Pain Neuroscience Education (PNE): Difference between revisions
Lynette Fox (talk | contribs) No edit summary |
Lynette Fox (talk | contribs) No edit summary |
||
| Line 157: | Line 157: | ||
#Podcasts | #Podcasts | ||
Chews health podcast SESSION 4 – KNOW PAIN: METAPHORIC EXPRESSION WITH MIKE STEWART – [http://chewshealth.co.uk/tpmpsession4/ PART 1], [http://chewshealth.co.uk/tpmpsession5/ PART 2] | Chews health podcast SESSION 4 – KNOW PAIN: METAPHORIC EXPRESSION WITH MIKE STEWART – [http://chewshealth.co.uk/tpmpsession4/ PART 1], [http://chewshealth.co.uk/tpmpsession5/ PART 2] | ||
Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider [http://physiouk.s3.amazonaws.com/Mike%20Stewart_Know%20Pain_Interview.mp3?inf_contact_key=f652f9d7e9bb1e1e7769a05d4cce3545ada22cb05afed3dc0bbf3a3f95e585cd discussion] | Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider [http://physiouk.s3.amazonaws.com/Mike%20Stewart_Know%20Pain_Interview.mp3?inf_contact_key=f652f9d7e9bb1e1e7769a05d4cce3545ada22cb05afed3dc0bbf3a3f95e585cd discussion] | ||
#Youtube videos | #Youtube videos | ||
#Books | #Books | ||
#Research | #Research | ||
#Website | #Website | ||
#Other | |||
Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider [http://www.physiouk.co.uk/course_pdfs/MikeS_Know_Pain_Transcript.pdf?inf_contact_key=ce65762746464ffc93c7afb89146987b5938f00a5ee899cc899e1bef4f1da23c discussion (transcription)] | |||
<br> | <br> | ||
| Line 174: | Line 177: | ||
*Resources | *Resources | ||
<br> | <br> | ||
*References:<br> | *References:<br> | ||
Revision as of 21:03, 13 January 2016
- What is Pain Neuroscience Education (PNE)?
- What does PNE consist of / involve?
- Rx to resolve?
- Indicators for the use of PNE
Low Back Pain
Low back pain (LBP) is currently considered to be the most common cause of disability and time off work in the over 45 age group, with it being reported that 84% people will experience LBP at some point during their life (Balagué et al., 2012). Whilst LBP is generally considered a self-limiting condition it can have severe implications to the patient’s psychological and physical health. Results from a UK survey, analysing the consultation prevalence for LBP showed that 417 per 10 000 registered patients sought medical help for their LBP, with the highest numbers being seen in the 45- 64 age group (536 per 10 000) (Jordan et al., 2010). Furthermore an Australian cohort study discovered whilst most patient’s recovered 1/3 had not fully recovered after 1 year (Henschke et al., 2008). LBP is clearly a substantial problem for both the health system and the socioeconomic environment, thus effective management is critical.
Updated NICE guidelines for Chronic LBP states that information and self-care advice should be provided to patients to promote self-management by fostering a positive attitude and providing realistic expectations to patients. However the type, duration, frequency and content of this advice was not reported on (NICE, 2015).
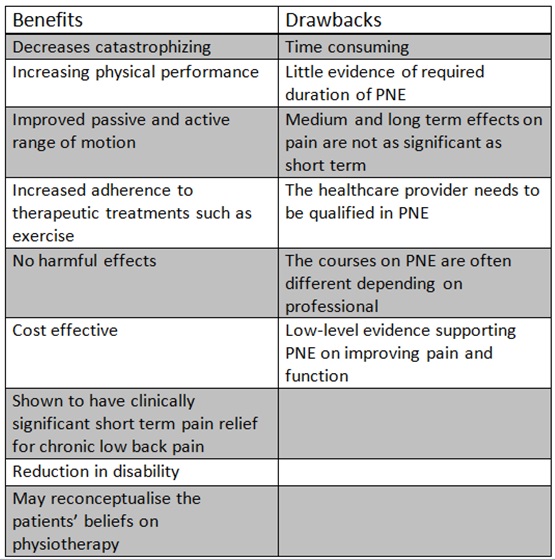
- The benefits and drawbacks of PNE
Brain activity clinical imaging of PNE effect
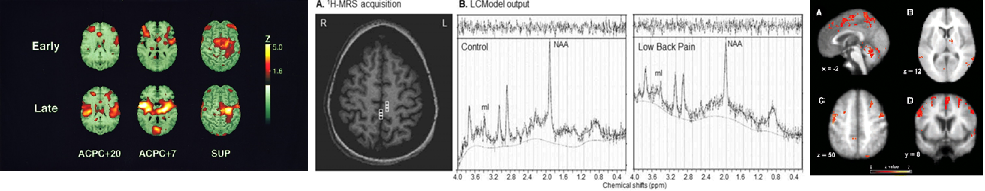
There are various types of brain imaging including those pictured below:
Figure ?. Pictured left to right are Positron emission tomography (PET), magnetic resonance spectroscopy (MRS) and functional magnetic resonance imaging (fMRI) of pain. (Sharma, Brooks, Popescu et al., 2012; Cole, Farrell, Duff et al., 2006; Casey, Morrow, Lorenz et al., 2001).
