Objective Vestibular Assessment
Top Contributors - Jess Bell, Kim Jackson, Rucha Gadgil and Robin Tacchetti
Introduction[edit | edit source]
As discussed here, the therapist needs to conduct a thorough subjective assessment of the vestibular patient in order to determine the nature and potential cause of his / her symptoms. The objective assessment must be equally thorough and include a range of tests, from oculomotor testing to dynamic visual acuity and gait / balance assessments. This page will discuss the key components of the objective assessment of the vestibular patient.
Objective Evaluation[edit | edit source]
Vision Screening[edit | edit source]
Oculomotor screen[edit | edit source]
When conducting any vision screening or testing, it is important to watch and ask the patient how must effort a task requires and the degree of symptoms provoked. The basic oculomotor screen during a vestibular assessment should include:[1]
- Fixation in primary and eccentric gaze
- Smooth pursuit or tracking
- Vestibulo-ocular reflex (VOR) cancellation
- Saccades
Oculomotor Testing[edit | edit source]
Spontaneous Nystagmus[edit | edit source]
Spontaneous nystagmus is tested in primary and eccentric gaze. It occurs due to the unopposed tonic neural activity of the intact side when there are lesions in the peripheral vestibular systems (acute) or central vestibular pathways.[1]
Primary gaze is tested as follows:[1]
- The patient looks forward and visually fixates on a target
- This position is held for 10 seconds and the therapist looks for any nystagmus
Eccentric gaze:[1]
The most common pathological type of nystagmus driven by the CNS is gaze evoked nystagmus (GEN). It is tested as follows:[1]
- The patient to fixate on a position 30 degrees to each side, up and down (i.e. an eccentric position)
- Each position is held for 10 seconds and the therapist looks for nystagmus
- GEN is only present with eccentric gaze, not in primary gaze
It is important to differentiate between GEN and end point nystagmus. End point nystagmus occurs when gaze is held at the end of range. End point nystagmus is considered normal, so in order to test for GEN it is essential that the patient only holds his / her gaze 30 degrees off-centre.[1][2]
For a summary of the difference between peripheral and central nystagmus, please see Table 1.
| Findings | Peripheral | Central |
|---|---|---|
| Effect of fixation (room light) | Nystagmus is typically absent within 2-3 days in room light | Nystagmus either does not change or it increases |
| Direction of nystagmus | Usually mixed plane (horizontal and torsional) | Usually single plane (sustained down beating) |
| Effect of gaze | Nystagmus increases with gaze toward direction of quick phase | Nystagmus either does not change or it reverses direction |
Smooth Pursuit and VOR Cancellation[edit | edit source]
- Slow, tracking eye movements that maintain images of smaller moving targets (20 to 30 degrees per second) on the fovea[1][3]
- Centrally mediated reflex[1]
Smooth Pursuit Eye Movements[edit | edit source]
- Refixation saccades occur during target motion toward the side of the lesion
- There may be unilateral or bilateral refixation saccades[1]
VOR Cancellation[edit | edit source]
- Head and eyes move with a target - suppressing the VOR
- Refixation saccades will occur during head movement toward the side of the lesion[1]
Smooth Pursuit Torsion Test[edit | edit source]
- The smooth pursuit neck torsion test measures smooth pursuit eye movement with the head / trunk in neutral and when the trunk and neck are rotated relative to a stationary head[4]
- Smooth pursuit neck torsion test is considered to be specific for detecting eye movement disturbances due to altered cervical sensory input[5][6]
- A decrease in velocity gain of smooth pursuit eye movements during the test is only seen in patients with neck pain[1]
Saccadic Eye Movements[edit | edit source]
Saccades are defined as: “fast conjugate eye movements that shift the eyes from one target to another, bringing an object of interest into focus on the fovea where visual acuity is highest”.[7]
Saccades are centrally mediated – there are volitional saccades and reflexive saccades.[8][9]
In order to test saccadic eye movements:[1]
- Instruct the patient to look between two targets as quickly as possible – vertical and horizontal
- During these fast changes in eye position, the therapist looks at the amplitude, velocity and accuracy of targeting
- Hypometric saccade = when the patient ‘undershoots’ the target
- Hypermetric saccade = when the patient ‘overshoots’ the target
One hypometric saccade is typically considered normal. Two or more hypometric or one or more hypermetric saccades is considered abnormal.[1]
Vestibulo-Ocular Reflex (VOR) Testing[edit | edit source]
The VOR is the primary mechanism for gaze stability during head movement. There are two tests of VOR function that can be done effectively in the clinic without an infrared camera system:[1]
- The Head thrust test
