Glioblastoma
Original Editors - Simone Potts from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Definition/Description[edit | edit source]
Glioblastoma Multiforme develops from star-shaped glial cells that support nerve cells. A glioblastoma multiforme is classified as a grade IV astrocytoma. It is also referred to as a glioblastoma or GBM[1]
Glioblastoma multiforme (GBM) is the most common and most malignant of the glial tumors. Media attention was brought to this form of brain cancer when Senator Ted Kennedy was diagnosed with glioblastoma and ultimately died from it.
Gliomas are a heterogeneous group of neoplasms that differ in location within the central nervous system. There is no particular age or sex distribution. Growth potential, extent of invasiveness, morphological features, tendency for progression, and response to treatments vary between each case diagnosed.
GBM can spread through the brain tissue, but rarely spreads to other areas outside of the central nervous system.
All GBM tumors have abnormal and numerous blood vessels, a common feature of a fast-growing tumor. These blood vessels deliver necessary oxygen and nutrients to the tumors, helping them grow and spread. In addition, these blood vessels easily mix with normal brain tissue and travel away from the main tumor, which makes GBM tumors a challenge to treat.[2]
Prevalence[edit | edit source]
Approximately 60% of the estimated 17,000 primary brain tumors diagnosed in the United States each year are gliomas.
Glioblastoma multiforme is the most frequent primary brain tumor. In most European and North American countries, incidence is approximately 2-3 new cases per 100,000 people per year. [2]
Characteristics/Clinical Presentation[edit | edit source]
• Most invasive type of glial tumor
• Commonly spreads to nearby tissue
• Grows rapidly
• Includes distinct genetic subtypes
• May be composed of several different kinds of cells (i.e., astrocytes, oligodendrocytes)
• May have evolved from a low-grade astrocytoma or an oligodendroglioma
• Common among men and women in their 50s-70s
• More common in men than women
• Accounts for 17 percent of all primary brain tumor[1]
The most common presentation of patients with glioblastomas is a slowly progressive neurologic deficit, usually motorweakness. However, the most common symptom experienced by patients is headache.
Patients may present with generalized symptoms of increased intracranial pressure (ICP), including headaches, nausea and vomiting, and cognitive impairment.
General symptoms include headaches, nausea and vomiting, personality changes, and slowing of cognitive function.
Headaches can vary in intensity and quality, and they frequently are more severe in the early morning or upon first awakening.
Changes in personality, mood, mental capacity, and concentration can be early indicators or may be the only abnormalities observed.
Focal signs include hemiparesis, sensory loss, visual loss, aphasia, and others.
Seizures are a presenting symptom in approximately 20% of patients with supratentorial brain tumors.[2]
o Increased Intracranial Pressure
o Headache, especially retroorbital; sometimes worse upon awakening, improves during the day
o Vomiting (with or without nausea)
o Visual changes (blurring, blind spots, diplopia, abnormal eye movements)
o Changes in mentation (impaired thinking, difficulty concentrating or reading, memory or speech)
o Personality change, irritability
o Unusual drowsiness, increased sleeping
o Sensory changes
o Muscle weakness or hemiparesis
o Bladder dysfunction
o Increased lower extremity reflexes compared with upper extremity reflexes
o Decreased coordination, gait changes, ataxia
o Positive Babinski reflex
o Clonus (ankle or wrist)
o Vertigo, head tilt [3]
Associated Co-morbidities[edit | edit source]
add text here
Medications[edit | edit source]
add text here
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
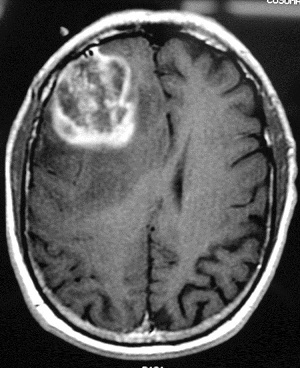
T1-weighted axial gadolinium-enhanced magnetic resonance image demonstrates an enhancing tumor of the right frontal lobe. Image courtesy of George Jallo, MD. [2]
Image taken from: emedicine.medscape.com/article/340870-overview
• MRI with and without contrast is the study of choice in diagnosing this dis. These lesions typically have an enhancing ring observed on T1-weighted images and a broad surrounding zone of edema apparent on T2-weighted images.
• Currently, no specific laboratory studies are helpful in making a diagnosis of glioblastoma.
• Positron emission tomography (PET) scans and magnetic resonance (MR) spectroscopy can be helpful in identifying glioblastomas in difficult cases, such as those associated with radiation necrosis or hemorrhage. On PET scans, increased regional glucose metabolism closely correlates with cellularity and reduced survival.[4]
Etiology/Causes[edit | edit source]
The etiology of glioblastoma remains unknown in most cases. Familial gliomas account for approximately 5% of malignant gliomas, and less than 1% of gliomas are associated with a known genetic syndrome.
Although concerns have been raised regarding cell phone use as a potential risk factor for development of gliomas, study results have been inconsistent, and this possibility remains controversial. The largest studies have not supported cell phone use as a cancer risk factor. However, a recently released multinational report concluded that studies that are independent of the telecom industry show that cell phone use may pose a significant risk for brain tumors, and some European countries have taken steps to limit cell phone use by children.[2]
Systemic Involvement[edit | edit source]
add text here
Medical Management (current best evidence)[edit | edit source]
Standard treatment is surgery followed by radiation therapy or a combination of radiation therapy and chemotherapy. If surgery is not an option, the doctor may administer radiation therapy followed by or combined with chemotherapy. Many clinical trials using radiation, chemotherapy, or a combination are available for initial and recurrent GBM. Clinical trials using molecularly targeted therapies showing success in other cancers are also being tested in GBM patients. [1]
Upon initial diagnosis of glioblastoma multiforme (GBM), standard treatment consists of maximal surgical resection, radiotherapy, and concomitant and adjuvant chemotherapy with temozolomide.[5]
Physical Therapy Management (current best evidence)[edit | edit source]
No universal restrictions on activity are necessary for patients with glioblastomas. The patient's activity depends on his or her overall neurologic status. The presence of seizures may prevent the patient from driving. In many circumstances, physical therapy and/or rehabilitation are extremely beneficial. Activity is encouraged to reduce the risk of deep venous thrombosis.[5]
Alternative/Holistic Management (current best evidence)[edit | edit source]
add text here
Differential Diagnosis[edit | edit source]
Anaplastic astrocytoma
Cavernous malformation
Cerebral abscess
CNS lymphoma
Encephalitis
Intracranial hemorrhage
Metastasis
Oligodendroglioma
Radiation necrosis
Toxoplasmosis[4]
Case Reports/ Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1zepmoDGp3XTKZAQU0EPaK8ExMkl8HQAfYYAnfMDQ66fj3MQIM|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 http://www.braintumor.org/patients-family-friends/about-brain-tumors/tumor-types/glioblastoma-multiforme.html?gclid=CNGRyOuN2KcCFSVe7AodwCdk8Q
- ↑ 2.0 2.1 2.2 2.3 2.4 http://emedicine.medscape.com/article/283252-overview
- ↑ Goodman C, Snyder T. Differential Diagnosis for Physical Therapists: Screening for Referral. St. Louis, MO: Saunders Elsevier: 2007.
- ↑ 4.0 4.1 http://emedicine.medscape.com/article/283252-diagnosis
- ↑ 5.0 5.1 http://emedicine.medscape.com/article/283252-treatment