Hand Rheumatoid Arthritis
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (19/03/2020)
Original Editor - Your name will be added here if you created the original content for this page.
Lead Editors
Introduction[edit | edit source]
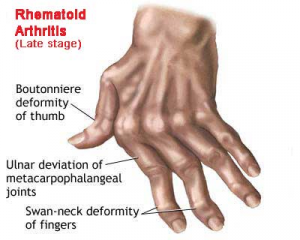
Rheumatoid arthritis (RA) is a chronic inflammatory disease affecting the hand joints and leading to impairment in hand functions.
- Most common clinical presentation of RA is polyarthritis of small joints of hands: proximal interphalangeal (PIP), metacarpophalangeal (MCP) joints and wrist.
- The hand is one of the main elements of the rehabilitation of patients with rheumatoid arthritis (RA) due to deformities, which occur in approximately 90% of patients.
- It is a serious problem, both in the psychological and functional aspect, connected with muscle strength reduction, a limited range of motion and non-acceptance of the changes in the shape of the limb.[1]
- Adults with RA should have access to specialist physiotherapy, with periodic review (NICE guideline)[2]
Clinically Relevant Anatomy[edit | edit source]
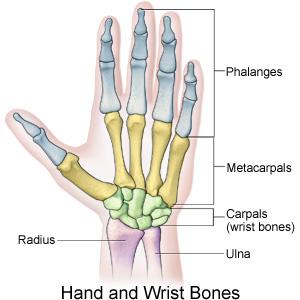
The hand contains a complex range of structures which permit a wide variety of movements, many of which are essential for day-to-day tasks. For anatomy see Wrist and Hand
- Synovium - In patients with rheumatoid arthritis, the synovium is strongly thickened and inflamed.
- RA affects the joints of the hand and wrist including
- Wrist joint
- Metacarpal joints
- Metacarpophalangeal Joint (MCPJ) – condyloid joints comprised of the articulation between metacarpal and proximal phalanx in each of the 5 digits.
- Interphalangeal Joints – between the phalanges and there are two in each digit. The thumb is an exception, and has only oneinterphalangeal joint. The two joints are the:
- Proximal Interphalangeal Joints (PIPJ)
- Distal Interphalangeal Joints (DIPJ)
Pathological Process[edit | edit source]
Rheumatoid arthritis (RA) is a chronic inflammatory systemic disease.
- The immunological process within the connective tissue contributes to progressive disability.
- It starts in the synovial membrane and leads to a gradual deterioration of articular and periarticular structures and deformity development.
- Problems which are constantly experienced by RA patients include morning joint stiffness and reduced muscle strength.
- The first symptoms are symmetrical carpal and metacarpophalangeal arthritis manifested by pain, oedema, exudate and a limited range of motion.
- Progressive hand dysfunction contributes to various limitations in the personal, social and professional aspects of life.
- Pain is the dominant symptom reported by patients.
- Rheumatic pain is chronic and lasts from the onset of the disease until the end of a patient’s life[1]
Clinical Presentation[edit | edit source]
add text here relating to the clinical presentation of the condition
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 Księżopolska-Orłowska K, Sadura-Sieklucka T, Kasprzak K, Gaszewska E, Rodkiewicz-Bogusławska A, Sokołowska B. The beneficial effects of rehabilitation on hand function in patients with rheumatoid arthritis. Reumatologia. 2016;54(6):285. Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241364/ (last accessed 20.3.2020)
- ↑ NICE Rheumatoid arthritis in Adults:Management Available from:https://www.nice.org.uk/guidance/ng100/chapter/Recommendations (last accessed 20.3.2020)