Skin Anatomy, Physiology, and Healing Process
Top Contributors - Stacy Schiurring, Jess Bell, Kim Jackson and Lucinda hampton
Introduction[edit | edit source]
Our skin, part of the integumentary system, is the largest organ system in the human body. However, it is often overlooked and under appreciated for the role it plays in overall health.[1] Many people only consider the role skin plays in our appearance and how we are perceived by the society. Facial expressions are an important form of non-verbal communication and can have a strong social influence.[2] While our skin is an important part of our outer appearance, it provders a greater contribution to human life and wellbeing than just aesthetics.[1]
This article will overview the anatomy and physiology of skin, skin's response to injury, normal tissue healing, the phases of acute wound healing, and the altered healing in chronic wounds.
Wound healing is complex and involves the coordination of many intricate processes. There are many factors that can impact wound healing, both positively and negatively.
The Role of the Skin[edit | edit source]
Skin provides numerous functions vital to life and is important for overall health.[1]. Skin's health and appearance can be an indicator of general health, and skin integrity failure often accompanies the failure of other systems within the body.[3]
8 Key Functions of the Skin[1]:
- Protection: Skin acts as a physical barrier to the external environment and provides protection for internal organs against external threats[1][4]
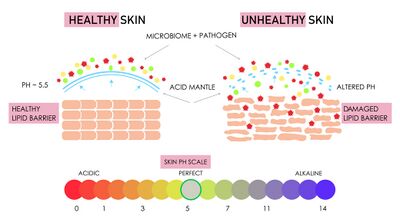
- Immune function: Our skin contains a protective acidic barrier called the acid mantle. This acidic layer has a pH between 4.2 and 6.0 and this creates a hostile environment for harmful invading organisms while maintaining a favourable environment for beneficial microbes.[1] The acid nature of skin is a key requesite for healthy skin. Skin pH can affect the synthesis and maintenance of a competent skin barrier, play a role in skin pigmentation, and ion homeostasis.[5] Skin pH tends to be lower in people with darker skin because melanin byproducts are acidic and skin pH also tends to increase slightly as we age, which can contribute to an increase in the risk of infection and alter our healing ability.[1].
Specific immune cells and proteins contained in the dermis which activate the immune response and attack invading microbes. These cells include: Langerhans cells, memory T cells, and lymphoid cells.[4]
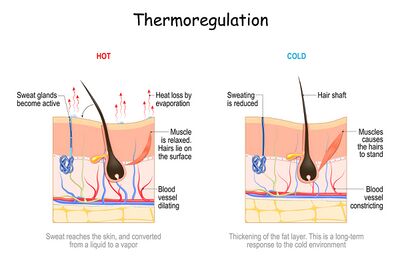
The surface of our skin houses millions of bacteria, fungi and viruses that compose the skin microbiome and serves as a physical barrier to prevent the invasion of pathogens. As in our gut, the skin microbiome plays essential roles in the protection against invading pathogens, the education of the immune system,[6] and contributing back to the pH of the acid mantle.[1] - Thermoregulation: Humans, and all mammals, can maintain a stable core body temperature via thermoregulatory responses. By increasing blood flow to the skin through vessel dilation, body temperates are lowered by evaporative cooling of moist/sweaty surfaces to release body heat. [1][7] However, if water lost to evaporative cooling is not replaced, body fluid homeostasis will be challenged.[7]
- Prevention of fluid loss: In addition to the physical barrier provided by skin, it also contains lipids, proteins, amino acids, and salts that work to maintain internal body homeostasis by attracting and holding onto water. Due to this mechanism, under normal circumstances, the outer layer of our skin is about 30% water.
- Synthesis of vitamin D: Vitamin D is recognized as a prohormone, also known as calciferol. There are two major forms of vitamin D: D2 which is human-made and fortified into foods (such as milk cheese, yogurt, cereals, and juices) and D3 which is synthesized by the skin and from eating animal-based foods (fatty fish, fish liver oil, and egg yolk).[8]. While vitamin D can be ingested through food or supplements, the skin and exposure to sunlight is the body's primary source of vitamin D.[1] Vitamin D is essential for calcium and phosphate absorption, bone formation, renal function, and our immune function.[1] [8]
- Protection from ultraviolet radiation: Ultraviolet radiation (UVR) can cause DNA photodamage, sunburn, and cause both local and systemic immunosuppressive properties.[9] Melanin and carotene give skin its colour and serve to reflect UVR as a protective mechanism to radiation damage.[1] Melanin also has antioxidant and radical scavenging properties.[9] Melanin is produced by melanocytes in response to increased sunlight, which is why populations that evolved in areas with more sun exposure tend to have darker skin.[1]
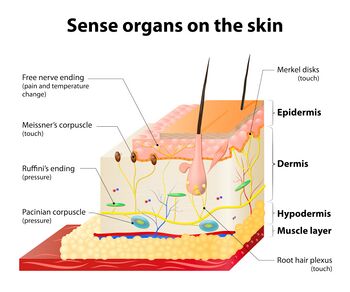
- Interaction with the environment: Our skin gathers sensory information through free nerve endings, hairs, receptors to touch, temperature, pain. In addition, through physiological processes like sweating or blushing, information is shared about our internal state to the outside world.[1]
- Healing: Tissue restoration in response to injury.[1]
Please view the following short optional video for an overview of the roles and functions of the skin.
Skin Anatomy and Physiology[edit | edit source]
It's important to understand the layers of our skin so that we can understand how healing occurs differently based on depth. The skin has two principle layers, the epidermis and the dermis. The hypodermis is considered an extension of the skin by some sources, but not by others.[1]
The Epidermis[edit | edit source]
- Composed of five layers
- It is avascular
- It's thickness varies based on location, for example it is thickest on the heels and thinnest on the eyelids. Areas that have increased use from friction or weight bearing can build up thicker layers of skin, for example where a pencil rubs your writing finger or shoe rubs against your foot.
- It has no nerves, however free nerve endings from the dermis do extend into the mid layers of the epidermis.
Five layers of the epidermis (moving from least to most superficial):
- Stratum basale
- Only layer that undergoes continuous mitosis to produce new cells[1]
- Keratinocytes are constantly being produced in the stratum basale and they move up through the layers until they reached the outermost layer.[1] They are the most dominant cell type in the skin and play a critical role in wound healing as both structural cells and via important immune functions. [11]
- Melanocytes are also produced in this layer. They produce melanin, which contributes to the colour of skin. Humans have approximately the same amount of melanocytes, therefore skin colour is based on the amount of melanin that those melanocytes produce in response to their environment.[1]
- Also contains Merkel cells which can perform both nervous and endocrine actions. They can synthesize and store locally produced hormones and neurotransmitters. They function as mechanoreceptors [1] for light and selective tactile perception but not to hard touch and vibration; they are also involved in the transfer of nociceptive signals.[12]
- Stratum spinosum. This layer contains Langerhans cells and lymphocytes that play an important role in the immune system.
- Stratum spinosum
- Contains Langerhans cells and lymphocytes which play an important role in the immune system.[1]
- Stratum granulosum
- This layer contains the greatest concentration of free nerve endings that extend from the dermis. Free nerve endings are an unencapsulated dendrite originating from a sensory neuron. They are the most common nerve endings in skin and provide sensory information about painful stimuli, hot and cold, and to light touch, however they are less sensitive to abrupt changes in stimulation.[13]
- This is the most superficial layer of the epidermis which contains living cells.[1]
- Stratum lucidum
- Contains two to three layers of keratinocytes and is not living. It can be penetrated or shaved off without awareness.
- It is only found in areas of thick skin, like the palms of the hand and the soles of the feet. Present in calluses.[1]
- Stratum corneum
- Composed of 15 to 30 layers of keratinocytes called squames or corneocytes. These are the dead keratinocytes which contain a high concentration of keratin that provide a waterproof barrier for the skin, hair, and nails.
- This layer is continually being shed from the body. Shed cells are replaced via the process of skin cell migration from the stratum basale. This process takes an average of 30 days, but this will vary by age and certain health conditions. [1]
The Dermis[edit | edit source]
The dermis contains blood vessels and nerves and supplies the epidermis through capillary loops and free nerve endings. It consists of two layers. The first is the papillary layer that interdigitates with the epidermis and it's the ridges of this layer that give us our unique fingerprint. The papillary layer also contains fibroblasts, mast cells, macrophages, and leukocytes. So fibroblasts are responsible for the production of collagen, elastin, and proteins. And this gives our skin its strength and flexibility. Mast cells produce heparin and histamine, which play a big role in clot formation and in the inflammatory response. Macrophages in this layer play an important role in immune response, wound repair, cancer defence, salt balance, and hair regeneration. They are perhaps the most well known for destroying foreign invaders through phagocytosis. So if you recall from biology class, phagocytosis is the process by which cells envelop and digest other cells.
