Childhood Obesity: Difference between revisions
(added to obesity overview section and edited learning outcomes) |
(added to role of physiotherapist section and edited overview slightly) |
||
| Line 26: | Line 26: | ||
* Obese: BMI = 30-39.9 | * Obese: BMI = 30-39.9 | ||
* Severely Obese: BMI = ≥40 | * Severely Obese: BMI = ≥40 | ||
In children, BMI is not used to diagnose obesity, as children's bodies are constantly changing. | In children, BMI alone is not used to diagnose obesity, as children's bodies are constantly changing. To diagnose childhood obesity, paediatricians need to take many factors into consideration. Your child's doctor will first calculate which percentile of weight your child falls into. For example, if your child is in the 80th percentile for weight (based on BMI), this means that 80% of children of the same sex and age have a lower BMI. Along with this calculation, the paediatrician will take into consideration how your child is growing and developing, your family's history of obesity and related health problems (such as diabetes and heart disease), and your child's eating habits, activity levels, and general health. A diagnosis of childhood obesity will rely on all of these factors taken together, rather than BMI calculation alone. | ||
==== <u>The Problem</u> ==== | ==== <u>The Problem</u> ==== | ||
| Line 35: | Line 35: | ||
* Children tend to consume food and drinks high in fat and/or sugar more often than adults (REF) | * Children tend to consume food and drinks high in fat and/or sugar more often than adults (REF) | ||
==== <u> | ==== <u>Why does Childhood Obesity Matter?</u> ==== | ||
* Childhood obesity is linked to a greater risk of disability and premature death in adulthood | |||
* Individuals who are overweight or obese in childhood are more likely to be overweight or obese in adulthood | |||
* Obesity is associated with early development of diseases such as diabetes, heart disease, and certain types of cancer | |||
* Childhood obesity can predispose children to sleep apnoea, joint problems, back pain, and early puberty | |||
* Psychological issues such as low self-esteem and depression are more common in overweight children than in children of healthy weight | |||
==== <u>Things seem to be improving...</u> ==== | |||
* 76% of children age 5-15 meet physical activity guidelines, which is an increase from 71% in 2008 (REF) | * 76% of children age 5-15 meet physical activity guidelines, which is an increase from 71% in 2008 (REF) | ||
* 70% of children are considered to be a healthy weight | * 70% of children are considered to be a healthy weight | ||
* Childhood obesity has declined from 17% to 14% since 2014 | * Childhood obesity has declined from 17% to 14% since 2014 | ||
== Managing Childhood Obesity as a Parent == | == Managing Childhood Obesity as a Parent == | ||
== The Role of the Physiotherapist in Managing Childhood Obesity == | |||
Physiotherapists have many unique skills that are well-suited to addressing childhood obesity. Physiotherapists undergo training in anatomy, movement science, and behaviour-change techniques that allow them to prescribe physical activity and lifestyle changes in an effective and safe manner. Though physiotherapy may be traditionally thought of as a clinical or hospital role, physiotherapists work in a variety of settings including schools, care centres, and in the community. The continuing trend of inactivity and risk of obesity in children means that the role of physiotherapists will need to further expand in order to address these problems. | |||
Some of the ways in which physiotherapists could help in the management of childhood obesity include: | |||
* Assisting in the development of physical education programmes in schools | |||
* Address childhood obesity when coming into contact with overweight or obese children in a clinical setting | |||
* Encourage physical activity and outline physical activity guidelines for all children | |||
* Discuss lifestyle changes with parents of overweight or obese children including changes in nutrition and exercise | |||
* Treat muscle and joint problems that may be interfering with physical activity | |||
* Provide feedback and motivation for children and their families | |||
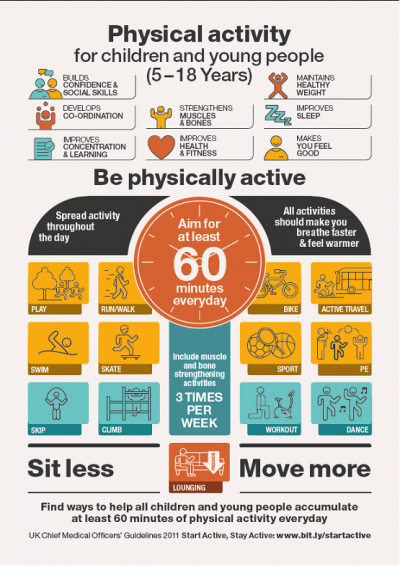
== Physical Activity Guidelines == | == Physical Activity Guidelines for Children (Age 5-12) == | ||
[[File:CMO+early+years+infographic+July+2016.png|left|thumb|566x566px]] | [[File:CMO+early+years+infographic+July+2016.png|left|thumb|566x566px]] | ||
[[File:Infograph.png|center|thumb|566x566px]] | [[File:Infograph.png|center|thumb|566x566px]] | ||
| Line 53: | Line 65: | ||
== Benefits of Physical Activity for Your Child (...and risks of inactivity) == | == Benefits of Physical Activity for Your Child (...and risks of inactivity) == | ||
== Barriers and Facilitators to Managing Childhood Obesity == | == Barriers and Facilitators to Managing Childhood Obesity - Behaviour Change Models for Children?? == | ||
== Local Opportunities for Physical Activity in Edinburgh == | == Local Opportunities for Physical Activity in Edinburgh == | ||
Revision as of 18:08, 6 March 2018
Original Editors - Alexander Dow, Andrea Civitarese, Lynne Turner, Alison O’Brien, Rachael Le Page, Courtney Ferguson
Top Contributors - Andrea Civitarese, Rachael Le Page, Lynne Turner, Kim Jackson, Lucinda hampton, Courtney Ferguson, Alison O' Brien, Alexander Dow and Rachael Lowe
Introduction[edit | edit source]
Aims[edit | edit source]
The goal of this page is to provide guidance and information for parents of overweight children, and to empower them to feel confident in managing childhood obesity.