Effects of therapeutic neuroscience education
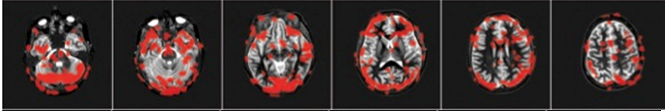
By teaching a patient more about how pain works with reassurance that pain doesn’t always mean tissue damage, their pain eases considerably and they experience other benefits including increased movement, better function and reduced fear avoidance. These effects are measurable via brain imaging as demonstrated below:
A high-level dancer experiencing significant back pain for almost two years who was scheduled for back surgery in two days was scanned using fMRI. Areas of brain activity related to pain are demarcated in red.
Row 1: Patient relaxing. Note no red areas. 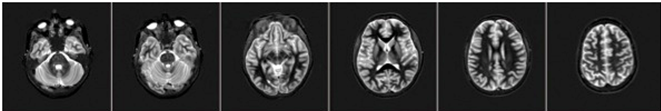
Row 2: Patient was asked her to move her painful back while in scanner. These images demonstrated brain activity related to pain whereby larger areas of red signifies more pain.
Row 3: After initial scans the patient taken out of the scanner and provided with a teaching session of 20-25 minutes about pain. The scan of the patient was immediately repeated doing the same painful task as performed in Row 2. Note this time, however, there is significantly less activity (fewer red areas), while doing the same painful task as before.
(Louw A, et. al 2014 – submitted for publication)
There is an obvious link in attention to pain that when negatively perceived, impacts on the experience of pain being greater. One study by Cole, Farrell and Duff et al., (2006) demonstrated that pain related brain activity was greater in pts with Alzheimer’s, than age matched healthy controls. However, in this population there is less reporting of pain and analgesic use. Is this due to difficulty to communicate pain or due to reduced attention to pain?
- Which patients groups it works best for
- Training / education of therapists to use it
- What is the history and where has it been developed from?
- History of pain models and devlopment of PNE
Where has PNE developed from?
The biomedical model is most commonly used by physiotherapists and other medical health professionals for the management of pain (Louw, 2014 & Linton, 2005). The model follows that pain and injury interrelated, thus an increase in pain means further tissue damage have occurred (Louw, 2014) and vice-versa. This model, called the Cartesian model, is over 450 years old, and many argue inaccurate and significantly outdated (Louw, 2014).
Cartesian Model
The Cartesian ‘mid-body’ was first proposed in the early 16th Century by the French Philosopher, Mathematician and Scientist Rene Descartes, in an attempt to show that humans were a mechanical body controlled by a rational soul (Linton, 2005). Descartes model proposed that the brain was the centre of senses, receiving hollow nerve tubes through which free spirits flowed. Nerves were connected to the brain as a piece of rope may be connected to an alarm; thus as pulling of the rope would cause the alarm to sound, injury caused a mechanical-like rope to be pulled, activating a bell in the individuals mind (Linton, 2005). Descartes therefore considered there was a direct correlation between the extent of tissue damage and pain experienced, the greater the extent of damage the more intense the pain experienced (Linton, 2005)
Why is the model considered outdated?
Descartes model continues to be used in current medical practice and influences the perception that all pain is a result of injury and tissue damage (Linton, 2005). Clinicians frequently use the biological model to explain patient’s pain, describing pain as being due to either disc, joint or abnormal movement pattern (Louw, 2014). The resulting treatment is therefore focused on addressing the abnormal movement pattern or faulty tissue, and the pain goes away. However research has shown that education using words such as “bulging”, “herniated” and “ruptured” actually increases patient's levels of fear and anxiety, resulting in protected movements and lack of exercise compliance (Louw, 2014).
