Telehealth for Low Back Pain
Introduction[edit | edit source]
Telehealth can be defined as the provision of healthcare remotely through form of telecommunications such as a telephone or laptop. This wiki page reviews the use of Telehealth in the patient population with lower back pain (LBP).
What is Telehealth?[edit | edit source]
Telehealth is a modality in which a healthcare professional such as a Physiotherapist, Nurse or Doctor can consult with a patient through video or audio call by means of a telephone, laptop, mobile phone, or tablet. Telehealth is a term which is used interchangeably with ‘telemed,’ ‘telemedicine,’ ‘physiodirect,’ and ‘teleconsultation.’ Ultimately, this service allows a healthcare professional and a patient to consult when they are not able to gather face to face for a variance of reasons [1].
History of Telehealth[edit | edit source]
The term Telehealth originated in the mid-20th century when healthcare professionals would attend to infectious disease patients from a distance using bells and signs. In the 1970’s Telehealth developed into what we know it to be today. Originally, NASA needed to solve being able to monitor astronaut’s health whilst in space. There developed Telehealth through means of video call. In the 1980’s militants on large vessels and workers on oil rigs in the surroundings of the USA would consult with healthcare professionals at the LA medical centre through telephone and video call. As it was unrealistic for them to see someone face to face, Telehealth became their best option to get immediate advice.
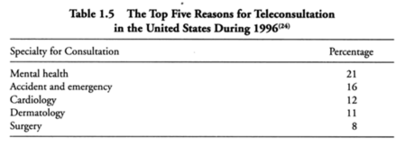
Fast forward to the 1990’s, the USA become the largest consumer of telephone consultations, surpassing Norway. In 1996, figure (2) demonstrates what areas these types of consultations were being used for [1].
Validity and Reliability of Telehealth[edit | edit source]
Validity is the ability of a measure or modality to achieve what it is intended to achieve. When a modality has high validity, the results can be more trusted or believed [2]. A randomised control trial conducted in 2014 investigated the validity of telehealth in lower back pain compared to face-to-face appointments. It found that telehealth’s validity was varied dependant on the specific element of the assessment, as show below:
Detection of pain with specific movements- High validity
Identifying the quality lumbar movement- Moderate validity
Postural analysis- Poor validity
Identifying reasons for limitations- Poor validity
The study concludes that ‘Important components of the standard musculoskeletal assessment of LBP are valid via telerehabilitation in a clinical setting.’ [3]
Reliability is the ability of a measure or modality to achieve the same results when the measure is repeated [2]. The inter-rater reliability of telehealth (0.92-0.96) is deemed ‘very good.’ Intra-rater reliability is also deemed very good (0.92-0.96) [4].
Telehealth as a tool for Assessing Low Back Pain[edit | edit source]
Tools for Assessments[edit | edit source]
Future Improvements to Telehealth Assessments[edit | edit source]
Telehealth as a tool for Management Low Back Pain[edit | edit source]
Management Options[edit | edit source]
Future Improvements to Telehealth Managements[edit | edit source]
Pros and Cons of Telehealth[edit | edit source]
•Travelling is often unaffordable to individuals living in remote areas, telehealth can provide a solution to this
•Healthcare is often inaccessible to people, which has been highlighted in the global pandemic of 2020, telehealth provides a solution to this
•There is now a push to use technology in order to enhance health services [5].
•Telehealth has been shown to be effective in managing health conditions such as obesity and asthma.
•Reduces healthcare costs by improving efficiency and revenue
•Possibility of better continuity of care
•LBP has a high prevalence rate of 39% [6] worldwide, finding ways to ease the burden of face to face care is important.
•Poor patient compliance is associated with telehealth [7].
•Patients often decline to use telehealth due to preferring face to face contact
•May lead to fragmentation of care amongst multiple providers
•There may be a lower quality of patient clinician relationship
•Patients may have a lack of access to necessary technology
• Initial cost of acquiring technical equipment
•Many argue its overall effectiveness for dealing with LBP
•The problem of establishing patient rapport
Conclusion[edit | edit source]
References[edit | edit source]
IMAGE 1: http://2.bp.blogspot.com/--szGmCEUsJU/Vo8IjEZaqiI/AAAAAAAAc3s/ffCzwHxM4eg/s1600/VoIP%2BDr.jpg
IMAGE 2: Darkins, A. & Cary, M. (2000) Telemedicine and Telehealth: Principles, Policies, Performances and Pitfalls. 1st ed. USA: Springer Publishing Company.
Dario Moreti Cabral A, Almeida L, (2017) Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342‐1351.Available at doi:10.1016/j.spinee.2017.04.008
Toon (2002) Using Telephones in Primary Care British Medical Journal 2002;324:1230 Available at: https://doi.org/10.1136/bmj.324.7348.1230
- ↑ 1.0 1.1 Darkins, A. & Cary, M. (2000) Telemedicine and Telehealth: Principles, Policies, Performances and Pitfalls. 1st ed. USA: Springer Publishing Company.
- ↑ 2.0 2.1 Grove, S. and Cipher, D. (2020) ‘Statistics for nursing research.’ 3rd ed. Missouri: Elsevier: pp 41-56
- ↑ Truter, P., Russel, T. & Fary, R. ‘Low Back Pain via Telerehabilitation in a Clinical Setting’ Telemedicine and e-Health; 20(2) pp 1-12.
- ↑ Palacin- Marin, F., Esteban-Moreno, B., Olea, N., Herrera-Viedma, E. & Arroyo-Morales, M. ‘Agreement between telerehabilitation and face-to-face clinical outcome assessments for low back pain in primary care’ Health Service Research; 38(11); pp 947- 952.
- ↑ Dario Moreti Cabral A, Almeida L, (2017) Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342‐1351.Available at doi:10.1016/j.spinee.2017.04.008
- ↑ Murray, C.J. Vos, T., Lozano, R, Naghavi, M, Flaxman, A.D., Michaud, C., Ezzati, M., Shibuya, K., Salomon, J.A., Abdalla, S. and Aboyans, V.(2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The lancet, 380(9859), pp.2197-2223. Available at: https://doi.org/10.1016/S0140-6736(12)61689-4
- ↑ Toon (2002) Using Telephones in Primary Care British Medical Journal 2002;324:1230 Available at: https://doi.org/10.1136/bmj.324.7348.1230