- The dynamic visual acuity (DVA) test
The head shaking test can also be conducted, but it works better with an infrared camera system.[1]
Head Thrust Test[edit | edit source]
The head thrust test (HTT) is generally accepted as a useful clinical test for assessing the angular vestibulo-ocular reflex.[10] The test is performed as follows:[1][10]
- The patient is asked to focus on a target
- The therapist gently grasps the patient’s head and applies a small-amplitude, high-acceleration thrust
- It must be performed quickly
- The patient must not be able to predict on which side the thrust will be applied
- The therapist observes the patient’s eyes for corrective saccades once the head stops moving
- Refixation saccades indicate decreased VOR gain - i.e. a positive test
- The testing side is the side that the head is thrusted towards:[1]
- Positive head thrust on right side = right sided deficit
- Corrective saccades to right and left = bilateral deficit
Dynamic Visual Acuity[edit | edit source]
There are different ways to assess dynamic visual acuity (VOR), including the dynamic visual acuity (DVA) test. The DVA compares static with dynamic visual acuity. A positive DVA test indicates the presence of oscillopsia or impaired gaze stability with head movement.[1]
Older Acuity Chart[edit | edit source]
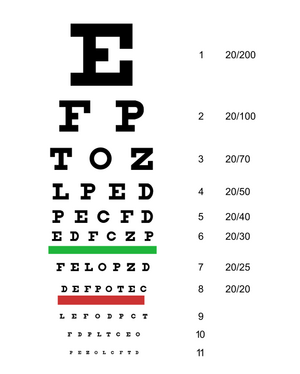
Utilises a 10 ft LogMar or Snellen chart (see Figure 1). There should be the same number of optotypes (i.e. letters) per line on the chart, but these charts do not have this feature.[1]
Current Acuity Chart[edit | edit source]
The current acuity chart does have the same number of optotypes on each line. A copy this chart can be found at i-see.org.
When using this chart, the patient’s distance from the chart can be varied. Each line on the acuity chart has a recommended distance.[1]
The test is conducted as follows:[1]
- Patient starts two feet away from the chart in a sitting position
- The patient’s head is tipped down into slight flexion
- Patients should wear glasses if required
- The patient reads the static visual acuity chart with his / her head still
- The following instruction is given:
- “Read the lowest line that is clear to you”
- The patient reads from left to right to the lowest line possible until she / he misses at least one optotype on a line
- The line above this (i.e. where no optotypes were missed) is the static DVA line
- Then, the therapist silently chooses a line that is 4 to 6 lines above the static DVA line
- The therapist begins turning the patient’s head horizontally at 2 Hz or 120 bpm on a metronome
- The therapist tells the patient which line to start reading with the same instructions - using colours next to the lines can help to tell the patient where to start
- The patient continues to read down the chart from left to right until she / he misses at least one optotype on a line
- At this point, testing is stopped
- The line above the one where the patient began missing optotypes while the head was moving is the dynamic DVA line
To score the test, count the difference between the static and dynamic DVA lines (where there were no optotypes missed in each of these lines). If there is a three or more line difference, then the DVA is considered abnormal. This reflects a functional measurement of the VOR.[1]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 Tonks B. Vestibular Assessment Course. Physioplus, 2021.
- ↑ Serra A, Leigh RJ. Diagnostic value of nystagmus: spontaneous and induced ocular oscillations. J Neurol Neurosurg Psychiatry. 2002;73(6):615-8.
- ↑ Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. Types of Eye Movements and Their Functions. Available from: https://www.ncbi.nlm.nih.gov/books/NBK10991/
- ↑ Tjell C, Rosenhall U. Smooth pursuit neck torsion test: a specific test for cervical dizziness. Am J Otol. 1998;19(1):76-81.
- ↑ Daly L, Giffard P, Thomas L, Treleaven J. Validity of clinical measures of smooth pursuit eye movement control in patients with idiopathic neck pain. Musculoskelet Sci Pract. 2018;33:18-23.
- ↑ Majcen Rosker Z, Vodicar M, Kristjansson E. Inter-visit reliability of smooth pursuit neck torsion test in patients with chronic neck pain and healthy individuals. Diagnostics (Basel). 2021;11(5):752.
- ↑ Termsarasab P, Thammongkolchai T, Rucker JC, Frucht SJ. The diagnostic value of saccades in movement disorder patients: a practical guide and review. J Clin Mov Disord. 2015;2:14.
- ↑ Patel SS, Jankovic J, Hood AJ, Jeter CB, Sereno AB. Reflexive and volitional saccades: biomarkers of Huntington disease severity and progression. J Neurol Sci. 2012;313(1-2):35-41.
- ↑ McDowell JE, Dyckman KA, Austin BP, Clementz BA. Neurophysiology and neuroanatomy of reflexive and volitional saccades: evidence from studies of humans. Brain Cogn. 2008;68(3):255-70.
- ↑ 10.0 10.1 Schubert MC, Tusa RJ, Grine LE, Herdman SJ. Optimizing the sensitivity of the head thrust test for identifying vestibular hypofunction. Phys Ther. 2004;84(2):151-8.