Thumb Ligament Injuries: Difference between revisions
No edit summary |
No edit summary |
||
| Line 51: | Line 51: | ||
because of pain and swelling in the acute setting | because of pain and swelling in the acute setting | ||
== Outcome Measures == | == Outcome Measures == | ||
Revision as of 16:28, 31 October 2020
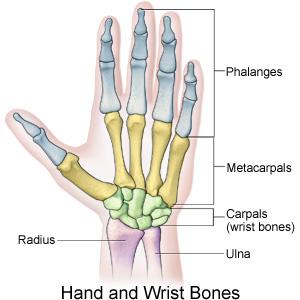
Clinical Relevant Anatomy[edit | edit source]
The thumb MCP is similar in anatomical appearance to those of the finger,but essentially functions as a hinge or ginglymus joints. The articular morphology found in this joint makes it the most varied motion of all joints, with range of motion of 6 to 86 degree in flexion-extension. [1]
- flexor pollicis brevis (FBP)
- Abductor pollicis brevis (APB) muscles insert partially on the sesamoids and provide stability against hyperextension forces.
The ligamentous anatomy is analogous to that seen in the finger MCP joints, with extrinsic tendons providing additional support
Mechanism of Injury / Pathological Process[edit | edit source]
The Metacarpophalangeal (MCP) joint of the thumb are stabilize by two major ligaments. The ulnar collateral ligament (UCL) and the Radial collateral ligament (RCL) . The UCL is more commonly injured, usually from forced radial deviation (abduction) of the thumb, while the RCL are rarely injuried. However, in severe type of injuries, both ligaments may be ruptured.[2]
Clinical Presentation[edit | edit source]
add text here relating to the clinical presentatio
Diagnostic Procedures[edit | edit source]
History taking, including mechanism, finger position during injury, the presence of deformity, previous treatment received, and subjective sense of stability of the injured thumb.
• Neurovascular exam must determine motor function, perfusion, and
sensation.
• Weakness with pinch function usually exists in ligament ruptures.
• Examine the base of the thumb for ligamentous laxity and compare it
to the uninjured hand:
• Examine the thumb with 20–30* of flexion.
• Carefully abduct the thumb passively and compare the angle of
deviation to the uninjured thumb.
• An angulation of >30* on the injured thumb or >15* compared to
the uninjured thumb is diagnostic for a ligamentous injury.
• Radiography should be obtained to assess for the presence of a Stener's lesion or a fracture fragment.
•further assessment of joint should be performed using a digital block may be necessary to complete a full examination
because of pain and swelling in the acute setting
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions[edit | edit source]
A thumb spica splint or cast immobilization is indicated for 4 weeks for
a partial rupture, or up to 6 weeks if an associated avulsion fracture is
present.
For acute injury
• Rest, elevation, ice
• Immobilization in a thumb spica splint
• Analgesics
• Orthopedic follow-up
For chronic injury
• Thumb spica brace
• Activity modifi cation
• Orthopedic surgery consultation for elective ligament repair or
reconstruction may be necessary with a complete rupture.
Physical or occupational therapy is helpful postoperatively to increase
range of motion and strength, and to assist in resuming activities
Differential Diagnosis[edit | edit source]
• First metacarpal or proximal phalanx fractures
• First CMC joint arthritis
• Volar plate injury
Resources[edit | edit source]
add appropriate resources here