Hyperparathyroidism: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Hyperparathyroidism effects not only the endocrine system but also the central nervous system (CNS), musculoskeletal system, gastrointestinal (GI), and the gastrourinary system (GU). 2 | Hyperparathyroidism effects not only the endocrine system but also the central nervous system (CNS), musculoskeletal system, gastrointestinal (GI), and the gastrourinary system (GU). <ref name="2" /> | ||
Individuals with this disorder commonly exhibit muscle weakness and fatigue. Other symptoms associated with hyperparathyroidism include: | Individuals with this disorder commonly exhibit muscle weakness and fatigue. Other symptoms associated with hyperparathyroidism include: | ||
· Loss of appetite 2 | · Loss of appetite <ref name="2" /> | ||
· | · Lethargy<ref name="1" /> | ||
· | · Drowsiness<ref name="1" /> | ||
· Weight | · Weight loss<ref name="2" /> | ||
· Nausea and | · Nausea and vomiting<ref name="2" /> | ||
· | · Depression<ref name="2" /> | ||
· Increased thirst and urination 2 | · Increased thirst and urination <ref name="2" /> | ||
· Kidney stones5 | · Kidney stones5 | ||
| Line 42: | Line 42: | ||
· Fragile bones that easily fracture (osteoporosis)5 | · Fragile bones that easily fracture (osteoporosis)5 | ||
· GI | · GI problems<ref name="2" /> | ||
· | · Pancreatitis<ref name="2" /> | ||
· Bone decalcification (hypercalcemia)2 | · Bone decalcification (hypercalcemia)<ref name="2" /> | ||
· Psychotic | · Psychotic paranoia<ref name="2" /> | ||
· Frequent complaints of illness with no apparent cause5 | · Frequent complaints of illness with no apparent cause5 | ||
· | · Paresthesias<ref name="1" /> | ||
· Hyperactive deep tendon | · Hyperactive deep tendon reflexes<ref name="1" /> | ||
· Personality | · Personality changes<ref name="1" /> | ||
· Muscle weakness and | · Muscle weakness and atrophy<ref name="1" /> | ||
· | · Gout<ref name="1" /> | ||
· | · Myalgia<ref name="1" /> | ||
· Abdominal | · Abdominal pain<ref name="1" /> | ||
· | · Constipation<ref name="1" /> | ||
· Peptic | · Peptic ulcers<ref name="1" /> | ||
· Renal | · Renal colic<ref name="1" /> | ||
· Hyper- | · Hyper-calcemia<ref name="1" /> | ||
· Kidney | · Kidney infections<ref name="1" /> | ||
· Renal | · Renal hypertension<ref name="1" /> | ||
<br><br> | <br><br> | ||
== Associated Co-morbidities<br> == | == Associated Co-morbidities<br> == | ||
Revision as of 16:56, 20 March 2014
Original Editors - Suzette Austin & Erica Jezke from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Suzette Austin, Erica Jeszke, Lucinda hampton, Elaine Lonnemann, WikiSysop, 127.0.0.1, Kim Jackson and Admin
Definition/Description
[edit | edit source]
“Hyperparathyroidism is a disorder caused by overactivity of one or more of the four parathyroid glands that disrupts calcium, phosphate, and bone metabolism.” Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive titleThe parathyroid glands are located in the neck on the posterior surface of each lobe of the thyroid gland. [2,5] Each of the four parathyroid glands is about the size of a grain of rice.5 As part of the endocrine system, these glands secrete parathyroid hormone (PTH), which regulates calcium and phosphorus. Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Hyperparathyroidism is classified into three groups: primary, secondary, or tertiary.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Primary hyperparathyroidism develops when there is an imbalance between serum calcium levels and PTH secretion.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Secondary hyperparathyroidism occurs when the glands have become enlarged due to malfunction of another organ system.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Tertiary hyperparathyroidism is seen in dialysis clients who have chronic secondary hyperparathyroidism.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Prevalence
[edit | edit source]
