Management of Chronic Ankle Instability: Difference between revisions
No edit summary |
(Corrected hyperlink) |
||
| (15 intermediate revisions by 3 users not shown) | |||
| Line 6: | Line 6: | ||
== Definition of Chronic Ankle Instability (CAI) == | == Definition of Chronic Ankle Instability (CAI) == | ||
Chronic ankle instability (CAI) has been defined as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.”<ref>Hertel J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164367/ Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability.] J Athl Train. 2002 Dec;37(4):364-375.</ref> Chronic instability refers to a feeling of apprehension in the ankle, “giving way” and recurrent ankle sprains, persisting for a minimum of | Chronic ankle instability (CAI) has been defined as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.”<ref>Hertel J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164367/ Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability.] J Athl Train. 2002 Dec;37(4):364-375.</ref> Chronic instability refers to a feeling of apprehension in the ankle, “giving way” and recurrent ankle sprains, persisting for a minimum of six months after the initial sprain.<ref name=":1" /> Symptoms include:<ref name=":1" /> | ||
* Lateral ankle pain | * Lateral ankle pain | ||
| Line 14: | Line 14: | ||
* In terms of ''impairments'':<ref name=":0">Hiller CE, Kilbreath SL, Refshauge KM. [https://meridian.allenpress.com/jat/article/46/2/133/191250/Chronic-Ankle-Instability-Evolution-of-the-Model Chronic ankle instability: evolution of the model]. Journal of athletic training. 2011 Mar;46(2):133-41.</ref> | * In terms of ''impairments'':<ref name=":0">Hiller CE, Kilbreath SL, Refshauge KM. [https://meridian.allenpress.com/jat/article/46/2/133/191250/Chronic-Ankle-Instability-Evolution-of-the-Model Chronic ankle instability: evolution of the model]. Journal of athletic training. 2011 Mar;46(2):133-41.</ref> | ||
** | ** Increased ligamentous laxity | ||
** | ** Proprioceptive deficits | ||
* In terms of ''activity limitations:''<ref name=":0" /> | * In terms of ''activity limitations:''<ref name=":0" /> | ||
** | ** Inability to walk | ||
** | ** Inability to jump | ||
* In terms of ''participation'':<ref name=":0" /> | * In terms of ''participation'':<ref name=":0" /> | ||
** | ** Cessation of sport | ||
** | ** Withdrawing from or decreasing occupational involvement | ||
** | ** Decreasing levels of exercise | ||
** | ** Change in the type of sport | ||
=== Long | === Long-term Outcomes === | ||
Patients with CAI | Patients with CAI experience a reduction in their physical quality of life. Treatments may improve stability, but they take a long time and may require specialised equipment.<ref name=":1">Simpson H. Chronic Ankle Instability Course. Physiopedia 2022</ref> Konradsen et al.<ref name=":19">Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002 Jun;12(3):129-35.</ref> conducted a study that followed-up with patients seven years post-ankle inversion trauma. They found the following:<ref name=":19" /> | ||
* 32% of patients reported chronic complaints of pain, swelling or recurrent sprains | * 32% of patients reported chronic complaints of pain, swelling or recurrent sprains | ||
| Line 35: | Line 35: | ||
* 19% were bothered by repeated inversion injuries | * 19% were bothered by repeated inversion injuries | ||
* 43% of these subjects felt that they could compensate by using an external ankle support | * 43% of these subjects felt that they could compensate by using an external ankle support | ||
* 85% of people who develop CAI after unilateral sprain reported problems in the contralateral ankle | * 85% of people who develop CAI after unilateral sprain reported problems in the contralateral ankle | ||
According to Hertel <ref name=":2">Hertel J. Immobilisation for acute severe ankle sprain. Lancet. 2009 Feb 14;373(9663):524-6. </ref>one sprain guarantees another. | According to Hertel,<ref name=":2">Hertel J. Immobilisation for acute severe ankle sprain. Lancet. 2009 Feb 14;373(9663):524-6. </ref> one sprain guarantees another.<ref name=":1" /> And Struijs and Kerkhoffs<ref>Struijs PA, Kerkhoffs GM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2907605/ Ankle sprain]. BMJ Clin Evid. 2010 May 13;2010:1115.</ref> found that there was a 30% recurrence of sprains within a year of injury.<ref name=":1" /> | ||
Additional reported long-term outcomes include: | Additional reported long-term outcomes include: | ||
* Articular cartilage defects on the medial side of the joint due to:<ref name=":1" /> | * Articular cartilage defects on the medial side of the joint due to:<ref name=":1" /> | ||
** Tearing of ATFL and CFL | ** Tearing of anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL) | ||
** Altering and increasing peak cartilage strain | ** Altering and increasing peak cartilage strain | ||
** Leading to tibiotalar cartilage degeneration (OA) | ** Leading to tibiotalar cartilage degeneration (OA) | ||
* Anterior talar positional fault <ref>Wikstrom EA, Hubbard TJ. [https://www.archives-pmr.org/article/S0003-9993(10)00253-4/fulltext Talar positional fault in persons with chronic ankle instability]. Arch Phys Med Rehabil. 2010 Aug;91(8):1267-71.</ref> | * Anterior talar positional fault<ref>Wikstrom EA, Hubbard TJ. [https://www.archives-pmr.org/article/S0003-9993(10)00253-4/fulltext Talar positional fault in persons with chronic ankle instability]. Arch Phys Med Rehabil. 2010 Aug;91(8):1267-71.</ref> | ||
* Altered movement patterns in unstable ankles:<ref name=":1" /> | * Altered movement patterns in unstable ankles:<ref name=":1" /> | ||
** Landing in more dorsiflexion in an attempt to minimise reliance on lateral ligaments and increase bony stability | ** Landing in more dorsiflexion in an attempt to minimise reliance on lateral ligaments and increase bony stability | ||
** In drop jump: greater maximum calcaneal eversion and frontal displacement of the body | ** In drop jump: greater maximum calcaneal eversion and frontal displacement of the body | ||
** Faster time to peak ground reaction force in drop landing | ** Faster time to peak ground reaction force in drop landing | ||
** Greater medial ground reaction force | ** Greater medial ground reaction force | ||
** Metatarsal height is lowered during | ** Metatarsal height is lowered during the terminal swing of gait | ||
* | * | ||
== Mechanical and Functional Instability == | == Mechanical and Functional Instability == | ||
There are two commonly accepted subgroups of CAI: mechanical instability and functional instability. <ref name=":1" /><ref name=":0" />In Hertel's | There are two commonly accepted subgroups of CAI: mechanical instability and functional instability.<ref name=":1" /><ref name=":0" /> In Hertel's<ref name=":3">Hertel J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164367/ Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability.] J Athl Train. 2002 Dec;37(4):364-375</ref> model of ankle stability, mechanical and functional instability are part of a continuum. Recurrent sprains occur when both conditions are present.<ref name=":3" /> | ||
=== Mechanical Instability === | === Mechanical Instability === | ||
Mechanical instability is referred to as pathological ligamentous laxity about the ankle-joint complex<ref>Tropp H. Commentary: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164386/ Functional Ankle Instability Revisited]. J Athl Train. 2002 Dec;37(4):512-515.</ref>Mechanical instability may | Mechanical instability is referred to as pathological ligamentous laxity about the ankle-joint complex.<ref>Tropp H. Commentary: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164386/ Functional Ankle Instability Revisited]. J Athl Train. 2002 Dec;37(4):512-515.</ref> Mechanical instability may be caused by various anatomic changes that are present in isolation or in combination. They can lead to pathologies that are responsible for ankle instability.<ref name=":0" /> | ||
=== Functional Instability === | === Functional Instability === | ||
There is no universally approved definition of functional ankle instability.<ref>Konradsen L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164369/ Factors Contributing to Chronic Ankle Instability: Kinesthesia and Joint Position Sense]. J Athl Train. 2002 Dec;37(4):381-385. </ref> Based on the definition established by | There is no universally approved definition of functional ankle instability.<ref>Konradsen L. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC164369/ Factors Contributing to Chronic Ankle Instability: Kinesthesia and Joint Position Sense]. J Athl Train. 2002 Dec;37(4):381-385. </ref> Based on the definition established by Evans et al.,<ref name=":4">Evans GA, Hardcastle P, Frenyo AD. Acute rupture of the lateral ligament of the ankle. To suture or not to suture? J Bone Joint Surg Br. 1984 Mar;66(2):209-12</ref> functional instability is a subjective complaint of weakness. Lentell et al.<ref name=":5">Lentell G, Katzman LL, Walters MR. The Relationship between Muscle Function and Ankle Stability. J Orthop Sports Phys Ther. 1990;11(12):605-11.</ref> describe functional instability as ankle pain and the perception that the injured ankle is less functional than the other ankle or less functional than pre-injury.<ref name=":5" /> Tropp et al.<ref name=":6">Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985 Jun;6(3):180-2.</ref> concluded that functional instability could be defined as a joint motion that does not exceed normal physiologic limits but is no longer controlled voluntarily.<ref name=":6" /> | ||
