Pudendal Neuralgia: Difference between revisions
Sazia Queyam (talk | contribs) m (Added picture) |
Sazia Queyam (talk | contribs) m (g) |
||
| Line 12: | Line 12: | ||
Neuralgia (Greek neuron, "nerve" + algos, "pain") is pain in the distribution of a nerve or nerves. | Neuralgia (Greek neuron, "nerve" + algos, "pain") is pain in the distribution of a nerve or nerves. | ||
It is a chronic neuropathic pelvic pain that is often misdiagnosed and inappropriately treated by many practitioners. | |||
It occurs in both men and women, although studies reveal that about two-thirds of those with the disease are women. The primary symptom is pain in the genitals or the anal-rectal area and the immense discomfort is usually worse when sitting. The pain tends to move around in the pelvic area and can occur on one or both sides of the body. Sufferers describe the pain as burning, knife-like or aching, stabbing, pinching, twisting and even numbness. | |||
Other terms that one may find related to Pudendal neuralgia are- Pudendal Nerve Entrapment, Pudendal Neuropathy, Bicyclist syndrome, obstetric neuropathy, Alcock Canal Syndrome. | |||
Point to be noted is that the sufferer might display all the symptoms of pudendal neuralgia but not actually have an entrapped (pinched) pudendal nerve. Entrapment is just one possible cause. | |||
=== Clinically Relevant Anatomy === | === Clinically Relevant Anatomy === | ||
| Line 22: | Line 26: | ||
The pudendal nerve is paired, meaning there are two nerves, one on the left and one on the right side of the body. | The pudendal nerve is paired, meaning there are two nerves, one on the left and one on the right side of the body. | ||
* '''Nerve roots''' – S2-S4 | |||
* '''Sensory''' – innervates the external genitalia of both sexes and the skin around the anus, anal canal and perineum | |||
* '''Motor''' – innervates various pelvic muscles, the external urethral sphincter and the external anal sphincter. | |||
* '''Autonomic''' – carries sympathetic nerve fibres to the skin of the S2-S4 dermatomal region. | |||
<br> | |||
<br> | |||
== Pathophysiology == | |||
It can be unilateral or bilateral. | |||
Causes include compression, stretch, direct trauma, and radiation. Pudendal neuralgia is a functional entrapment where pain occurs during a compression or stretch maneuver. The neuropathy worsens due to repetitive microtrauma resulting in persistent pain and dysfunctional complaints. The pudendal nerve is compressed during prolong sitting and cycling. | |||
Stretch of the nerve by straining with constipation and childbirth can cause pudendal neuropathy. Fitness exercises, machines, weight lifting with squats, leg presses or karate with kick boxing and rollerblading are all etiologic factors. Youthful sports are a common denominator, possibly related to bony remodeling of the ischial spine. Driving over rough roads or farm fields causes vibration trauma. Falls onto the buttocks can cause pudendal neuralgia.[ Source: http://www.painspa.co.uk/conditions/pudendal-neuralgia/] | |||
== Clinical Presentation == | == Clinical Presentation == | ||
| Line 50: | Line 58: | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Diagnostic criteria were defined at the Nantes Consensus Conference in 2006. Five essential criteria must all be present: pain limited to the territory of innervation of pudendal nerve, pain predominant during sitting, pain does not awaken patient from sleep, no objective sensory defects, positive effect of anesthetic infiltration of the pudendal nerve. | |||
Physical examination focuses on a simple pudendal neurological evaluation. Pinprick sensation is tested at each branch bilaterally: dorsal nerve (clitoris and glans penis), perineal nerve (posterior labia and posterior scrotum), and inferior anal nerve (posterior perianal skin). Hyperalgesia is more common than hypoalgesia. Normal sensation to pinprick may occur even when quantitative sensory testing is abnormal. Pressure is placed on the nerve at the Alcock canal and medial to the ischial spine attempting to reproduce pain, bladder, or rectal symptoms—the Valleix phenomenon.<br> | |||