Hyperparathyroidism is most prevalent in postmenopausal women over the age of 60.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title Incidence of hyperparathyroidism is about equal in men and women under the age of 50. Incidence increases with age and female gender.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The occurrence of hyperparathyroidism is highest among blacks followed by whites.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title The condition is less prevalent in asians, hispanics, and other races.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Characteristics/Clinical Presentation[edit | edit source]
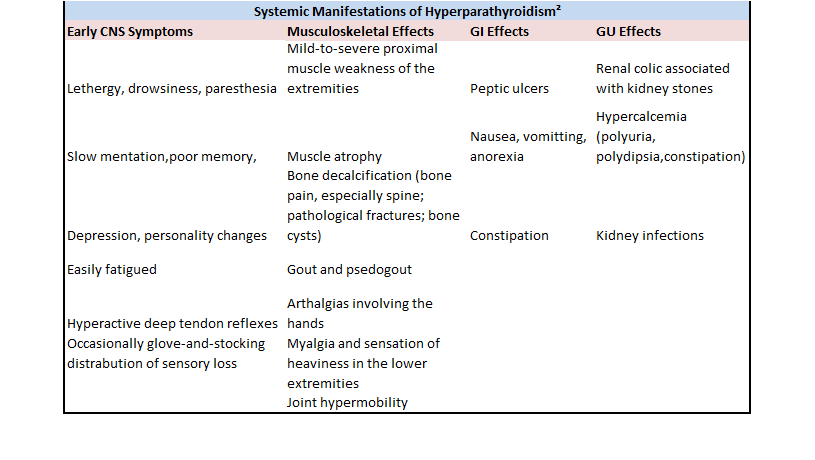
Hyperparathyroidism effects not only the endocrine system but also the central nervous system (CNS), musculoskeletal system, gastrointestinal (GI), and the gastrourinary system (GU). Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Individuals with this disorder commonly exhibit muscle weakness and fatigue. Other symptoms associated with hyperparathyroidism include:
· Loss of appetite Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· LethargyCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· DrowsinessCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Weight lossCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Nausea and vomitingCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· DepressionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Increased thirst and urination Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Kidney stones5
· Bone and joint pain5
· Fragile bones that easily fracture (osteoporosis)5
· GI problemsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· PancreatitisCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Bone decalcification (hypercalcemia)Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Psychotic paranoiaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Frequent complaints of illness with no apparent cause5
· ParesthesiasCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Hyperactive deep tendon reflexesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Personality changesCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Muscle weakness and atrophyCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· GoutCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· MyalgiaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Abdominal painCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· ConstipationCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Peptic ulcersCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Renal colicCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Hyper-calcemiaCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Kidney infectionsCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
· Renal hypertensionCite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Associated Co-morbidities
[edit | edit source]
Patients with mild PHPT had a significantly increased risk of developing cardiovascular, cerebrovascular disease, renal dysfunction and fractures.4 Additional co-morbidities include:
- Osteogenisis Imperfecta 1
- Paget’s Disease1
- Multiple myeloma1
- Carcinoma1
- Vitamin D deficiency1
- Bone damage1
- Hypocalcaemia 1
- Kidney damage
Medications[edit | edit source]
Medications to treat hyperparathyroidism include:
Calcimimetics. Calcimimetics mimic calcium circulating in the blood and may trick the parathyroid glands into releasing less parathyroid hormone. It may be prescribed to treat primary hyperparathyroidism, particularly if surgery hasn't successfully cured the disorder or a person isn't a good candidate for surgery.
Hormone replacement therapy. Hormone replacement therapy (HRT) does not address the underlying causes of excess PTH but helps to prevent bone from demineralizing as a result of excess PTH in the blood. HRT is used for menopausal women or for individuals who are exhibiting signs of osteoporosis. Estrogen and progestin are commonly used in combination for this treatment option.
Bisphosphonates- Bisphosphonates prevents the loss of calcium from bones decreasing the risk for development of osteoporosis which is caused by hyperparathyroidism.