Impaired proprioceptive and neuromuscular control can be responsible for functional instability.<ref name=":3" /> | Impaired proprioceptive and neuromuscular control can be responsible for functional instability.<ref name=":3" /> | ||
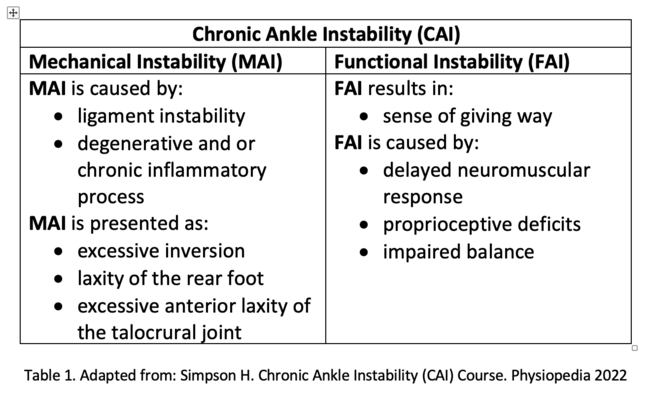
Table 1 summarises the causes and | Mechanical instability is typically presented as excessive inversion, laxity of the rear foot, and excessive anterior laxity of the talocrural joint. It can be caused by ligament instability or degenerative and chronic inflammatory process. In functional instability, on the other hand, patients complain about the sense of the ankle giving way. The delayed neuromuscular response, proprioceptive deficits or impaired balance can cause this symptom. | ||
Table 1 summarises the causes and results of mechanical and functional ankle instability:<ref name=":1" /> | |||
[[File:CAI-2.png|alt=|center|frameless|650x650px]] | [[File:CAI-2.png|alt=|center|frameless|650x650px]] | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Diagnostic procedures | Diagnostic procedures can help clinicians confirm the presence of various ankle deficiencies, including reduced range of motion and perceived disability. This can help to define/diagnose a specific condition. Clinicians should consider if research findings suggest "consistent positive utility" before deciding which diagnostic tool to use:<ref name=":7">Gribble PA. [https://meridian.allenpress.com/jat/article/54/6/617/420891/Evaluating-and-Differentiating-Ankle-Instability Evaluating and differentiating ankle instability]. Journal of athletic training. 2019 Jun;54(6):617-27.</ref> | ||
* Anterior drawer test | * ''' Anterior drawer test''': performed in slight knee flexion to relax the gastrocnemius. However, Kovaleski et al.<ref name=":8">Kovaleski JE, Norrell PM, Heitman RJ, Hollis JM, Pearsall AW. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2386430/ Knee and ankle position, anterior drawer laxity, and stiffness of the ankle complex]. J Athl Train. 2008 May-Jun;43(3):242-8.</ref> suggest testing with the knee flexed to 90° and the ankle at 10° of plantar flexion to isolate the anterior talofibular ligament.<ref name=":8" /> A bilateral comparison is recommended.<ref name=":7" /> Excessive anterior translation and a lack of a solid end feel indicate a positive test result. | ||
* Stress radiography | * '''Stress radiography''': used to quantify the extent of ankle-joint laxity. It shows the separation of the bony joint structures while a force is applied. Clinically, it helps to identify excessive strain within the ligamentous structures. A total anterior translation greater than 9 mm or translation greater than 5 mm (or both) when compared with the contralateral side indicates significant laxity of the anterior talofibular ligament. Pathologic laxity of the calcaneofibular ligament is demonstrated by a talar tilt angle greater than 10°, or an angle that is more than 5° greater than the contralateral limb.<ref name=":7" /> | ||
* [[MRI Scans|MRI]] | * [[MRI Scans|'''MRI''']]: not considered conclusive. Negative MRI results must be viewed with caution in a symptomatic patient and arthroscopy should be considered.<ref>Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010 Jun;16(2):78-80.</ref> | ||
* Diagnostic ultrasound offers moderate to | * '''Diagnostic ultrasound''': evidence suggests that diagnostic ultrasound offers a moderate to strong confirmation of lateral ligamentous injury.<ref>Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010 Jan;39(1):41-7. </ref> It shows increased lateral ligament length during the anterior drawer and talar tilt tests in individuals with a history of CAI.<ref>Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012 Jul;42(7):593-600.</ref> | ||
* Stable force plates | * '''Stable force plates''': suggested for gait and hop stability assessment:<ref name=":12">McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. [https://journals.lww.com/acsm-msse/Fulltext/2008/10000/Balance_Training_Improves_Function_and_Postural.14.aspx Balance training improves function and postural control in those with chronic ankle instability]. Med Sci Sports Exerc. 2008 Oct;40(10):1810-9.</ref> | ||
{{#ev:youtube|v=D6JMr-ZPbjQ|300}}<ref>Vicon. Vicon Gait and Posture Biomechanics. 2018. Available from: https://www.youtube.com/watch?v=D6JMr-ZPbjQ [last accessed 9/07/2022]</ref> | {{#ev:youtube|v=D6JMr-ZPbjQ|300}}<ref>Vicon. Vicon Gait and Posture Biomechanics. 2018. Available from: https://www.youtube.com/watch?v=D6JMr-ZPbjQ [last accessed 9/07/2022]</ref> | ||