However Descartes biomedical model has been questioned in recent years, with critics arguing that it fails to consider the perception of pain from the nervous system, as well as the psychological and social factors that may influence recovery (Linton, 2005). Furthermore both psychiatrists and behavioural scientists have highlighted specific medical examples to further question the validity of Descartes model. The examples below suggest that pain may potentially be a phenomenon more than just nociception, and may have a neurological element:
- Pain was not expressed by a soldier injured in war until reaching the hospital (Goldberg, 2008)
- Similar injuries in different patients caused substantially different pain responses (Goldberg, 2008)
- An incision to the skin twice as deep as that of another, does not hurt twice as much (Goldberg, 2008)
- Why 40% of people with horrific injuries felt either no or a low intensity of pain (Melzack, Wall & Ty. 1982)
- Why up to 70% of people's do not report pain or associated symptoms consistent with their X-ray/ MRI finding (Bhattacharyya et al., 2003; Boden et al., 1990)
- Why 51% of amputees reported phantom pain and 76% phantom sensations including: cold, electric sensations and movement in the phantom limb (Kooijmana, 2000).
Furthermore in Beecher’s (1956) comparison study of 150 male civilian patients in contrast to wartime casualties, it was discovered that 83% in the civilian group requested narcotics, whilst only 32% of military patients with the same extent of tissue damage asked for them; thereby suggesting the level of pain experienced is patient dependant. In this example it was proposed the patient's emotions, beliefs and experiences of pain altered the brains interpretation of the pain, resulting in different intensities of pain being experienced.
The Pain-neuroscience education model
In the last century Descartes biomedical model has been replaced by the biopsychosocial model of chronic pain (Goldberg, 2008), in which pain is classified as being due to increased sensitivity of the nervous system rather than further injury (Louw, 2014). In layman’s terms, pain persists after tissue healing, due to the fact that the body’s alarm system remains activated, and are stimulated by a much lower intensity of stimulus (Louw, 2014); i.e. a much lower degree of movement provocation causes pain.
How does this affect clinicians in practice?
Investigations by the Therapeutic Neuroscience research team at the ‘International Spine and Pain Institute’ has discovered that people in pain are interested in pain and more specifically the mechanisms of pain (Louw, Louw & Crous, 2009). Thus current treatment for patients with chronic pain should have a greater focus on educating patients about the neuroscience of their pain, rather than classifying their pain as being due to faulty movement patterns or damaged tissues.
- Section 1 – Scenarios to aid learning and clinical relevance:
- Becky’s Boss interviewed showing an experience of now chronic LBP that was managed by medication only
- Limited education given and ? low knowledge of pain mechanisms etc.
- Diagram of alarm systems (can be a hand drawn and in a simple video format with narration or just images with text)
- Interview (video or transcript) with Leanne @ NUH (to email 06/01/2016)
- Her experiences / beliefs
- What is PNE
- How does she use it?
- What are the outcomes like for her patients?
- Section 3 – Evidence
- Paper 1 (with link)
- Paper 2 (with link)
- Paper 3 (with link)
- Paper 4 (with link)
- NICE Guidelines
- Comment and clinical bottom line of evidence collectively.
- Referances:
Jordan KP, Kadam UT, Hayward R, Porcheret M, Young C, Croft P. (2010). Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskeletal disorders. 11 (144).
Balagué F, Mannion AF, Pellisé F, Cedraschi C. (2012). Non-specific low back pain. The Lancet. 4 (379), 482-91.
Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. (2008). Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ. 337 (a171).
National Institute for Health and Clinical Excellence (2015) Back pain - low (without radiculopathy). Clinical Knowledge Summary. London: NICE.
- Summary:
- Concise summary or key points of the page.
- Resources and useful links:
- Podcasts
Chews health podcast SESSION 4 – KNOW PAIN: METAPHORIC EXPRESSION WITH MIKE STEWART – PART 1, PART 2
Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider discussion
- Youtube videos
- Books
- Research
- Website
- Other
Know Pain course: A Practical guide for Therapeutic Neuroscience Education, course provider discussion (transcription)
- Conclusion of entire page.
- Resources
- References: