Hypermobile Meniscus: Difference between revisions
No edit summary |
(Added photo) |
||
| Line 20: | Line 20: | ||
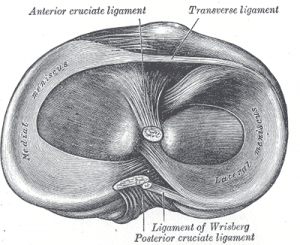
The menisci are crescent shaped, cartilaginous discs that lie between the articular cartilage of the femur and tibia. The menisci have various functions - load transmission, shock absorption, joint lubrication, nutrition, secondary mechanical stability, and guiding of movements.<ref>Habegger A. The Knee. 2023 Mar.</ref>[[File:Meniscus sup view Gray349.png|center|thumb|Caudal view of right knee|alt=]] | The menisci are crescent shaped, cartilaginous discs that lie between the articular cartilage of the femur and tibia. The menisci have various functions - load transmission, shock absorption, joint lubrication, nutrition, secondary mechanical stability, and guiding of movements.<ref>Habegger A. The Knee. 2023 Mar.</ref>[[File:Meniscus sup view Gray349.png|center|thumb|Caudal view of right knee|alt=]] | ||
<br>In a stable knee, the LM is smaller, thinner, and more mobile than the medial meniscus. In addition, the lateral meniscus has less stabilizers at its posterolateral aspect.<ref name=":0" /> The stabilizers of the lateral meniscus include the – popliteomeniscal fascicles (PMF), the posterior capsule, the meniscofemoral ligaments, and the posterior meniscotibial ligament. <ref name=":0" /> These attachments to the posterior knee prevent the subluxation of the posterior horn of the lateral meniscus into the knee joint. <ref name=":2">McHugh C. Hypermobile lateral Meniscus [Internet]. Orthosports. 2022 [cited 2023 Mar 28]. Available from: <nowiki>https://orthosports.com.au/hypermobile_lateral_meniscus</nowiki></ref> | <br>In a stable knee, the LM is smaller, thinner, and more mobile than the medial meniscus. In addition, the lateral meniscus has less stabilizers at its posterolateral aspect.<ref name=":0" /> The stabilizers of the lateral meniscus include the – popliteomeniscal fascicles (PMF), the posterior capsule, the meniscofemoral ligaments, and the posterior meniscotibial ligament. <ref name=":0" /> These attachments to the posterior knee prevent the subluxation of the posterior horn of the lateral meniscus into the knee joint. <ref name=":2">McHugh C. Hypermobile lateral Meniscus [Internet]. Orthosports. 2022 [cited 2023 Mar 28]. Available from: <nowiki>https://orthosports.com.au/hypermobile_lateral_meniscus</nowiki></ref> | ||
[[File:60B33236-0507-48AD-A47A-3EC0C5BFFA5F.jpeg|thumb|435x435px|Posterior ligamentous structures of the knee]] | |||
== Mechanism of Injury / Pathological Process<br> == | == Mechanism of Injury / Pathological Process<br> == | ||
Revision as of 16:31, 28 March 2023
Top Contributors - Robert Pierce, Madisyn Melchor, Kim Jackson, Matt Huey, Cindy John-Chu and Briana Marin
Top Contributors - Robert Pierce, Madisyn Melchor, Kim Jackson, Matt Huey, Cindy John-Chu and Briana Marin
Clinically Relevant Anatomy
[edit | edit source]
Lateral meniscus hypermobility (LMH) is excess motion at the lateral meniscus (LM) that can cause lateral knee pain or tenderness, locking of the knee, or limitation of the range of motion during knee flexion. [1][2] It is a rare, uncommon condition. [1]
The menisci are crescent shaped, cartilaginous discs that lie between the articular cartilage of the femur and tibia. The menisci have various functions - load transmission, shock absorption, joint lubrication, nutrition, secondary mechanical stability, and guiding of movements.[3]
In a stable knee, the LM is smaller, thinner, and more mobile than the medial meniscus. In addition, the lateral meniscus has less stabilizers at its posterolateral aspect.[1] The stabilizers of the lateral meniscus include the – popliteomeniscal fascicles (PMF), the posterior capsule, the meniscofemoral ligaments, and the posterior meniscotibial ligament. [1] These attachments to the posterior knee prevent the subluxation of the posterior horn of the lateral meniscus into the knee joint. [4]
Mechanism of Injury / Pathological Process
[edit | edit source]
LMH is thought to be related to a congenital deficiency in the capsular attachments[5], or an atraumatic injury to the ligamentous attachments[4], specifically the PMF [2]. Trauma that causes rupture to the PMF can be insignificant, so patients may not recall a specific mechanism of injury.