== Outcome Measures == | == Outcome Measures == | ||
| Line 59: | Line 69: | ||
== Management / Interventions<br> == | == Management / Interventions<br> == | ||
Invasive Interventions which are performed by experinced practicioners: | |||
# Pudendal Nerve Release Surgery. | |||
# Botox / Botulinum toxin Type A injections. | |||
# Pulsed radio-frequency treatment of the pudendal nerve, sacral nerve roots or sacroiliac joints. | |||
# Cortisone injections. | |||
# Activated platelet extract injections (PRP platelet-rich plasma). | |||
# Hyaluronic acid injections. | |||
# Neuro-modulation with implantable electrodes. | |||
Pharmacological Management: Medications can be used in patients who fail lifestyle modifications. Anti neuropathic drugs are the mainstay of management in pudendal neuralgia. These drugs include tricyclics, gabapentinoids and selective noradrenaline reuptake inhibitors (SNRIs). | |||
Clinical management depends on the cause of distress to the nerve. When the cause is not obvious patients are advised to try the least invasive and least risky therapies initially. | |||
Self management includes: Lifestyle changes and exercises to relax muscles surrounding the affected nerve. | |||
Patients should use a cushion that supports the ischial tuberosities to elevate the pelvic floor off the seat. This support decreases the pressure applied to the pelvic floor muscles and pudendal nerve. Avoidance of postures or movement which triggers pain. | |||
Pelvic Floor Relaxation exercises. | |||
== Differential Diagnosis<br> == | == Differential Diagnosis<br> == | ||
# Prostatitis. | |||
# Prostadynia. | |||
# Endometriosis. | |||
# Vulvodynia. | |||
# <br> | |||
== Resources <br> == | == Resources <br> == | ||
Revision as of 23:03, 16 June 2018
Original Editor - Sazia Queyam
Lead Editors
Introduction[edit | edit source]
Pudendal ( Latin pudenda, meaning “external genitals”, derived from pudendum, meaning "parts to be ashamed of".
Neuralgia (Greek neuron, "nerve" + algos, "pain") is pain in the distribution of a nerve or nerves.
It is a chronic neuropathic pelvic pain that is often misdiagnosed and inappropriately treated by many practitioners.
It occurs in both men and women, although studies reveal that about two-thirds of those with the disease are women. The primary symptom is pain in the genitals or the anal-rectal area and the immense discomfort is usually worse when sitting. The pain tends to move around in the pelvic area and can occur on one or both sides of the body. Sufferers describe the pain as burning, knife-like or aching, stabbing, pinching, twisting and even numbness.
Other terms that one may find related to Pudendal neuralgia are- Pudendal Nerve Entrapment, Pudendal Neuropathy, Bicyclist syndrome, obstetric neuropathy, Alcock Canal Syndrome.
Point to be noted is that the sufferer might display all the symptoms of pudendal neuralgia but not actually have an entrapped (pinched) pudendal nerve. Entrapment is just one possible cause.
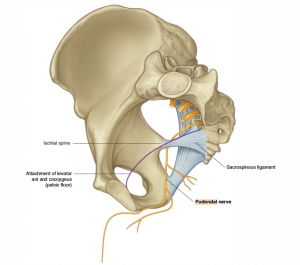
Clinically Relevant Anatomy[edit | edit source]
The pudendal nerve is paired, meaning there are two nerves, one on the left and one on the right side of the body.
- Nerve roots – S2-S4
- Sensory – innervates the external genitalia of both sexes and the skin around the anus, anal canal and perineum
- Motor – innervates various pelvic muscles, the external urethral sphincter and the external anal sphincter.
- Autonomic – carries sympathetic nerve fibres to the skin of the S2-S4 dermatomal region.
Pathophysiology[edit | edit source]
It can be unilateral or bilateral.
Causes include compression, stretch, direct trauma, and radiation. Pudendal neuralgia is a functional entrapment where pain occurs during a compression or stretch maneuver. The neuropathy worsens due to repetitive microtrauma resulting in persistent pain and dysfunctional complaints. The pudendal nerve is compressed during prolong sitting and cycling.