The reticular layer is between the papillary layer and the subcutaneous layer or hypodermis. It is made up of collagen, blood vessels, nerve endings, T-cells, hair follicles and glands. The hair follicles contain stem cells that produce keratinocytes that will become hair, and they've been shown to play an important role in wound healing by contributing epithelial cells to close the wound. The T-lymphocytes are responsible for destroying pathogens and malignant cells and the nerves located in the dermis detect sensations such as itching, touch, pressure, vibration, pain, and temperature. While injuries that extend into the dermis can be associated with increased pain due to nerve exposure and damage, they also have the advantage of bleeding, which helps to protect the nerve endings and can result in less pain than the superficial paper cuts that don't bleed. So when nerves have been completely damaged by an injury or burn, there's no pain experienced at all because the system is no longer functioning. Remember, nerves are there to provide information about our environment and the interpretation occurs in our brain. So when the nerves have been damaged, there's no information coming in to interpret and so some of these wounds with nerve damage will have no pain.
The Hypodermis[edit | edit source]
It's located below the dermis and contains subcutaneous tissue. Some sources will consider it an extension of the skin and others won't. For our purposes, we won't. It's made up of loose connective tissue, adipose tissue, it's very well vascularised, well innervated. It helps attach the skin to the muscles and bones through superficial fascia, and also provides insulation and cushioning through fat storage.
Wounds[edit | edit source]
ADD definition of a wound
When there's injury to the skin, wounds and tissue loss can be categorised based on their depth and also the tissues involved.
There's typically three categories that wounds fall into depending on their depth. (MAKE INTO A TABLE?)
- The first is erosion. This is loss of the superficial epidermis only, with no loss of the dermis. These wounds are unlikely to bleed, although they may appear red. Some examples are superficial abrasions, stage one pressure injuries or superficial burns, formerly known as first degree burns. Healing occurs through local inflammatory process and epidermal replacement from keratinocyte migration upward. Clinically, you'll see erythema and pain that is mild and pretty short-lived.
- The next category is a partial thickness wound. This involves loss of the epidermis and part of the dermis. So these wounds will bleed. They include stage two pressure injuries, superficial and deep partial thickness burns, formerly known as second-degree burns, skin tears, and some deep abrasions. Healing here occurs through re-epithelialisation as a result of epithelial cell migration from the wound edges towards the centre of the wound. Clinically you would see bleeding, seeping of serous fluid, blistering, or pain.
- The final category is full thickness wounds. This is loss of both the epidermis and dermis with extension into the subcutaneous tissue. So this may involve bone, tendon, ligament, or muscle. It includes full thickness burns formerly known as third-degree burns, stage three and four pressure injuries, surgical incisions, traumatic wounds and necrotic wounds that required some deep debridement. This type of healing occurs through the process of secondary intention, which we're going to talk about in a little bit.
Normal Tissue Healing[edit | edit source]
Must understand normal healing process to understand when things go wrong.
So when we're talking about healing, the process of tissue repair is incredibly complex. It's a symphony of events involving many systems and a full description could take an entire course of its own. But for brevity here, we're going to discuss the basic series of events.
There are four mechanisms by which healing takes place.
- The first is continuous cell cycling. So this is how normal intact skin is replaced, through keratinocyte production in the stratum basale followed by upward migration through the layers of the epidermis that we discussed previously.
- The second is cell proliferation. This is a repair process where healthy cells undergo mitosis to repair damage. The new tissue formed through this process is called granulation tissue. The structure and function of lost tissue is not exactly duplicated, but it is similar to the original and is accompanied by some scarring.
- The third type of tissue healing is regeneration. This type of healing occurs through complete duplication of structure and function, and only some tissues are capable of this, such as the liver, kidney, gastrointestinal tract and the epidermis. Okay. Nothing else can do that.
- And the fourth type of healing is fibroproliferative healing. This is pathological, where lost tissue is not replaced and the body replaces it with a fibrous scar instead. This may happen with deep wounds, persistent inflammation, fibroproliferative diseases, or any other underlying health conditions.
there are four different categories of healing.
This is important to know so that you know what to expect when you're dealing with a particular type of wound. The longer that a wound is open, the more significant the residual scar will be. This is important to know so that you can focus on reducing healing time and also provide the patient with realistic expectations.
- Category one refers to wounds that heal by primary intention. This means surgical wounds, where an incision is made. The tissue is free from contamination and there's minimal tissue loss. These wounds are closed with external force using sutures, staples, adhesive strips or glue. Epidermal regeneration is the primary mechanism of healing and contraction and scarring are minimal here. There are no complications. These wounds close in about two weeks time, okay.
- Category two refers to wounds healed by delayed primary intention. These are surgical wounds where the decision is made not to approximate the wound edges due to concern about contamination, active infection, or significant tissue loss. Once the wound has sufficiently healed or been freed from debris and pathogens, it is then closed with sutures, staples, grafting, or skin flap placement, okay. So these wounds have the potential to result in significant scarring if closure is delayed or chronic inflammation sets in.
- Category three refers to wounds healing by secondary intention. This is the process that the majority of wound care practice revolves around. These wounds extend into the subdermal tissue and they heal as a result of the body's inflammatory response, formation of new granulation tissue to fill the empty space, and then re-epithelialisation or new skin formation over the top. The edges are approximated through wound contraction due to myofibroblasts, which functions similar to smooth muscle cells and sort of march their way across the wound. These wounds typically take weeks to months to close, depending on size and other factors that may complicate the process.
- Category four refers to partial thickness wounds that heal by re-epithelialisation. Since the subdermal layers are not involved, wound contraction's not a factor, there's minimal to no granulation tissue, minimal to no scarring. The duration to closure for these wounds depends on depth, but ranges from one to two weeks. So those are pretty fast and you won't see those often.
four phases of healing
When we're looking at tissue healing and how that happens, with every wound the body goes through four phases of healing. These phases are not consecutive, but they overlap with each other, okay. So while the completion of this entire healing process lasts up to two years, acute ones are typically closed in about 21 days. If healing is disrupted and the wound is still open after about four weeks, it's considered chronic.
- The first phase of wound healing is haemostasis or clot formation. Think of this like an ambulance and fire being called to the site of a building explosion. Blood vessels respond immediately with vasoconstriction to prevent blood loss and tissue injury, platelets arrive at the site along with fibrin, and they form a clot to provide a temporary barrier to the external environment. Once dry, these clots are what form what we know is a scab, right? The scab is a body's temporary wound dressing that prevents blood loss and protects us from the outside world while the tissue repair takes place underneath. This process begins within seconds and it continues for the first 12 hours after injury.
- The second phase of healing is the inflammatory phase. So think of this as the initial cleanup of debris, once the emergency personnel has left, someone has to come in and clean up a mess from the building explosion, right? So this phase is important to kill any pathogens that may have entered the body, remove debris and dead tissue, and then stimulate new blood vessel growth. Neutrophils, mast cells, and macrophages all play a big role in this phase. The process is essential to acute wound healing, but can become problematic if it persists for too long. This inflammatory phase occurs in the first 24 hours after injury and typically lasts for about one week. You can see it clinically as redness, swelling, heat, and pain.
- The third phase of healing is the proliferative phase. If we go back to our emergency analogy, once the debris has been cleaned up, reconstruction must begin. So this phase of repair is characterised by new blood vessel formation or angiogenesis, connective tissue growth or fibroplasia, new skin cell formation or epithelialisation, and continued cleaning out of any remaining debris. Neutrophils, mast cells, and macrophages are still present during this phase, but the most predominant types are fibroblasts and endothelial cells, which are responsible for the growth of granulation tissue and capillaries. Fibroblasts initially produce type three collagen, which tends to be weaker and more disorganised than type one collagen. Granulation tissue is bright red, beady, vascular tissue that fills in the wound cavity. It's made up of collagen, elastin, and blood vessels. Within hours of injury, re-epithelisation begins with upward migration of the existing keratinocytes. So like we talked about the process before, within a few days, the process continues with cell proliferation through mitosis. The time it takes for a wound to be considered closed varies based on the circumferential size and also the depth. There will be a visible scar if the wound takes more than three to four weeks to re-epithelialise. This proliferative phase begins around four to six days after injury and can last from three weeks to two months. So even though the wound may appear closed once it's re-epithelialised it's not considered healed until the next phase is complete. That's when the tissue is more susceptible to injury from outside sources.
- This final phase of tissue injury is the remodelling phase. This is where the wound contracts, granulation tissue settles, blood flow decreases down to pre-injury levels, and the wound tensile strength increases. Myofibroblasts are responsible for wound contraction essentially by marching across the wound. Fibroblasts, myofibroblasts, endothelial cells, and macrophages are the most predominant cells and they slowly decrease as this phase progresses. During this phase, type three collagen is slowly replaced by type one collagen, which has increased tensile strength. The remodelling phase begins about two weeks after injury and lasts up to two years. So this means the wound may appear healed before this process is complete. At about six weeks after injury, the wound has about half its ultimate tensile strength. And once the remodelling phase is complete, that wounded area will only have about 80% of its original strength. These timelines are important to keep in mind when you're working with patients that have had chronic or repeated wounds, or even patients that have recent wounds or surgery so that you know what to expect and you can, sort of, give them expectations.