Commonly, hypermobility is due to an overuse injury, as well as atraumatic hypermobility. An isolated incidence of LMH is rare. Studies have found that in many cases of anterior cruciate ligament (ACL), and/or posterolateral injuries to the knee there is concurrent damage to the PMF, which may result in LMH.
Clinical Presentation[edit | edit source]
Symptoms include painful popping or locking with the knee in flexion and/or external rotation. Pain can be reproduced through application of a varus force when the hip and knee are placed in flexion and external rotation (FABER).
Diagnostic Procedures[edit | edit source]
Arthroscopy is considered the gold standard of diagnosing LMH. If 50% of the LM crosses anterior to the midline of the tibial plateau, an LMH diagnosis is confirmed. This is called a Gutter's Sign and is present in 95.5% of patients with LMH. To determine the level of hypermobility of the LM, an arthroscopic procedure is conducted to test for a Gutter's Sign - a probed hooked behind the posterior lateral meniscus with anterior pressure to cause translation of the LM beyond the tibial articular surface. (Steyn)
Two main techniques to stabilize the LM is to suture the tissue to the anterior popliteomeniscal fascicle or fasten the LM to the posterior capsule of the knee. (Beel)
An MRI will show no abnormalities, but if an MRI is taken during the “locked” phase, you may see the posterior aspect of the LM anterior to the midline of the tibial plateau. This is indicative of LMH.
Outcome Measures[edit | edit source]
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
· Bucket-handle Meniscal Lesion
· Anterior Cruciate Ligament (ACL Tear)
· Ligamentous Instabilities
· Articular Cartilage lesions
· Patellar Dislocation
· Patellar Pathology
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1. Beel W, Macchiarola L, Mouton C, Laver L, Seil R. The hypermobile and unstable lateral meniscus: a narrative review of the anatomy, biomechanics, diagnosis and treatment options. Ann Jt [Internet]. 2022;7:14–14. Available from: http://dx.doi.org/10.21037/aoj-21-9
- ↑ 2.0 2.1 4. Kamiya T, Suzuki T, Otsubo H, Kuroda M, Matsumura T, Kubota C, et al. Midterm outcomes after arthroscopic surgery for hypermobile lateral meniscus in adults: Restriction of paradoxical motion. J Orthop Sci [Internet]. 2018;23(6):1000–4. Available from: http://dx.doi.org/10.1016/j.jos.2018.06.003
- ↑ Habegger A. The Knee. 2023 Mar.
- ↑ 4.0 4.1 McHugh C. Hypermobile lateral Meniscus [Internet]. Orthosports. 2022 [cited 2023 Mar 28]. Available from: https://orthosports.com.au/hypermobile_lateral_meniscus
- ↑ Van Steyn MO, Mariscalco MW, Pedroza AD, Smerek J, Kaeding CC, Flanigan DC. The hypermobile lateral meniscus: a retrospective review of presentation, imaging, treatment, and results. Knee Surg Sports Traumatol Arthrosc [Internet]. 2016;24(5):1555–9. Available from: http://dx.doi.org/10.1007/s00167-014-3497-0