Male Urinary Incontinence
Top Contributors - Stacy Schiurring, Kim Jackson, Lucinda hampton and Jess Bell
This page aims to provide an introductory discussion of men's health physiotherapy with regards to male sexual dysfunction. Please note that further training is required through a reputable pelvic health education company before attempting the techniques discussed in this page. See the Resources section at the bottom of this page for links to pelvic and men's health special interest groups.
Introduction[edit | edit source]
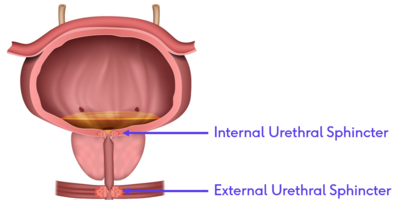
Normal urinary continence is maintained when the closure pressure of the urethra is greater than the pressure from the bladder above it. This requires a complex interaction between the autonomic nervous system that controls the more proximal smooth muscles of the internal urethral sphincter and the somatic nervous system that controls the striated muscles of the external urethral sphincter.[1]
| Innervation | Type of Muscle | Function and Features | |
|---|---|---|---|
| Internal Urethral
Sphincter |
Autonomic control | Smooth muscle |
|
| External Urethral
Sphincter |
Somatic voluntary control | Striated skeletal muscle |
|
Problems can occur for a variety of reasons. There can be problems with the closure mechanism of the urethra which would result in stress incontinence or problems with the bladder itself which could result in frequency, urgency and urge incontinence. Male urinary incontinence has a significant psychosocial impact affecting the individual's quality of life, work absenteeism and depression. It can also have a significant emotional impact on the individual's spouse, partner or care provider.[3]
The Micturition Cycle[edit | edit source]
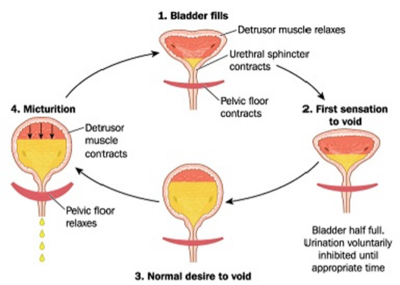
Urinary continence is a pressure game.[2] Maintaining urinary continence is a complex interaction between the bladder, brain, muscles of the pelvic floor, and social contexts. The bladder spends 99% of the time in a storage phase, collecting urine as it arrives from the kidneys via the ureters. The bladder undergoes receptive relaxation of the detrusor muscle to allow for the increasing volume without a rise in pressure. Low storage pressure is needed to allow urine drainage into the bladder from the upper urinary tract. While the bladder is in its storage phase, the urethra and the sphincteric mechanism are closed and the high outlet resistance pressure maintains continence. Urinary continence is maintained when the pressure in the urethra exceeds the pressure in the bladder. Urethral pressure is generated by the sphincter mechanism.[3]
When it is time to void, a series of coordinated parasympathetic peripheral and central pathways cause the urinary sphincters to relax while activating the detrusor muscle. Bladder fullness is a stimulus for voiding, and urge is a motivator.[3]
The following short video provides a thorough summary of the micturition cycle.
Types of Male Urinary Incontinence[edit | edit source]
Stress Urinary Incontinence[edit | edit source]
Stress incontinence occurs when the closure force of the sphincter mechanism is unable to control the amount of pressure being exerted from the bladder, resulting in leaking urine.[5]
There are multiple internal and external sources of pressure:
- forced exhalations such as coughing, sneezing, or laughing
- running, jumping
- post-catheter insertion
- cystoscopy
- TURP operation
- typical after a prostatectomy
Stress urinary incontinence is typically treated by addressing urinary sphincter strength and or control, and pressure management.[2]
Urgency or Overactive Bladder[edit | edit source]
Urgency is when a person has a strong, sudden need to urinate. This is also known as an overactive bladder.
Mixed Urinary Incontinence[edit | edit source]
Mixed urinary incontinence is a combination of stress and urgency incontinence.
Other Types of Urinary Incontinence[edit | edit source]
- Nocturia is the need to wake up at night to go urinate.
- Nocturnal Enuresis is leaking of urine during sleep.
- Post-micturition dribble is leaking that occurs immediately after urination.
- Continuous urinary leakage is the inability to maintain any continence.
Physiotherapy Treatment for Male Incontinence[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Hodges PW, Stafford RE, Hall L, Neumann P, Morrison S, Frawley H, Doorbar-Baptist S, Nahon I, Crow J, Thompson J, Cameron AP. Reconsideration of pelvic floor muscle training to prevent and treat incontinence after radical prostatectomy. InUrologic Oncology: Seminars and Original Investigations 2019 Dec 25. Elsevier.
- ↑ 2.0 2.1 2.2 Roscher, P. Men's Health. Male Urinary Incontinence. Physioplus. 2022.
- ↑ 3.0 3.1 3.2 Nahon I. Physiotherapy management of incontinence in men. Journal of physiotherapy. 2021 Apr 1;67(2):87-94.
- ↑ YouTube. The Micturition Reflex | Bladder Nerve Supply | Renal Physiology. Available from: https://www.youtube.com/watch?v=Zl4VoTpxluQ [last accessed 23/03/2022]
- ↑ 5.0 5.1 Abrams P, Andersson KE, Apostolidis A, Birder L, Bliss D, Brubaker L, Cardozo L, Castro-Diaz D, O'connell PR, Cottenden A, Cotterill N. 6th International Consultation on Incontinence. Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence.Neurourology and urodynamics. 2018;37(7):2271-2.