* Imaged guided injections of cortisone as a clinical diagnostic tool | * '''Imaged guided injections of cortisone''' as a clinical diagnostic tool. The Delphi-based consensus of experts from the European Society of Musculoskeletal Radiology found that intraarticular foot and ankle anaesthetic injections performed under imaging guidance provide precise information about the source of pain'''.'''<ref>Sconfienza LM, Adriaensen M, Albano D, Alcala-Galiano A, Allen G, et al. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8794903/ Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VI, foot and ankle.] Eur Radiol. 2022 Feb;32(2):1384-94.</ref> | ||
== Physiotherapy Management == | == Physiotherapy Management == | ||
Conservative management is the treatment of choice for acute lateral ankle injuries - a surgical approach for these injuries is reserved for special cases.<ref>Aicale R, Maffulli N. Chronic lateral ankle instability: a topical review. Foot & Ankle International. 2020 Dec;41(12):1571-81.</ref> Currently available conservative modalities include:<ref name=":1" /> | |||
* Neuromuscular training | * Neuromuscular training | ||
| Line 93: | Line 95: | ||
=== Neuromuscular Training === | === Neuromuscular Training === | ||
* | * De Vries et al.<ref name=":9">de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011 Aug 10;(8):CD004124.</ref> found that neuromuscular training alone has a positive short-term outcome and patients had better function.<ref name=":9" /> This type of training is a key feature of the majority of conservative treatment regimes.<ref name=":9" /><ref name=":1" /> | ||
* A study by Kim et al<ref name=":10">Kim E, Choi H, Cha JH, Park JC, Kim T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5358023/ Effects of Neuromuscular Training on the Rear-foot Angle Kinematics in Elite Women Field Hockey Players with Chronic Ankle Instability.] J Sports Sci Med. 2017 Mar 1;16(1):137-146.</ref> | * A study by Kim et al.<ref name=":10">Kim E, Choi H, Cha JH, Park JC, Kim T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5358023/ Effects of Neuromuscular Training on the Rear-foot Angle Kinematics in Elite Women Field Hockey Players with Chronic Ankle Instability.] J Sports Sci Med. 2017 Mar 1;16(1):137-146.</ref> found that athletes with unstable ankles have an altered gait pattern - i.e. a relatively inverted ankle position during the initial contact and midstance. Engaging in six weeks of neuromuscular training immediately changed the athlete's ankle orientation to a relatively more inverted direction during jump landing. However, there was no effect on walking and running.<ref name=":10" /> | ||
* According to Guzmán-Muñoz | * According to Guzmán-Muñoz et al.,<ref name=":11">Guzmán-Muñoz E, Daigre-Prieto M, Soto-Santander K, Concha-Cisternas Y, Méndez-Rebolledo G, Sazo-Rodríguez S, Valdés-Badilla P. [http://archivosdemedicinadeldeporte.com/articulos/upload/or02_guzman-ingles.pdf The effects of neuromuscular training on the postural control of university volleyball players with functional ankle instability: A pilot study.] Archivos de medicina del deporte. 2019;35(5):283-7</ref> four weeks of neuromuscular training improved postural control in college volleyball players with functional ankle instability (FAI) .<ref name=":11" />[[File:Neuromuscular reeducation step 1.jpg|alt=|thumb|216x216px|Step 1]] | ||
[[File:Neuromuscular reeducation step 2.jpg|thumb|216x216px|Step 2]] | [[File:Neuromuscular reeducation step 2.jpg|thumb|216x216px|Step 2]] | ||
[[File:Neuromuscular reeducation step 3.jpg|thumb|216x216px|Step 3]] | [[File:Neuromuscular reeducation step 3.jpg|thumb|216x216px|Step 3]] | ||
==== Guide to Neuromuscular Training ==== | ==== Guide to Neuromuscular Training ==== | ||
Neuromuscular training is | Neuromuscular training is an "unconscious activation of dynamic restraints in preparation and in response to joint motion and loads to maintain and restore functional joint stability".<ref name=":1" /> | ||
Goals of neuromuscular training: | Goals of neuromuscular training: | ||
# To | # To optimise lower limb postural control<ref name=":1" /> | ||
# To restore active stability by training <ref>Loudon JK, Santos MJ, Franks L, Liu W. The effectiveness of active exercise as an intervention for functional ankle instability: a systematic review. Sports Med. 2008;38(7):553-63.</ref> | # To restore active stability by training<ref>Loudon JK, Santos MJ, Franks L, Liu W. The effectiveness of active exercise as an intervention for functional ankle instability: a systematic review. Sports Med. 2008;38(7):553-63.</ref> | ||
===== Exercises ===== | ===== Exercises ===== | ||
Exercises are performed in | Exercises are performed in closed chain and functional positions: | ||
* | * Single limb stance on wobble board or balance mat | ||
* | * Single limb ball toss | ||
* | * Single leg theraband kicks and step downs (see Figures with Steps 1-3) | ||
=== Balance Training === | === Balance Training === | ||
