint of weakness.[11] Lentell and his colleagues [12] describes functional instability as ankle pain and the perception that the ankle is less functional than the other side or the situation prior to the injury. [12] Tropp et al. [13] concluded, that a joint motion that did not exceed normal physiologic limits, but was no longer controlled voluntarily, defines functional instability. [13]
Impaired proprioceptive and neuromuscular control can be responsible for functional instability.[8]
Table 1 summerises the causes and the results of mechanical and functional ankle instability:[2]
Diagnostic Procedures[edit | edit source]
Clinicians may also use diagnostic tools that provide a range or scale of information that could indicate if the patient presents with a deficiency (eg, range of motion, perceived disability) that helps to define a condition. evidence-based assessments of diagnostic tools is the importance of consistent findings in the literature. A clinician must decide if conclusions from published studies are homogeneous or heterogeneous. Obviously, if the findings related to the utility of a diagnostic tool are more homogeneous, then the clinician should be more willing to implement the tool if the findings suggest consistent positive utility; in contrast, if multiple studies show the tool cannot provide good diagnostic discrimination, the clinician should not spend time and resources using the tool.[14]
- Anterior drawer test is performed in slight knee flexion to relax the gastrocnemius, but Kovaleski et al[15] suggested a testing position with the knee flexed to 90° and the ankle in 10° of plantar flexion to isolate the anterior talofibular ligament. [15] A bilateral comparison is recommended. [14] Excessive anterior translation and the lack of a solid end feel indicate positive test results.
- Stress Radiography is used to quantify the extent of ankle-joint laxity. It shows the separation of the bony joint structures while a force is applied. Clinically it helps to identify excessive strain within the ligamentous structures. A total anterior translation greater than 9 mm or translation greater than 5 mm (or both) when compared with the contralateral side indicates significant laxity of the anterior talofibular ligament. Pathologic laxity of the CF ligament is demonstrated by a talar tilt angle greater than 10° in total or more than 5° greater than the contralateral limb. [14]
- MRI is not conclusive. Negative MRI results must be viewed with caution in a symptomatic patient and arthroscopy should be considered.[16]
- Diagnostic ultrasound offers moderate to strong confirmation of lateral ligamentous injury, evidence suggests.[17]It shows an increased lateral ligament lengths during the anterior drawer and talar tilt tests among individuals with a history of CAI.[18]
- Stable force plates are suggested for gait and hop stability assessment[19]
- Imaged guided injections of cortisone as clinical diagnostic tool
Physiotherapy Management[edit | edit source]
add text here relating to diagnostic tests for the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train. 2002 Dec;37(4):364-375.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Simpson H. Chronic Ankle Instability Course. Physiopedia 2022
- ↑ 3.0 3.1 3.2 3.3 3.4 Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. Journal of athletic training. 2011 Mar;46(2):133-41.
- ↑ Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002 Jun;12(3):129-35.
- ↑ 5.0 5.1 Hertel J. Immobilisation for acute severe ankle sprain. Lancet. 2009 Feb 14;373(9663):524-6.
- ↑ Struijs PA, Kerkhoffs GM. Ankle sprain. BMJ Clin Evid. 2010 May 13;2010:1115.
- ↑ Wikstrom EA, Hubbard TJ. Talar positional fault in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010 Aug;91(8):1267-71.
- ↑ 8.0 8.1 8.2 Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train. 2002 Dec;37(4):364-375
- ↑ Tropp H. Commentary: Functional Ankle Instability Revisited. J Athl Train. 2002 Dec;37(4):512-515.
- ↑ Konradsen L. Factors Contributing to Chronic Ankle Instability: Kinesthesia and Joint Position Sense. J Athl Train. 2002 Dec;37(4):381-385.
- ↑ 11.0 11.1 Evans GA, Hardcastle P, Frenyo AD. Acute rupture of the lateral ligament of the ankle. To suture or not to suture? J Bone Joint Surg Br. 1984 Mar;66(2):209-12
- ↑ 12.0 12.1 Lentell G, Katzman LL, Walters MR. The Relationship between Muscle Function and Ankle Stability. J Orthop Sports Phys Ther. 1990;11(12):605-11.
- ↑ 13.0 13.1 Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985 Jun;6(3):180-2.
- ↑ 14.0 14.1 14.2 Gribble PA. Evaluating and differentiating ankle instability. Journal of athletic training. 2019 Jun;54(6):617-27.
- ↑ 15.0 15.1 Kovaleski JE, Norrell PM, Heitman RJ, Hollis JM, Pearsall AW. Knee and ankle position, anterior drawer laxity, and stiffness of the ankle complex. J Athl Train. 2008 May-Jun;43(3):242-8.
- ↑ Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010 Jun;16(2):78-80.
- ↑ Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010 Jan;39(1):41-7.
- ↑ Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012 Jul;42(7):593-600.
- ↑ McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008 Oct;40(10):1810-9.