Glycosides and Congestive Heart Failure
Introduction[edit | edit source]
The two types of glycosides used to treat CHF are digoxin and digitoxin, the primary being digoxin.
- Cardiac glycosides, including digitalis and digoxin, have long-standing use in clinical practice.
- Superior therapies with milder adverse effects and better safety profiles have now replaced it, such as beta-blockers and calcium-channel blockers.
- In current practice, they are reserved as a backup drug when first-line agents are ineffective.
- Its optimal use is in the treatment of mild to moderate heart failure in adult patients and to increase myocardial contraction[1].
- Digoxin is a positive inotropic agent that activates the sodium-calcium membrane exchange pump which increases the intracellular calcium concentrations. This increase in calcium will lead to stronger contractions of the heart. Digoxin also reduces sympathetic responses via the vagus nerve, which will reduce overall heart rate. The combination of increased contractility and reduced heart rate creates a more efficient pump for cardiac output[2].
- Digitoxin is similar in structure and effects to digoxin, though the effects are longer-lasting. Unlike digoxin (which is eliminated from the body via the kidneys), it is eliminated via the liver, so could be used in patients with poor kidney function. However the evidence for its use is poor and it is rarely used in western medicine.[3]
Digoxin[edit | edit source]
Pharmacokinetics
- Digoxin is traditionally taken orally, with doses between 0.125mg- 0.25mg daily, with large storage taking place in skeletal muscles.
- It is mostly absorbed through the small intestine and metabolized in the liver through hydrolysis, oxidation, and conjugation[4]. Approximately 70% of digoxin is cleared through the kidneys and has a half-life of 36 hours.
Side effects[edit | edit source]
Toxicity is a common adverse effect caused by higher concentrations of serum Digoxin. Monitoring blood concentrations is important to prevent toxicity, especially if the patient has renal complications or is elderly. Serum digoxin concentration levels should remain between 0.5 nmol/L to 0.9 nmol/L, depending on the body weight of the patient. Chronic toxicity, more common than acute toxicity, may occur if these concentrations reach above the therapeutic dose for a prolonged period of time.
These effects include dysrhythmias, altered mental status, drowsiness, visual disturbances, gastrointestinal issues, and altered potassium levels[5].
Identifying signs of these adverse effects are critical for a physical therapists to maintain patient safety. Despite these potential negative effects, patients on digoxin can participate in physical therapy better than without the medication. Due to digoxin’s effect on cardiac output, the heart is able to more effectively pump blood into the system, improving the exercise tolerance of the patient.
Conclusions[edit | edit source]
There have been no major advances in the pharmacological management of patients hospitalized for worsening chronic HF over the last 2 decades. These patients remain at high risk for early readmission or death .
Digoxin
- Has multiple favorable properties that make it an ideal therapy for worsening chronic HF.
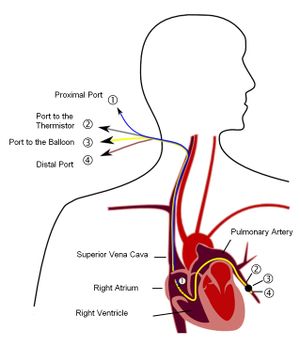
- Is the only available inotrope known to increase CO and decrease pulmonary capillary wedge pressure (ie pressure obtained when a catheter is passed from the right side of the heart into the pulmonary artery as far as it will go and "wedged" into an end artery. The pressure distal to the wedged catheter is an approximation of cardiac left atrial pressure[6]) without causing deleterious increases in heart rate or decreases in blood pressure.
- Improves signs and symptoms of HF and functional status.
- Is known to reduce all-cause and HF-specific hospitalizations[7]. .
References[edit | edit source]
- ↑ David MN, Shetty M. Digoxin. InStatPearls [Internet] 2020 Mar 4. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK556025/ (last accessed 26.9.2020)
- ↑ Campbell, T. J., & MacDonald, P. S. (2003, July 21). Digoxin in heart failure andcardiac arrhythmias. Retrieved from https://www.mja.com.au/journal/2003/179/2/digoxin-heart-failure-and-cardiac-arrhythmias
- ↑ WIkipedia Digitoxin Available from: https://en.wikipedia.org/wiki/Digitoxin#cite_note-Belz-1 (last accessed 19.6.2019)
- ↑ Iisalo E. Clinical pharmacokinetics of digoxin. Current neurology and neuroscience reports. https://www.ncbi.nlm.nih.gov/pubmed/322907. Accessed November 26, 2018.
- ↑ MacLeod-Glover, N., Mink, M., Yarema, M., & Chuang, R. (2016). Digoxin toxicity: Case for retiring its use in elderly patients? Canadian Family Physician, 62(3), 223–228
- ↑ Medical Dictionary for the Health Professions and Nursing © Farlex 2012 Available from:https://medical-dictionary.thefreedictionary.com/Dictionary
- ↑ Ambrosy AP, Pang PS, Gheorghiade M. Digoxin for worsening chronic heart failure: underutilized and underrated. Available from:https://heartfailure.onlinejacc.org/content/4/5/365 (last accessed 26.9.2020)