* | * While investigating functional ankle instability and health-related quality of life, Arnold et al.<ref>Arnold BL, Wright CJ, Ross SE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3418941/ Functional ankle instability and health-related quality of life]. J Athl Train. 2011 Nov-Dec;46(6):634-41. </ref> concluded that balance training can affect multiple joints and produce overall improvements.<ref name=":1" /> | ||
* McKeon | * McKeon et al.<ref name=":12" /> showed that balance training significantly improves static postural control and dynamic postural control.<ref name=":1" /> | ||
* A prospective cohort study by Sefton et al <ref>Sefton JM, Yarar C, Hicks-Little CA, Berry JW, Cordova ML. [https://www.jospt.org/doi/epdf/10.2519/jospt.2011.3365 Six weeks of balance training improves sensorimotor function in individuals with chronic ankle instability]. J Orthop Sports Phys Ther. 2011 Feb;41(2):81-9. </ref> found that rehabilitation affects sensorimotor system function.<ref name=":1" /> | * A prospective cohort study by Sefton et al.<ref>Sefton JM, Yarar C, Hicks-Little CA, Berry JW, Cordova ML. [https://www.jospt.org/doi/epdf/10.2519/jospt.2011.3365 Six weeks of balance training improves sensorimotor function in individuals with chronic ankle instability]. J Orthop Sports Phys Ther. 2011 Feb;41(2):81-9. </ref> found that rehabilitation affects sensorimotor system function.<ref name=":1" /> | ||
* Based on | * Based on a review of randomised controlled trials, Mollà Casanova et al.<ref name=":13">Mollà-Casanova S, Inglés M, Serra-Añó P. Effects of balance training on functionality, ankle instability, and dynamic balance outcomes in people with chronic ankle instability: systematic review and meta-analysis. Clinical Rehabilitation. 2021 Dec;35(12):1694-709.</ref> concluded that balance training significantly improves functionality, instability, and dynamic balance outcomes in people with chronic ankle instability.<ref name=":13" /> | ||
==== Guide to Balance Training ==== | ==== Guide to Balance Training ==== | ||
The literature indicates that the following balance measures should guide clinical practice. However, De Vries et al.<ref name=":9" /> did not find a correlation with function: | |||
* | * Centre-of-pressure (COP) excursion<ref>Yousefi M, Sadeghi H, Ilbiegi S, Ebrahimabadi Z, Kakavand M, Wikstrom EA. Center of pressure excursion and muscle activation during gait initiation in individuals with and without chronic ankle instability. Journal of Biomechanics,2020, 18. | ||
</ref> | </ref> | ||
* Time-to-boundary (TTB) after landing<ref>Hertel J, Olmsted-Kramer LC, Challis JH. Time-to-boundary measures of postural control during single-leg quiet standing. J Appl Biomech. 2006 Feb;22(1):67-73.</ref> | * Time-to-boundary (TTB) after landing<ref>Hertel J, Olmsted-Kramer LC, Challis JH. Time-to-boundary measures of postural control during single-leg quiet standing. J Appl Biomech. 2006 Feb;22(1):67-73.</ref> | ||
* Peak plantar analysis<ref>Orlin MN, McPoil TG. [https://academic.oup.com/ptj/article/80/4/399/2842449 Plantar Pressure Assessment]. Physical Therapy 2000; 80( 4): 399–409</ref> | * Peak plantar analysis<ref>Orlin MN, McPoil TG. [https://academic.oup.com/ptj/article/80/4/399/2842449 Plantar Pressure Assessment]. Physical Therapy 2000; 80( 4): 399–409</ref> | ||
*[[Star Excursion Balance Test|SEBT]] | *[[Star Excursion Balance Test|Star Excursion Balance Test (SEBT)]] | ||
===== Proprioception ===== | ===== Proprioception ===== | ||
Kinesthesia and joint position sense (JPS) | Kinesthesia and joint position sense (JPS) are usually impaired in patients with chronic ankle instability.<ref name=":14">Ma T, Li Q, Song Y, Hua Y. [https://reader.elsevier.com/reader/sd/pii/S2095254620301332?token=A55CD5F274084301C297A4C580896992426C2279DB388976687BB5341483686596BCB4BC79664A7317EACC5580DCBB22&originRegion=eu-west-1&originCreation=20220711070542 Chronic ankle instability is associated with proprioception deficits: a systematic review and meta-analysis]. Journal of sport and health science. 2021 Mar 1;10(2):182-91.</ref> The testing methodology for proprioception includes: | ||
* Kinesthesia: assessed using threshold-to-detection of passive motion<ref name=":1" /> | * Kinesthesia: assessed using threshold-to-detection of passive motion<ref name=":1" /> | ||
| Line 144: | Line 145: | ||
* Perturbation exercises with elastic tubing<ref>Han K, Ricard MD, Fellingham GW. [https://www.jospt.org/doi/epdf/10.2519/jospt.2009.2958 Effects of a 4-week exercise program on balance using elastic tubing as a perturbation force for individuals with a history of ankle sprains]. J Orthop Sports Phys Ther. 2009 Apr;39(4):246-55.</ref><ref name=":1" /> | * Perturbation exercises with elastic tubing<ref>Han K, Ricard MD, Fellingham GW. [https://www.jospt.org/doi/epdf/10.2519/jospt.2009.2958 Effects of a 4-week exercise program on balance using elastic tubing as a perturbation force for individuals with a history of ankle sprains]. J Orthop Sports Phys Ther. 2009 Apr;39(4):246-55.</ref><ref name=":1" /> | ||
