Joubert Syndrome
Introduction[edit | edit source]
Joubert syndrome (JS) is a rare autosomal recessive genetic heterogeneously inherited disorder characterized by hypotonia, ataxia, developmental delay, intellectual disability, abnormal eye movements, and neonatal respiratory dysregulation, among other neurological features.[1] Joubert syndrome is characterized by the absence or underdevelopment of the cerebellar vermis - an area of the brain that controls balance and coordination -- as well as a malformed brain stem (molar tooth sign). The most common features of Joubert syndrome in infants include abnormally rapid breathing (hyperpnea), decreased muscle tone (hypotonia), abnormal eye movements, impaired intellectual development, and the inability to coordinate voluntary muscle movements (ataxia). Extra fingers and toes (polydactyly), a cleft lip or palate, and tongue anomalies are all possible physical malformations. Kidney and liver abnormalities can develop, and seizures may also occur. Many cases of Joubert syndrome appear to be sporadic (not inherited). In most other cases, Joubert syndrome is inherited in an autosomal recessive manner (meaning both parents must have a copy of the mutation) via mutation in at least 10 different genes, including NPHP1, AHI1, and CEP290.[2]
Clinical characteristics:[edit | edit source]
Classic Joubert syndrome (JS) is characterized by three primary findings:[3]
- A distinctive cerebellar and brain stem malformation called the molar tooth sign (MTS)
- Hypotonia
- Developmental delays
Often these findings are accompanied by
- Episodic tachypnea or apnea and/or atypical eye movements.
- Breathing abnormalities that improved with age.
- Truncal ataxia
- Delayed acquisition of gross motor milestones
- Cognitive abilities are variable (ranging from severe intellectual disability to normal)
- Retinal dystrophy,
- Renal disease
- Ocular colobomas
- Occipital encephalocele
- Hepatic fibrosis
- Polydactyl
- Oral hematomas
- Endocrine abnormalities
Diagnosis[edit | edit source]
The clinical diagnosis of JS is based on the presence of characteristic
clinical features[edit | edit source]
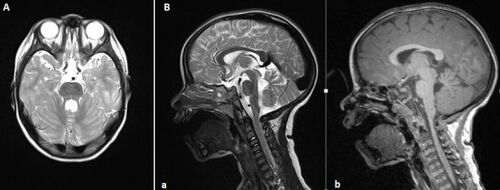
MRI findings[edit | edit source]
The MRI Sign of the molar tooth comprises an abnormally deep interpeduncular fossa; prominent, straight, and thickened superior cerebellar peduncles; and hypoplasia of the vermis, the midline portion of the cerebellum.
To date pathogenic variants in 34 genes are known to cause JS; 33 of these are autosomal recessive and one is X-linked. A molecular diagnosis of JS can be established in about 62%-94% of individuals with a clinical diagnosis of JS by identification of biallelic pathogenic variants in one of the 33 autosomal recessive JS-related genes or a heterozygous pathogenic variant in the one X-linked JS-related gene.
Management:[edit | edit source]
Treatment of manifestations: Infants and children with abnormal breathing may require stimulatory medications (e.g., caffeine); supplemental oxygen; mechanical support; or tracheostomy in rare cases. Other interventions may include speech therapy for oromotor dysfunction; occupational and physical therapy; educational support, including special programs for the visually impaired; and feedings by gastrostomy tube. Surgery may be required for polydactyly and symptomatic ptosis and/or strabismus. Nephronophthisis, end-stage renal disease, liver failure and/or fibrosis are treated with standard approaches.
Surveillance[edit | edit source]
Annual evaluations of growth, vision, and liver and kidney function; periodic neuropsychologic and developmental testing.
Agents/circumstances to avoid: Nephrotoxic medications such as nonsteroidal anti-inflammatory drugs in those with renal impairment; hepatotoxic drugs in those with liver impairment.
Genetic counseling:[edit | edit source]
JS is predominantly inherited in an autosomal recessive manner. JS caused by pathogenic variants in OFD1 is inherited in an X-linked manner. Digenic inheritance has been reported.
For autosomal recessive inheritance: at conception, each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. Once the pathogenic variants have been identified in an affected family member, carrier testing for at-risk family members, prenatal testing for pregnancies at increased risk, and preimplantation genetic testing are possible. For pregnancies known to be at increased risk for JS, prenatal diagnosis by ultrasound examination with or without fetal MRI has been successful.
- ↑ Alam S, Khatoon F, Khan N. Joubert syndrome: a case report. [cited 2021 Oct 31]; Available from: https://doi.org/10.1186/s43161-021-00039-7
- ↑ Parisi M, Glass I. Joubert syndrome. GeneReviews®[Internet]. 2017 Jun 29.
- ↑ Parisi M, Glass I. Joubert Syndrome Summary. 2019;1–52
- ↑ Jellouli M, Gargah T. Sign of the «molar tooth»: characteristic MRI appearance of Joubert syndrome. The Pan African Medical Journal. 2015 Oct 13;22:127-.