Calcitonin- Calcitonin is used in the treatment of osteoporosis.8 It binds to osteoclasts and inhibits their action, helping to prevent the breakdown of bone.8
Diagnostic Tests/Lab Tests/Lab Values[edit | edit source]
Diagnostic tests/Labs:6
· Blood tests are used to indicate how much calcium, PTH and phosphorus are in the blood. If an elevated amount of any of these is found in the blood it may be indicative of overactivity of the parathyroid glands.
Other tests once diagnosis has been made:
o Bone mineral density test (bone densitometry). Dual energy X-ray absorptiometry, or a DXA scan, is commonly used to measure bone mineral density. This test measures how many grams of calcium and other minerals are packed into a segment of bone.
o Urine tests. A 24-hour collection of urine can be used to measure kidney function and how much calcium is expelled in urine. This test may help in determining if kidney dysfunction or parathyroid disorder is the primary cause of bone demineralization.
o Imaging tests of kidneys. Used to determine presence of kidney stones or other kidney abnormalities.
Etiology/Causes[edit | edit source]
“The most common cause of primary hyperparathyroidism is a single adenoma of the parathyroid gland.”1
Systemic Involvement[edit | edit source]
Medical Management (current best evidence)[edit | edit source]
Treatment for primary hyperparathyroidism is surgical removal of affected parathyroid gland, management of any bone or organ damage, and use of medication to protect bones prior to surgery or when parathyroidectomy is not an option. 1
Physical Therapy Management (current best evidence)[edit | edit source]
Therapists may observe skeletal, articular and neuromuscular impairments associated with hyperparathyroidism. 7 In the acute phase, therapists should exercise caution with patients as they are at an increased risk for bone fracture.1 After surgery, patients should be encouraged to ambulate as soon as possible to prevent further demineralization.1 Encourage and aid patients in setting up their homes to avoid or minimize fall risks.1
Alternative/Holistic Management (current best evidence)[edit | edit source]
Eating a healthy and well balanced natural diet, avoiding coffee, tea, alcohol, tobacco, and carbonated beverages, exercising regularly, and drinking plenty of water may help to reduce the symptoms of hyperparathyroidism.9 Some herbal supplements have been used for the treatment of hyperparathyroidism including chaste tree and dandelion. 9 Some holistic medical practitioners also treat hyperparathyroidism.9 Vitamin supplements including calcium, vitamin D, Ipriflavone (soy isoflavones) standardized extract and Omega-3 fatty acids have been used to help treat this disorder.9 Alternative treatments for hyperparathyroidism have not been proven effective for the management of hyperparathyroidism. Alternative/holistic treatment options should be discussed with a qualified healthcare practitioner prior to initiation.
Differential Diagnosis[edit | edit source]
Differential Diagnosis10
Adrenal insufficiency
Certain malignant tumors or myelomas
Excessive calcium or vitamin D ingestion
Familial hypocalciuric hypercalcemia
Hyperthyroidism
Malnutrition
Case Reports/ Case Studies[edit | edit source]
A patient with persistent primary hyperparathyroidism due to a second ectopic adenoma.11
A 33 year old woman was diagnosed with hyperparathyroidism and treated with parathyroidectomy. Post-operatively the patient’s serum calcium and PTH levels decreased but did not normalize and continued to present with kidney stones.
Diplopia associated with hyperparathyroidism: report of a case.12
A 60 year old man presented with diplopia as well as common symptoms of hyperparathyroidism. He was diagnosed with primary hyperparathyroidism and a search for the cause of the diplopia continued. After undergoing thyroidectomy his double vision was relieved as his serum calcium levels returned to normal.
Primary hyperparathyroidism presenting as recurrent acute pancreatitis: A case report and review of literature13
A 32 year old man presents with repetitive episodes of pancreatitis. Patient was treated by parathyroidectomy and recurrence of abdominal pain ceased and serum calcium levels normalized.
Resources
[edit | edit source]
add appropriate resources here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: addfeedhere|charset=UTF-8|short|max=10<div class="researchbox"><rss>Feed goes here!!|charset=UTF-8|short|max=10</rss></div>