** | ** Four exercises including front pull, back pull, crossover and reverse crossover, performed 3 times per week. The standard protocol includes 3 sets of 15 repetitions with a resistance band while standing on the affected leg | ||
** Goal: to maintain alignment and stability | ** Goal: to maintain alignment and stability | ||
** Outcome: balance improved in 4 weeks | ** Outcome: balance improved in 4 weeks | ||
=== Mobilisation === | === Mobilisation === | ||
* Limited ankle dorsiflexion during jogging and gait is considered a risk factor for recurrent sprains | * Limited ankle dorsiflexion during jogging and walking gait is considered a risk factor for recurrent sprains because of the following:<ref name=":1" /> | ||
** Inability to reach | ** Inability to reach the closed-packed position of the ankle joint during stance | ||
** Tendency to lock midfoot in supination | ** Tendency to lock midfoot in supination | ||
** The centre of gravity | ** The centre of gravity moves laterally, thus the ankle joint becomes vulnerable to supination and a sprain | ||
* According to Westad et al<ref name=":15">Westad K, Tjoestolvsen F, Hebron C. The effectiveness of Mulligan's mobilisation with movement (MWM) on peripheral joints in musculoskeletal (MSK) conditions: A systematic review. Musculoskeletal Science and Practice. 2019 Feb 1;39:157-63</ref>mobilisation with movement (MWM) | * According to Westad et al.,<ref name=":15">Westad K, Tjoestolvsen F, Hebron C. The effectiveness of Mulligan's mobilisation with movement (MWM) on peripheral joints in musculoskeletal (MSK) conditions: A systematic review. Musculoskeletal Science and Practice. 2019 Feb 1;39:157-63</ref> mobilisation with movement (MWM) techniques used to treat peripheral joints were superior to a placebo, but not to other medical or physiotherapy interventions.<ref name=":15" /> | ||
* The results of a systematic review and meta-analysis by Weerasekara et al<ref name=":16">Weerasekara I, Deam H, Bamborough N, Brown S, Donnelly J, Thorp N, Rivett DA. [https://www.sciencedirect.com/science/article/pii/S0958259219302196 Effect of Mobilisation with Movement (MWM) on clinical outcomes in lateral ankle sprains: a systematic review and meta-analysis.] The Foot. 2020 Jun 1;43:101657.</ref> | * The results of a systematic review and meta-analysis by Weerasekara et al.<ref name=":16">Weerasekara I, Deam H, Bamborough N, Brown S, Donnelly J, Thorp N, Rivett DA. [https://www.sciencedirect.com/science/article/pii/S0958259219302196 Effect of Mobilisation with Movement (MWM) on clinical outcomes in lateral ankle sprains: a systematic review and meta-analysis.] The Foot. 2020 Jun 1;43:101657.</ref> suggest that a mobilisation with movement intervention immediately benefitted patients with chronic ankle instability by increasing dorsiflexion range of motion.<ref name=":16" /> | ||
===== Therapeutic Interventions ===== | ===== Therapeutic Interventions ===== | ||
[[Mulligan | [[Mulligan Concept|Mulligan’s mobilisation with movement]] (MWM) technique should include the following: | ||
* Fibular glide at distal and proximal tibiofibular joint | * Fibular glide at distal and proximal tibiofibular joint | ||
* Talar glide | * Talar glide | ||
Helene Simpson also recommends using an MWM technique that includes midfoot mobility at the navicular.<ref name=":1" /> | |||
=== Braces and | === Braces and Taping === | ||
==== Taping ==== | ==== Taping ==== | ||
* Hubbard and Cordova <ref>Hubbard TJ, Cordova M. Effect of ankle taping on mechanical laxity in chronic ankle instability. Foot Ankle Int. 2010 Jun;31(6):499-504.</ref>found that mechanical laxity decreased after applying | * Hubbard and Cordova<ref>Hubbard TJ, Cordova M. Effect of ankle taping on mechanical laxity in chronic ankle instability. Foot Ankle Int. 2010 Jun;31(6):499-504.</ref> found that mechanical laxity decreased after applying tape.<ref name=":1" /> | ||
* Delahunt et al <ref>Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010 Sep;91(9):1383-9. </ref> found no change in “actual” stability, but patients' perceptions of stability were significantly improved (56%).<ref name=":1" /> | * Delahunt et al.<ref>Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010 Sep;91(9):1383-9. </ref> found no change in “actual” stability, but patients' perceptions of stability were significantly improved (56%).<ref name=":1" /> | ||
* Hopper | * Hopper et al.<ref>Hopper D, Samsson K, Hulenik T, Ng C, Hall T, Robinson K. The influence of Mulligan ankle taping during balance performance in subjects with unilateral chronic ankle instability. Phys Ther Sport. 2009 Nov;10(4):125-30.</ref> found that Mulligan taping had no impact on neuromuscular control during static and dynamic balance.<ref name=":1" /> | ||