Stretch of the nerve by straining with constipation and childbirth can cause pudendal neuropathy. Fitness exercises, machines, weight lifting with squats, leg presses or karate with kick boxing and rollerblading are all etiologic factors. Youthful sports are a common denominator, possibly related to bony remodeling of the ischial spine. Driving over rough roads or farm fields causes vibration trauma. Falls onto the buttocks can cause pudendal neuralgia.[ Source: http://www.painspa.co.uk/conditions/pudendal-neuralgia/]
Clinical Presentation[edit | edit source]
Clinical characteristics include pelvic pain with sitting which increases throughout the day and decreases with standing or lying down,
sexual dysfunction and difficult with urination and/or defecation. To confirm pudendal neuralgia, the Nantes criteria are recommended.
Treatment includes behavioral modifications, physiotherapy, analgesics and nerve block, surgical pudendal nerve decompression,
radiofrequency and spinal cord stimulation.[ Source: Management of pudendal neuralgia. F. R. Pérez-López, link: https://doi.org/10.3109/13697137.2014.912263]
In most cases, patients will describe neuropathic pain – a burning, tingling, or numbing pain – that is worse with sitting, and less severe or absent when standing or lying down.
Initially, pain may be present only with sitting, but with time pain becomes more constant and severely aggravated by sitting. Many of my patients cannot tolerate sitting at all. Interestingly, patients usually report less pain when sitting on a toilet seat, a phenomenon that we believe is associated with pressure being applied to the ischial tuberosities rather than to the pelvic floor muscles. Pain usually gets progressively worse through the day.
Diagnostic Procedures[edit | edit source]
Diagnostic criteria were defined at the Nantes Consensus Conference in 2006. Five essential criteria must all be present: pain limited to the territory of innervation of pudendal nerve, pain predominant during sitting, pain does not awaken patient from sleep, no objective sensory defects, positive effect of anesthetic infiltration of the pudendal nerve.
Physical examination focuses on a simple pudendal neurological evaluation. Pinprick sensation is tested at each branch bilaterally: dorsal nerve (clitoris and glans penis), perineal nerve (posterior labia and posterior scrotum), and inferior anal nerve (posterior perianal skin). Hyperalgesia is more common than hypoalgesia. Normal sensation to pinprick may occur even when quantitative sensory testing is abnormal. Pressure is placed on the nerve at the Alcock canal and medial to the ischial spine attempting to reproduce pain, bladder, or rectal symptoms—the Valleix phenomenon.
Outcome Measures[edit | edit source]
The McGill Pain Questionnaire, also known as McGill Pain Index, is a scale of rating pain developed at McGill University by Melzack and Torgerson in 1971. It is a self-report questionnaire that allows individuals to give their doctor a good description of the quality and intensity of pain that they are experiencing.
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
Invasive Interventions which are performed by experinced practicioners:
- Pudendal Nerve Release Surgery.
- Botox / Botulinum toxin Type A injections.
- Pulsed radio-frequency treatment of the pudendal nerve, sacral nerve roots or sacroiliac joints.
- Cortisone injections.
- Activated platelet extract injections (PRP platelet-rich plasma).
- Hyaluronic acid injections.
- Neuro-modulation with implantable electrodes.
Pharmacological Management: Medications can be used in patients who fail lifestyle modifications. Anti neuropathic drugs are the mainstay of management in pudendal neuralgia. These drugs include tricyclics, gabapentinoids and selective noradrenaline reuptake inhibitors (SNRIs).
Clinical management depends on the cause of distress to the nerve. When the cause is not obvious patients are advised to try the least invasive and least risky therapies initially.
Self management includes: Lifestyle changes and exercises to relax muscles surrounding the affected nerve.
Patients should use a cushion that supports the ischial tuberosities to elevate the pelvic floor off the seat. This support decreases the pressure applied to the pelvic floor muscles and pudendal nerve. Avoidance of postures or movement which triggers pain.
Pelvic Floor Relaxation exercises.
Differential Diagnosis
[edit | edit source]
- Prostatitis.
- Prostadynia.
- Endometriosis.
- Vulvodynia.
Resources
[edit | edit source]
add appropriate resources here