Tendon Anatomy
Basic Anatomy and Physiology of a Tendon [edit | edit source]
Tendons are situated between bone and muscles and are bright white in colour, their fibro-elastic composition gives them the strength require to transmit large mechanical forces. Each muscle has two tendons, one proximally and one distally. The point at which the tendon forms attachment to the muscle is also known as the musculotendinous junction (MTJ) and the point at which it attaches to the bone is known as the osteotendinous junction (OTJ). The purpose of the tendon is to transmit forces generated from the muscle to the bone to elicit movement. The proximal attachment of the tendon is also known as the origin and the distal tendon is called the insertion.[1]
Tendons have different shapes and sizes depending on the role of the muscle. Muscles that generate a lot of power and force tend to have shorter and wider tendons than those that perform more fine delicate movements. These tend to be long and thin. [2]
Cellular Component of a Tendon [edit | edit source]
The tendon cells are known as tenoblasts and tenocytes. They make up approximately 90-95% of the cells within the tendon. The other 5-10% include the chondrocyctes, synovial cells and the vascular cells.[1]
Tenoblasts are immature tendon cells. Initially they are different in size and shape but as they age they become elongated and spindle shaped and transform into tenocytes. The tenocyctes are responsible for the turnover of maintenance of the extracellular matrix (described below). The tenocyctes respond to mechanical load of the tendon and thus make adaptations. They are arranged in longitudinal rows and have extensive communication with adjacent cells usually through gap junctions.[1][3]
Gap junctions are very complex and complicated structures. They have two hemi-channels. These are also called connexons (a collection of six connexin protein subunits). These have a central pore. The connexons in an open state allow metabolites and ions to pass freely between the gap junctions. The connexins are numbered, the ones which we are interested in for cell communication and tendon regeneration are connexins 26, 32 and 43.[4][5][6]
Connexin 43 is situated in gap junctions between cells in rows along the collagen fibres. Connexins 26 and 32 have a more diffuse pattern. Connexin 43 is responsible for the inhibition of the collagen syntheses within the tenocyctes as a response to mechanical loading. Connexin 32 may have a stimulatory role, but all we need to know is that they aid communication between cells within the tendon to help with regeneration and adaptation. [7]
Extracellular Matrix Structure[edit | edit source]
Tendons consist of mainly type 1 collagen fibres (but there are others present) and proteoglycan. The type 1 collagen fibres are responsible for the tensile strength of the tendon whereas the proteoglycan are responsible for the viscoelastic nature of the tendon.
The orientation of the collagen fibres in tendons have been found to run; parallel, simply crossing, crossing of two fibres with one straight, a plait formation of three fibres and an up typing of two parallel running fibres. The orientation and organisation of collagen fibres differs from tendon to tendon and vary in location of the tendon. This is dependent on the requirement of each tendon. For example tendons that need to resist rotational tensile forces will have a collagen fibre orientation to enable this. [8]
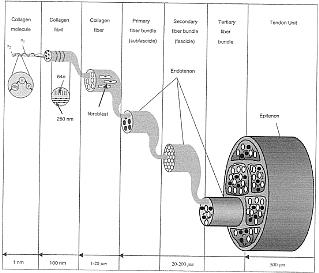
The collagen molecules consist of polypeptide chains, three of these chains combined together form a densely packed helical tropocollagen molecule. Five of these combined together form a microfibril. The microfibrils then aggregate together to form fibrils. These are then grouped into fibres and fibres into fibre bundles and then into fascicles.
