Otitis Media: Difference between revisions
Mohit Chand (talk | contribs) No edit summary |
Mohit Chand (talk | contribs) No edit summary |
||
| Line 65: | Line 65: | ||
* Irritability | * Irritability | ||
* Headache | * [[Headache]] | ||
* Disturbed or restless sleep | * Disturbed or restless sleep | ||
* Poor feeding or anorexia | * Poor feeding or anorexia | ||
Revision as of 14:39, 26 November 2023
Introduction[edit | edit source]
Otitis media refers to inflammation or infection of the middle ear, a common condition that can affect individuals of all ages, with a higher incidence in children.
It is a spectrum of diseases that includes:[1]
- Acute otitis media (AOM): A sudden onset of infection or inflammation in the middle ear.
- Chronic suppurative otitis media (CSOM): Persistent or recurrent inflammation or infection of the middle ear.
- Otitis media with effusion (OME): Fluid accumulation in the middle ear without active infection.
It is prevalent in all age groups, with a higher incidence in children, particularly between 6 to 24 months. This article explores the spectrum of otitis media, its etiology, epidemiology, pathophysiology, clinical features, diagnosis, and treatment modalities.[2]
Etiology[edit | edit source]
Otitis media is a complex condition that results from various factors such as infections, allergies, and environmental elements. Causes and risk factors of Otitis Media:
Infectious Agents:[edit | edit source]
Bacterial Pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis are major contributors.
Viral Pathogens: Respiratory syncytial virus, influenza virus, parainfluenza virus, rhinovirus, adenovirus.[3]
Immune System Factors:[edit | edit source]
Decreased immunity due to conditions like HIV, diabetes, and other immune deficiencies.
Genetic Predisposition:[edit | edit source]
Ethnicity: Children who are Native American, Hispanic and Alaska Natives have more ear infections than children of other ethnic groups.
Certain genetic factors may increase susceptibility to otitis media.[4]
Anatomic Abnormalities:[edit | edit source]
Abnormalities of the palate and tensor veli palatini.
Ciliary dysfunction.
Environmental Factors:[edit | edit source]
Passive Smoke Exposure: Especially in children.[5]
Cochlear Implants:[edit | edit source]
Individuals with cochlear implants may be at an increased risk.[8]
Other Factors:[edit | edit source]
Vitamin A deficiency.
Daycare attendance.
Lower socioeconomic status.
Family history of recurrent AOM.[9]
Epidemiology[edit | edit source]
Otitis media is a prevalent issue, with a slightly higher incidence in males than females. It is most common between the ages of six and twelve months and decreases after the age of five. [10]
It's a well-known fact that a significant number of children suffer from otitis media at least once in their lifetime. In fact, statistics show that around 80% of children are affected by it. Additionally, between 80% and 90% of all children experience otitis media with an effusion before they even start school. Although otitis media is less prevalent in adults, some sub-populations are still at risk. For instance, people who have a history of recurrent OM in childhood, cleft palate, immunodeficiency, or immunocompromised status are more susceptible to this condition.[11]
Pathophysiology[edit | edit source]
AOM is not always preceded by a viral upper respiratory tract infection that also affects the mucosa of the nose, nasopharynx, and Eustachian tubes.[12]
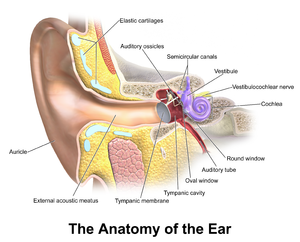
Infection of the middle ear results from nasopharyngeal organisms migrating via the eustachian tube. The anatomy of the eustachian tube in younger children is immature, typically being short, straight, wide (only becoming more oblique as the child grows), meaning infection blocks the narrow section of the Eustachian tube. This blockage reduces ventilation, increasing negative pressure and the release of exudate from the irritated mucosa takes place. Due to the presence of the exudate, the bacterial and viral organisms thrive, leading to suppuration and the presence of pus in the middle ear[13][14]
Clinical Features[edit | edit source]
Signs and symptoms of ear infection in children may include:
- Irritability
- Headache
- Disturbed or restless sleep
- Poor feeding or anorexia
- Vomiting
- Diarrhea
- Pulling or tugging at the ears.