Learning Outcomes[edit | edit source]
- Define childhood obesity and recognize its impact
- Recognize the benefits of physical activity and risks of inactivity
- Apply physical activity guidelines for children
- Define the role of physiotherapists in managing childhood obesity
- Apply management strategies for childhood obesity
- Identify local resources and physical activity opportunities for overweight or obese children and their families
Obesity Overview[edit | edit source]
What is Childhood Obesity?[edit | edit source]
For adults, body mass index (BMI) is the method that is most commonly used to diagnose obesity. This method uses an individual's height and weight to establish whether or not they fall within a healthy weight range. BMI ranges are listed below:
- Healthy weight: BMI = 18.5-24.9
- Overweight: BMI = 25-29.9
- Obese: BMI = 30-39.9
- Severely Obese: BMI = ≥40
In children, BMI alone is not used to diagnose obesity, as children's bodies are constantly changing. To diagnose childhood obesity, paediatricians need to take many factors into consideration. Your child's doctor will first calculate which percentile of weight your child falls into. For example, if your child is in the 80th percentile for weight (based on BMI), this means that 80% of children of the same sex and age have a lower BMI. Along with this calculation, the paediatrician will take into consideration how your child is growing and developing, your family's history of obesity and related health problems (such as diabetes and heart disease), and your child's eating habits, activity levels, and general health. A diagnosis of childhood obesity will rely on all of these factors taken together, rather than BMI calculation alone.
The Problem[edit | edit source]
- 16% of children in Scotland age 7-11 and 15% age 12-15 are at risk of obesity (REFERENCE). This means that about 150,000 children are currently at risk for obesity.
- Children who live in deprived areas are less likely to be of a healthy weight (REFERENCE)
- Younger children are more likely than older children to meet physical activity guidelines (REFERENCE)
- Girls tend to have lower levels of activity than boys (REF)
- Children tend to consume food and drinks high in fat and/or sugar more often than adults (REF)
Why does Childhood Obesity Matter?[edit | edit source]
- Childhood obesity is linked to a greater risk of disability and premature death in adulthood
- Individuals who are overweight or obese in childhood are more likely to be overweight or obese in adulthood
- Obesity is associated with early development of diseases such as diabetes, heart disease, and certain types of cancer
- Childhood obesity can predispose children to sleep apnoea, joint problems, back pain, and early puberty
- Psychological issues such as low self-esteem and depression are more common in overweight children than in children of healthy weight
Things seem to be improving...[edit | edit source]
- 76% of children age 5-15 meet physical activity guidelines, which is an increase from 71% in 2008 (REF)
- 70% of children are considered to be a healthy weight
- Childhood obesity has declined from 17% to 14% since 2014
Managing Childhood Obesity as a Parent[edit | edit source]
The Role of the Physiotherapist in Managing Childhood Obesity[edit | edit source]
Physiotherapists have many unique skills that are well-suited to addressing childhood obesity. Physiotherapists undergo training in anatomy, movement science, and behaviour-change techniques that allow them to prescribe physical activity and lifestyle changes in an effective and safe manner. Though physiotherapy may be traditionally thought of as a clinical or hospital role, physiotherapists work in a variety of settings including schools, care centres, and in the community. The continuing trend of inactivity and risk of obesity in children means that the role of physiotherapists will need to further expand in order to address these problems.
Some of the ways in which physiotherapists could help in the management of childhood obesity include:
- Assisting in the development of physical education programmes in schools
- Address childhood obesity when coming into contact with overweight or obese children in a clinical setting
- Encourage physical activity and outline physical activity guidelines for all children
- Discuss lifestyle changes with parents of overweight or obese children including changes in nutrition and exercise
- Treat muscle and joint problems that may be interfering with physical activity
- Provide feedback and motivation for children and their families
Physical Activity Guidelines for Children (Age 5-12)[edit | edit source]
Benefits of Physical Activity for Your Child (...and risks of inactivity)[edit | edit source]
Barriers and Facilitators to Managing Childhood Obesity - Behaviour Change Models for Children??[edit | edit source]
Local Opportunities for Physical Activity in Edinburgh[edit | edit source]
Specific Exercise Options for Different Socio-Economic Groups[edit | edit source]
Conclusion[edit | edit source]
Useful Links[edit | edit source]
References[edit | edit source]
see adding references tutorial.