Obstetric Fistula: Difference between revisions
Rosie Swift (talk | contribs) No edit summary |
Rosie Swift (talk | contribs) No edit summary |
||
| Line 3: | Line 3: | ||
</div> | </div> | ||
<div class="editorbox"> '''Original Editor '''- [[ | <div class="editorbox"> '''Original Editor '''- [[User:User Name|User Name]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
Revision as of 05:31, 20 November 2021
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (20/11/2021)
Top Contributors - Rosie Swift and Kim Jackson
Description[edit | edit source]
- Obstetric fistula is an abnormal opening between a woman’s genital tract and her urinary tract or rectum causing urinary and faecal incontinence, ongoing genital infections, anaemia and neurological symptoms of the lower limb[1].
- It is caused by prolonged obstructed labour. The child is often stillborn and there is a risk to future fertility if cervical damage has occurred[2].
- Unsurprisingly, this highly stigmatizing condition has a significant impact on mental health as well as social and conjugal relations[3].
- It is estimated that each year between 50 000 to 100 000 women worldwide are affected by obstetric fistula and that more than 2 million young women live with untreated obstetric fistula in Asia and sub-Saharan Africa[4]
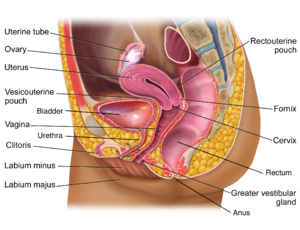
Clinically Relevant Anatomy
[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
Aetiology[edit | edit source]
Most common cause: Prolonged, obstructed labour (labour for 2 or 3 days)[5]
Could be avoided by:
delaying the age of first pregnancy,
cessation of harmful traditional practices
timely access to maternal and obstetric care (three delays - decision, journey, receiving appropriate skilled care)
Other (less common) causes:exual abuse and rape, the complications of unsafe abortions and surgical trauma (most commonly, injury to the bladder at caesarean section). Crohn’s disease, gynaecological cancer and infection. Iatrogenic causes: unintended consequence of colorectal anastomosis, anorectal operations, or radiation therapy (uncommon in low-resource settings)
Social causes that contribute to the issue: poverty, education, role of women in decision making, early marriage, harmful traditional practices, family planning - spacing of childbearing
Mechanism of Injury / Pathological Process[edit | edit source]
Necrosis of surrounding tissue due to pressure of the baby’s head against the pelvis. The reduced flow of blood to the soft tissues surrounding the bladder, vagina and rectum results in necrosis of the tissue. If the mother survives, this kind of labour often ends when the fetus dies and gradually decomposes enough to slide out of the vagina. The injured pelvic tissue also rots away, leaving a hole, or a fistula, between adjacent organs
VVF, RVF or combined
Clinical Presentation[edit | edit source]
Urinary or Faecal incontinence
Diagnostic Procedures[edit | edit source]
Through physical examination and report of symptoms
(add differential diagnosis - if relevant)
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Surgery - simple but need training. Special fistula hospitals. Most doctors in low resource settings lack the training or resources to identify and repair fistula
Physical rehabilitation
Education
Psychological support
Physiotherapy Management[edit | edit source]
Pre-op
Post-op
Resources
[edit | edit source]
Obstetric Fistula E-learning course - https://www.gfmer.ch/fistula/Obstetric-fistula-2015.htm
References[edit | edit source]
- ↑ Muleta M, Hamlin C, Fantahun M, Kennedy R and Tafesse B. Health and Social Problems Encountered by Treated and Untreated Obstetric Fistula Patients in Rural Ethiopia. Journal of Obstetrics and Gynaecology Canada. 2008.30(1). pp. 44-50. 30(1). pp. 44-50.
- ↑ Lombard L, St. Jorre J, Geddes R, El Ayadi A and Grant L. Rehabilitation experiences after obstetric fistula repair: systematic review of qualitative studies. Tropical medicine and International health. 2015 20(5). pp. 554-568.
- ↑ Desalliers J, Pare ME, Kouraogo S and Corcos J. Impact of surgery on quality of life of women with obstetric fistula: a qualitative study in Burkina Faso. International Urogynecological Journal. 2017. 28(7). pp.1091- 1100.
- ↑ World health Organisation. Obstetric Fistula [online]. 2021. Available from: https://www.who.int/news-room/facts-in-pictures/detail/10-facts-on-obstetric-fistula Accessed 18 Nov 2021
- ↑ Lombard L, St. Jorre J, Geddes R, El Ayadi A and Grant L. Rehabilitation experiences after obstetric fistula repair: systematic review of qualitative studies. Tropical medicine and International health. 2015. 20(5). pp. 554-568.