- About two-thirds of patients may also have a low-grade fever.[15]
The American Academy of Pediatrics has established guidelines for diagnosing acute otitis media, which involve the presence of moderate to severe bulging of the tympanic membrane or new onset of otorrhea (ear pain) not caused by otitis externa, or mild tympanic membrane bulging with recent onset of ear pain or erythema. These criteria are meant to assist primary care clinicians in making accurate diagnoses and informed clinical decisions, but not to replace their clinical judgment.[16]
On otoscopy, the tympanic membrane (TM) looks erythematous and may be bulging. If this fluid pressure has perforated the TM, small tear are visible with purulent discharge in the auditory canal. Patients may have a conductive hearing loss or a cervical lymphadenopathy.
It is important to test and document the function of the facial nerve (due to its anatomical course through the middle ear). Examination should also include checking for any intracranial complications, cervical lymphadenopathy, and signs of infection in the throat and oral cavity.
Diagnosis[edit | edit source]
The diagnosis of otitis media relies on a detailed medical history, a thorough physical examination, and specific diagnostic procedures. Professionals use an otoscope to visually inspect the external ear canal and tympanic membrane for signs like redness, bulging, or fluid accumulation. Tympanometry measures eardrum mobility, aiding in the assessment of middle ear fluid. In some cases, hearing tests (audiometry) may be conducted.
Laboratory tests, including tympanocentesis for fluid analysis, can be performed in certain situations. Imaging studies like CT or MRI are reserved for cases with suspected complications. Diagnostic criteria often involve established guidelines, such as those from the American Academy of Pediatrics.
Overall, otoscopy remains a primary diagnostic tool.
Treatment / Management[edit | edit source]
When acute otitis media is diagnosed, the primary goal of treatment is to relieve pain and address the underlying infection with antibiotics.
To relieve pain, non-steroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can be used. The use of antibiotics to treat otitis media early on is a controversial issue and varies based on the guidelines of the country.[17]However, there is evidence of oral antibiotics in suppurative AOM.
In cases of tympanic membrane perforation, ototopical antibiotics like ofloxacin may be preferred. Systemic steroids and antihistamines generally do not yield significant benefits. For recurrent instances, especially in children, consideration may be given to myringotomy with tube placement (tympanostomy tube) to enhance middle ear ventilation and reduce reliance on systemic antibiotics. Decision-making should align with established guidelines and clinical judgment.
Resources[edit | edit source]
American Academy of Pediatrics
References[edit | edit source]
- ↑ Rettig, E., & Tunkel, D. E. (2014). Contemporary Concepts in Management of Acute Otitis Media in Children. Otolaryngologic Clinics of North America, 47(5), 651. https://doi.org/10.1016/j.otc.2014.06.006
- ↑ Meherali, S., Campbell, A., Hartling, L., & Scott, S. (2019). Understanding Parents’ Experiences and Information Needs on Pediatric Acute Otitis Media: A Qualitative Study. Journal of Patient Experience, 6(1), 53-61. https://doi.org/10.1177/2374373518771362
- ↑ Seppälä E, Sillanpää S, Nurminen N, Huhtala H, Toppari J, Ilonen J, Veijola R, Knip M, Sipilä M, Laranne J, Oikarinen S, Hyöty H. Human enterovirus and rhinovirus infections are associated with otitis media in a prospective birth cohort study. J Clin Virol. 2016 Dec;85:1-6. doi: 10.1016/j.jcv.2016.10.010. Epub 2016 Oct 20. PMID: 27780081.
- ↑ Mittal R, Robalino G, Gerring R, Chan B, Yan D, Grati M, Liu XZ. Immunity genes and susceptibility to otitis media: a comprehensive review. J Genet Genomics. 2014 Nov 20;41(11):567-81. doi: 10.1016/j.jgg.2014.10.003. Epub 2014 Oct 31. PMID: 25434680.