Chronic Wounds[edit | edit source]
Chronic wounds are those that do not follow this normal process of healing. They are not closed or making significant progress towards healing in three weeks. These wounds have a disruption in the process. They do not follow the normal trajectory that we just covered. These are the wounds that you're most likely to encounter in your practice. In chronic wounds, the skin microbiome often tips in the balance in favour of the harmful microbiome over the beneficial ones. And these microbes can trigger the immune system to attack the body's cells required for healing rather than attacking the invaders. Chronic wounds may get stuck in one or more phases that persists for months or years. And the most common phase to be stuck in is the inflammatory phase. It's common for chronic wounds to go through periods of healing, stagnation, regression, and reoccurrence.
Chronic wounds typically have one or more of the following characteristics. They have a multifactorial aetiology. That person has advanced age or obesity, they've had a previous wound, injury or surgery, especially in the same area. Multiple co-morbidities, particularly vascular diseases, diabetes, or auto-immune conditions. Prolonged standing or dependency. So that's going to change the ability of blood flow return to their hearts. Mechanical forces or recurrent trauma, maybe that's from their shoe rubbing or something else that's pressure. Poor tissue perfusion or oxygenation. Medications that they are on can affect their wound healing, inadequate or inappropriate care, malnutrition, that's a big one that's often overlooked. Active infection, presence of a bacterial biofilm or changes in the skin microbiome.
There are five most common types of chronic wounds that you're likely to encounter. Those are venous insufficiency wounds, and those are the most common type of chronic wound that you're going to encounter in the clinic setting. Next are neuropathic wounds, related to diabetic neuropathy. Pressure injuries, these are formerly known as pressure ulcers or decubitus ulcers. Arterial ulcers, and then non-healing surgical wounds. And the non-healing surgical wounds typically have a lot of those previous things that we just talked about, like multiple co-morbidities or medications or what have you.
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 Palmer, D. Skin Anatomy, Physiology, and Healing. Physiotherapy Wound Care Programme. Physioplus. 2022.
- ↑ Crivelli C, Fridlund AJ. Facial displays are tools for social influence. Trends in cognitive sciences. 2018 May 1;22(5):388-99.
- ↑ Sussman C, Bates-Jensen BM, editors. Wound care: a collaborative practice manual. Lippincott Williams & Wilkins; 2007.
- ↑ 4.0 4.1 Naik S. One Size Does Not Fit All: Diversifying Immune Function in the Skin. The Journal of Immunology. 2022 Jan 15;208(2):227-34.
- ↑ Surber C, Humbert P, Abels C, Maibach H. The acid mantle: a myth or an essential part of skin health?. pH of the Skin: Issues and Challenges. 2018;54:1-0.
- ↑ Byrd AL, Belkaid Y, Segre JA. The human skin microbiome. Nature Reviews Microbiology. 2018 Mar;16(3):143-55.
- ↑ 7.0 7.1 McKinley MJ, Martelli D, Pennington GL, Trevaks D, McAllen RM. Integrating competing demands of osmoregulatory and thermoregulatory homeostasis. Physiology. 2018 May 1;33(3):170-81.
- ↑ 8.0 8.1 Ross AC, Taylor CL, Yaktine AL, Del Valle HB. Committee to review dietary reference intakes for vitamin D and calcium. Food and Nutrition Board. 2011 Jun 22.
- ↑ 9.0 9.1 Brenner M, Hearing VJ. The protective role of melanin against UV damage in human skin. Photochemistry and photobiology. 2008 May;84(3):539-49.
- ↑ YouTube. The science of skin | TED-Ed. Available from: https://www.youtube.com/watch?v=OxPlCkTKhzY [last accessed 11/06/2022]
- ↑ Piipponen M, Li D, Landén NX. The immune functions of keratinocytes in skin wound healing. International journal of molecular sciences. 2020 Jan;21(22):8790.
- ↑ Abraham J, Mathew S. Merkel cells: a collective review of current concepts. International Journal of Applied and Basic Medical Research. 2019 Jan;9(1):9.
- ↑ Molnar C and Gair J. Concepts of Biology – 1st Canadian Edition. BCcampus. Retrieved from https://opentextbc.ca/biology/ 2015.