Hand Rheumatoid Arthritis
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (19/03/2020)
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Introduction[edit | edit source]
Rheumatoid arthritis (RA) is a chronic inflammatory disease affecting the hand joints and leading to impairment in hand functions.
- Most common clinical presentation of RA is polyarthritis of small joints of hands: proximal interphalangeal (PIP), metacarpophalangeal (MCP) joints and wrist.
- The hand is one of the main elements of the rehabilitation of patients with rheumatoid arthritis (RA) due to deformities, which occur in approximately 90% of patients.
- It is a serious problem, both in the psychological and functional aspect, connected with muscle strength reduction, a limited range of motion and non-acceptance of the changes in the shape of the limb.[1]
- Adults with RA should have access to specialist physiotherapy, with periodic review (NICE guideline)[2]
Clinically Relevant Anatomy[edit | edit source]
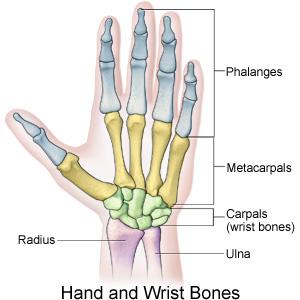
The hand contains a complex range of structures which permit a wide variety of movements, many of which are essential for day-to-day tasks. For anatomy see Wrist and Hand
- Synovium - In patients with rheumatoid arthritis, the synovium is strongly thickened and inflamed.
- RA affects the joints of the hand and wrist including
- Wrist joint
- Metacarpal joints
- Metacarpophalangeal Joint (MCPJ) – condyloid joints comprised of the articulation between metacarpal and proximal phalanx in each of the 5 digits.
- Interphalangeal Joints – between the phalanges and there are two in each digit. The thumb is an exception, and has only oneinterphalangeal joint. The two joints are the:
- Proximal Interphalangeal Joints (PIPJ)
- Distal Interphalangeal Joints (DIPJ)
Pathological Process[edit | edit source]
Rheumatoid arthritis (RA) is a chronic inflammatory systemic disease.
- The immunological process within the connective tissue contributes to progressive disability.
- It starts in the synovial membrane and leads to a gradual deterioration of articular and periarticular structures and deformity development.
- Problems which are constantly experienced by RA patients include morning joint stiffness and reduced muscle strength.
- The first symptoms are symmetrical carpal and metacarpophalangeal arthritis manifested by pain, oedema, exudate and a limited range of motion.
- Progressive hand dysfunction contributes to various limitations in the personal, social and professional aspects of life.
- Pain is the dominant symptom reported by patients.
- Rheumatic pain is chronic and lasts from the onset of the disease until the end of a patient’s life[1]
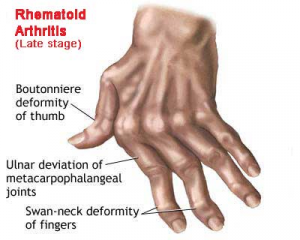
Clinical Presentation[edit | edit source]
Most common clinical presentation of RA is polyarthritis of small joints of hands: proximal interphalangeal (PIP), metacarpophalangeal (MCP) joints and wrist (other commonly affected joints include wrist, elbows, shoulders, hips, knees, ankles and metatarsophalangeal (MTP) joints).
- Most commonly joint involvement occurs insidiously over a period of months, however, in some cases, joint involvement may occur over weeks or overnight.
- Stiffness in the joints in the morning may last up to several hours, usually greater than an hour.
- On examination, there may be swelling, stiffness, deformity, and tenderness of the PIP, MCP wrist, synovitis, and there may be a decreased range of motion.
- The patient may have: "trigger finger" due to flexor tenosynovitis; "boutonniere (flexion at PIP and extension at DIP); swan neck (flexion at DIP and extension at PIP) deformities; subluxation of MCP joints; ulnar deviation; carpal tunnel syndrome; tenosynovitis.
- Rheumatoid nodules may be present in 20% of patients with rheumatoid arthritis; these occur over extensor surfaces at elbows, heals, and toes.[3]
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
Rehabilitation is a long-term process depending on the grade and type of deformity and activity of disease.
Exercises which strengthen muscles and increase joint mobility are beneficial.
Exercise intensity needs to be constantly controlled and adjusted to the activity of disease.
During the exacerbations the exercises should be performed in hospital or on an outpatient basis under strict supervision of a therapist.
Numerous therapeutic regimens are introduced during the chronic stage. These address both the dysfunctions and individual needs of the patient, including professional activity or hobbies.
Irrespective of the activity of disease, it is extremely important to teach the patient how to behave and perform activities of daily living in a safe way in order to limit excessive joint loading.
The improved function of the hand may be maintained with the continuation of an exercise programme at home. Functional assessment is a basic tool to determine hand dysfunction severity.[1]
Differential Diagnosis[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Księżopolska-Orłowska K, Sadura-Sieklucka T, Kasprzak K, Gaszewska E, Rodkiewicz-Bogusławska A, Sokołowska B. The beneficial effects of rehabilitation on hand function in patients with rheumatoid arthritis. Reumatologia. 2016;54(6):285. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241364/ (last accessed 20.3.2020)
- ↑ NICE Rheumatoid arthritis in Adults:Management Available from:https://www.nice.org.uk/guidance/ng100/chapter/Recommendations (last accessed 20.3.2020)
- ↑ Rheumatoid Arthritis updated feb 2020 Krati Chauhan; Jagmohan S. Jandu; Amandeep Goyal; Pankaj Bansal; Mohammed A. Al-Dhahir. Available from:https://www.ncbi.nlm.nih.gov/books/NBK441999/ (last accessed 20.3.2020)