- ↑ Strachan, D. P., & Cook, D. G. (1997). Health effects of passive smoking. 4. Parental smoking, middle ear disease and adenotonsillectomy in children. Thorax, 53(1), 50-56. https://doi.org/10.1136/thx.53.1.50
- ↑ Ardiç C, Yavuz E. Effect of breastfeeding on common pediatric infections: a 5-year prospective cohort study. Arch Argent Pediatr. 2018 Apr 1;116(2):126-132. English, Spanish. doi: 10.5546/aap.2018.eng.126. PMID: 29557599.
- ↑ Ardiç C, Yavuz E. Effect of breastfeeding on common pediatric infections: a 5-year prospective cohort study. Arch Argent Pediatr. 2018 Apr 1;116(2):126-132. English, Spanish. doi: 10.5546/aap.2018.eng.126. PMID: 29557599.
- ↑ Vila, P. M., Ghogomu, N. T., Odom-John, A. R., Hullar, T. E., & Hirose, K. (2017). Infectious complications of pediatric cochlear implants are highly influenced by otitis media. International Journal of Pediatric Otorhinolaryngology, 97, 76. https://doi.org/10.1016/j.ijporl.2017.02.026
- ↑ Kraemer MJ, Richardson MA, Weiss NS, Furukawa CT, Shapiro GG, Pierson WE, Bierman CW. Risk factors for persistent middle-ear effusions. Otitis media, catarrh, cigarette smoke exposure, and atopy. JAMA. 1983 Feb 25;249(8):1022-5. PMID: 6681641.
- ↑ Usonis V, Jackowska T, Petraitiene S, Sapala A, Neculau A, Stryjewska I, Devadiga R, Tafalla M, Holl K. Incidence of acute otitis media in children below 6 years of age seen in medical practices in five East European countries. BMC Pediatr. 2016 Jul 26;16:108. doi: 10.1186/s12887-016-0638-2. PMID: 27457584; PMCID: PMC4960887.
- ↑ M. Schilder, A. G., Chonmaitree, T., Cripps, A. W., Rosenfeld, R. M., Casselbrant, M. L., Haggard, M. P., & Venekamp, R. P. (2016). Otitis media. Nature Reviews. Disease Primers, 2(1). https://doi.org/10.1038/nrdp.2016.63
- ↑ Winther B, Alper CM, Mandel EM, Doyle WJ, Hendley JO. Temporal relationships between colds, upper respiratory viruses detected by polymerase chain reaction, and otitis media in young children followed through a typical cold season. Pediatrics. 2007 Jun;119(6):1069-75. doi: 10.1542/peds.2006-3294. PMID: 17545372.
- ↑ Fireman P. Otitis media and eustachian tube dysfunction: connection to allergic rhinitis. J Allergy Clin Immunol. 1997 Feb;99(2):S787-97. doi: 10.1016/s0091-6749(97)70130-1. PMID: 9042072.
- ↑ Fireman P. Eustachian tube obstruction and allergy: a role in otitis media with effusion? J Allergy Clin Immunol. 1985 Aug;76(2 Pt 1):137-40. doi: 10.1016/0091-6749(85)90690-6. PMID: 4019946.
- ↑ Kontiokari T, Koivunen P, Niemelä M, Pokka T, Uhari M. Symptoms of acute otitis media. Pediatr Infect Dis J. 1998 Aug;17(8):676-9. doi: 10.1097/00006454-199808000-00003. PMID: 9726339.
- ↑ Siddiq S, Grainger J. The diagnosis and management of acute otitis media: American Academy of Pediatrics Guidelines 2013. Arch Dis Child Educ Pract Ed. 2015 Aug;100(4):193-7. doi: 10.1136/archdischild-2013-305550. Epub 2014 Nov 12. PMID: 25395494.
- ↑ Rettig E, Tunkel DE. Contemporary concepts in management of acute otitis media in children. Otolaryngol Clin North Am. 2014 Oct;47(5):651-72. doi: 10.1016/j.otc.2014.06.006. Epub 2014 Aug 1. PMID: 25213276; PMCID: PMC4393005.