The fascicles are small in diameter in the young but as they mature into you adulthood they grow in size, peaking in size between the ages of 20-29 years old. As the tendon progressively ages the diameter becomes smaller, this has been linked to a possibility in the decreased strength of the muscle. It has also been noted that the diameter can shrink in size if the tendon becomes injured. [2][9]
Vascularity [edit | edit source]
Vascularity of a tendon is very important when considering the healing process. Blood supply from tendons can be split into two sources; the intrinsic and the extrinsic. The intrinic sources are at the MJT and thr OTJ, while the extinsic are at through the paratenon or the synovial sheath.The blood supply to specific areas are supplied by different sources. The intrinsic at the MTJ has been doucmented to extend into 1/3 of the tendon whereas the bloody supply originating from the OTJ is more avascular and is limited to the insertional point. This leave the extrinsic source to supply the mid portion of the tendon. [10]
Studies have shown that tendons have significantly reduced vascularity around bony pulleys. A connection has been made between tendons that can be compressed at multiple locations (between the MTJ and the enthesis) and common sites of degeneration and / or rupture. [11]
Innervation[edit | edit source]
The innervation of tendons start from cutaneous, peritendinous and muscular nerves. At the MTJ nerve fibres cross and entre the endotenon and the paratenon. These fibres then enter and innervate the epitenon. The majority of the nerve fibres terminate and reside on the surface of the tendon. The nerve endings can be categorised into myelinated and unmyelinated. The myelinated nerver fibers are specialised mechanoreceptors (Golgi tendon organs) sensing tension and pressure in the tendon. These tend to be located close to the muscle. The unmyelinated fibres are responsible for sensing and transmitting pain (nocioceptors). [12][13]
The surrounding Structure[edit | edit source]
The structures surrounding the tendon can be split into 5 subcategories. The main aim of these structures is to reduce friction and enable the tendon to glide smoothly. This is an important factor for ensuring the transitions of the force is at its most efficient. These structures are:
- The retinaculum / fibrous sheaths
- The reflection pulleys
- The synovial sheaths
- The peritendinous sheet (paratenon)
- The tendon bursae[1]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Kannus P. Structure of the tendon connective tissue. Scandinavian Journal of Medicine & Science in Sports. 2000; 10: 312-320. Cite error: Invalid
<ref>tag; name "Kannus 2000" defined multiple times with different content Cite error: Invalid<ref>tag; name "Kannus 2000" defined multiple times with different content Cite error: Invalid<ref>tag; name "Kannus 2000" defined multiple times with different content - ↑ 2.0 2.1 Benjamin M, kaiser E, Milz. Structure-function relationships in tendons: a review. Journal of Anatomy 2008; 212: 211-228
- ↑ Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. Journal of Musculoskeletal Neuronal Interact. 2006; 6 (2): 181-190.
- ↑ Maeda E, Shangjun Y, Wang W, Bader DL, Knight MM, Lee DA. Gap junction permability between tenocytes within tendon fasciles is supported by tensile loading. Journal of Biomechinical Model Mechanobiol 2012; 11:439-447
- ↑ Goldberg GS, Lampe PD, Nicholson BJ. Selective transfer of endogenous metabolites through gap junctions composed of different connexins. Nature Cell Biology 1999; 1:457–459.
- ↑ Wagett AD, Benjamin M, Ralphs JR. Connexin 32 and 43 gap junctions differentially modulate tenocyte response to cyclic mechanical load. European Journal of Cell Biology 2006 85:1145–1154
- ↑ Banes AJ, Weinhold P, Yang X, Tsuzaki M, Bynum D, Bottlang M, Brown T. Gap junctions regulate responses of tendon cells ex vivo to mechanical loading. Clinical Orthopaedics and Related Research 1999; 367:356–370
- ↑ Thomopoulos S, Marquez JP, Weinburger B, Birman V, Genin G. Collagen fiber orientation at the tendon to bone insertion and its influence on stress concentrations. Journal of Biomechanics 2006; 39(10):1842–1851.
- ↑ Sharma P, Maffulli N. Biology of tendon injury: healing, modeling and remodeling. Journal of Musculoskeletal Neuronal Interact. 2006; 6 (2): 181-190.
- ↑ Carr AJ, Norris SH. The blood supply of the calcanealfckLRtendon. Journal of Bone Joint Surgery 1989; 71:100-101
- ↑ Petersen W, Pufe T, Kurz B, Mentlein R, Tillmann B.fckLRAngiogenesis in fetal tendon development: spatial and temporal expression of the angiogenic peptide vascular endothelial cell growth factor. Anatomy and Embryology 2002; 205: 263–270.
- ↑ Lephart SM, Pincivero DM, Giraldo JL, Fu FH. ThefckLRrole of proprioception in the management and rehabilitation of athletic injuries. American Journal of Sports Medicine 1997; 25:130-137.
- ↑ Ackermann PW, Li J, Finn A, Ahmed M, Kreicbergs A. Autonomic innervation of tendons, ligaments and jointfckLRcapsules. A morphologic and quantitative study in thefckLRrat. Journal of Orthopaedic Research 2001; 19:372-378.