===== Therapeutic Intervention ===== | ===== Therapeutic Intervention ===== | ||
| Line 182: | Line 183: | ||
{{#ev:youtube|v=hTQjt7vGNCw|300}}<ref>UCO GATP. Sunderland Special Strip 2 SubTalar Sling - Side View. 2017. Available from: https://www.youtube.com/watch?v=hTQjt7vGNCw [last accessed 13/7/2022]</ref> | {{#ev:youtube|v=hTQjt7vGNCw|300}}<ref>UCO GATP. Sunderland Special Strip 2 SubTalar Sling - Side View. 2017. Available from: https://www.youtube.com/watch?v=hTQjt7vGNCw [last accessed 13/7/2022]</ref> | ||
* Fibular repositioning, <ref>Moiler K, Hall T, Robinson K. [https://www.jospt.org/doi/epdf/10.2519/jospt.2006.2259 The role of fibular tape in the prevention of ankle injury in basketball: A pilot study.] J Orthop Sports Phys Ther. 2006 Sep;36(9):661-8.</ref> but the exact mechanism for reducing the incidence of sprains is unknown | * Fibular repositioning,<ref>Moiler K, Hall T, Robinson K. [https://www.jospt.org/doi/epdf/10.2519/jospt.2006.2259 The role of fibular tape in the prevention of ankle injury in basketball: A pilot study.] J Orthop Sports Phys Ther. 2006 Sep;36(9):661-8.</ref> but the exact mechanism for reducing the incidence of sprains is unknown | ||
{{#ev:youtube|v=CRuWvtMmPKw|300}}<ref>Brooke Larson. Fibular Repositioning Taping Technique. 2018. Available from: https://www.youtube.com/watch?v=CRuWvtMmPKw[last accessed 13/7/2022]</ref> | {{#ev:youtube|v=CRuWvtMmPKw|300}}<ref>Brooke Larson. Fibular Repositioning Taping Technique. 2018. Available from: https://www.youtube.com/watch?v=CRuWvtMmPKw[last accessed 13/7/2022]</ref> | ||
*The application of the Kinesio Taping Method in preventing ankle sprains | *The application of the Kinesio Taping Method in preventing ankle sprains had no effect on muscle activation of the peroneus (fibularis) longus<ref>Briem K, Eythörsdöttir H, Magnúsdóttir RG, Pálmarsson R, Rúnarsdöttir T, Sveinsson T. [https://www.jospt.org/doi/epdf/10.2519/jospt.2011.3501 Effects of Kinesio tape compared with nonelastic sports tape and the untaped ankle during a sudden inversion perturbation in male athletes.] J Orthop Sports Phys Ther. 2011 May;41(5):328-35.</ref> | ||
==== Braces ==== | ==== Braces ==== | ||
No significant effect was found on function and balance | No significant effect was found on function and balance when braces were applied.<ref name=":1" /> The following findings are of interest: | ||
* Barlow at al<ref>Barlow G, Donovan L, Hart JM, Hertel J. Effect of lace-up ankle braces on electromyography measures during walking in adults with chronic ankle instability. Physical Therapy in Sport. 2015 Feb 1;16(1):16-21.</ref> found that braces affect neuromuscular activity during walking which can assist | * Barlow at al.<ref>Barlow G, Donovan L, Hart JM, Hertel J. Effect of lace-up ankle braces on electromyography measures during walking in adults with chronic ankle instability. Physical Therapy in Sport. 2015 Feb 1;16(1):16-21.</ref> found that braces affect neuromuscular activity during walking, which can assist in decreasing sprains. | ||
* Feger at al<ref>Feger MA, Donovan L, Hart JM, Hertel J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127510/ Effect of ankle braces on lower extremity muscle activation during functional exercises in participants with chronic ankle instability]. Int J Sports Phys Ther. 2014 Aug;9(4):476-87</ref> | * Feger at al.<ref>Feger MA, Donovan L, Hart JM, Hertel J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127510/ Effect of ankle braces on lower extremity muscle activation during functional exercises in participants with chronic ankle instability]. Int J Sports Phys Ther. 2014 Aug;9(4):476-87</ref> investigated the effect of ankle braces on lower extremity muscle activities during functional exercises: | ||
** Forward lunge: reduction of muscle activity during pre‐initial contact in the lateral gastrocnemius and post‐initial contact in the peroneus longus. | ** Forward lunge: reduction of muscle activity during pre‐initial contact in the lateral gastrocnemius and post‐initial contact in the peroneus longus. | ||
** Star excursion: less muscle activity of the peroneus longus, lateral gastrocnemius, rectus femoris, and gluteus medius during balance anterior reach. | ** Star excursion balance test: less muscle activity of the peroneus longus, lateral gastrocnemius, rectus femoris, and gluteus medius during balance anterior reach. | ||
** Anterior reach: significant reduction of the thigh and total muscle activity | ** Anterior reach: significant reduction of the thigh muscles and total muscle activity. | ||
** Posterolateral reach: considerable reduction of gluteus medius activity | ** Posterolateral reach: considerable reduction of gluteus medius activity. | ||
** Single limb eyes closed balance, star excursion balance posteromedial reach, or during lateral hop exercises: no differences between braced and unbraced conditions | ** Single limb eyes closed balance, star excursion balance posteromedial reach, or during lateral hop exercises: no differences between braced and unbraced conditions. | ||
* Janssen et al<ref>Janssen KW, van Mechelen W, Verhagen EA. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-12-210 Ankles back in a randomized controlled trial (ABrCt): braces versus neuromuscular exercises for the secondary prevention of ankle sprains. Design of a randomised controlled trial.] BMC Musculoskelet Disord. 2011 Sep 27;12:210.</ref>submitted a protocol to assess the effect of braces vs. neuromuscular exercises.<ref name=":1" /> | * Janssen et al.<ref>Janssen KW, van Mechelen W, Verhagen EA. [https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-12-210 Ankles back in a randomized controlled trial (ABrCt): braces versus neuromuscular exercises for the secondary prevention of ankle sprains. Design of a randomised controlled trial.] BMC Musculoskelet Disord. 2011 Sep 27;12:210.</ref> submitted a protocol to assess the effect of braces vs. neuromuscular exercises.<ref name=":1" />According to their 2014 publication<ref name=":20">Janssen KW, van Mechelen W, Verhagen EA. [https://bjsm.bmj.com/content/48/16/1235.long Bracing superior to neuromuscular training for the prevention of self-reported recurrent ankle sprains: a three-arm randomised controlled trial]. Br J Sports Med. 2014 Aug;48(16):1235-9. </ref>: "bracing was found superior to neuromuscular training in reducing the incidence but not the severity of self-reported recurrent ankle sprains after usual care".<ref name=":20" /> | ||
* Fuerst | * Fuerst et al.<ref name=":17">Fuerst P, Gollhofer A, Wenning M, Gehring D. [https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-021-00452-0 People with chronic ankle instability benefit from brace application in the highly dynamic change of direction movements]. Journal of Foot and Ankle Research. 2021 Dec;14(1):1-1.</ref> argued that individuals with ankle instability may benefit from a semi-rigid ankle brace to keep ankle inversion angles "in a range that is comparable to values of healthy people".<ref name=":17" /> | ||
===== Therapeutic intervention ===== | ===== Therapeutic intervention ===== | ||
* Measurements to assess the effectiveness of using braces in patients with chronic ankle instability are not sensitive enough to assess dynamic stability<ref name=":1" /> | * Measurements to assess the effectiveness of using braces in patients with chronic ankle instability are not sensitive enough to assess dynamic stability.<ref name=":1" /> | ||
* | * Helene Simpson suggests to continue to use braces:<ref name=":1" /> | ||
** | ** Based on data from acute ankle sprains and prevention of recurrent sprains for one year post-injury | ||
** Cost-effectiveness and time efficiency | ** Cost-effectiveness and time efficiency | ||
| Line 212: | Line 213: | ||
''Flexibility:'' | ''Flexibility:'' | ||
Traditional concepts of flexibility exercises in chronic ankle instability include stretches of the soleus and gastrocnemius, performed 3 times for 30 seconds. <ref name=":1" /> | Traditional concepts of flexibility exercises in chronic ankle instability include stretches of the soleus and gastrocnemius, performed 3 times for 30 seconds.<ref name=":1" /> A new protocol suggests including plantar fascia stretches and walking backwards.<ref name=":18">Lee KY, Lee HJ, Kim SE, Choi PB, Song SH, Jee YS. Short-term rehabilitation and ankle instability. Int J Sports Med. 2012 Jun;33(6):485-96.</ref> Helene Simpson recommends neural roll-down and toe extension stretches (flexor hallucis longus and big toe extension).<ref name=":1" /> | ||
''Strength:'' | ''Strength:'' | ||
A meta-analysis by Arnold et al.<ref>Arnold BL, Linens SW, de la Motte SJ, Ross SE. [https://meridian.allenpress.com/jat/article/44/6/653/110976/Concentric-Evertor-Strength-Differences-and Concentric evertor strength differences and functional ankle instability: a meta-analysis]. J Athl Train. 2009 Nov-Dec;44(6):653-62. </ref> on concentric evertor strength deficits found: | |||
* No cause and effect between deficits and loss of functional stability | * No cause and effect between deficits and loss of functional stability | ||
* Not easy to detect evertor | * Not easy to detect evertor weakness | ||
* Isokinetic testing at slow speeds might | * Isokinetic testing at slow speeds might maximise differences | ||
* Weakness of invertors | * Weakness of invertors | ||
During strengthening exercises, muscle co-contraction is essential. Treatment protocols should include: | |||
* Bilateral calf raises | * Bilateral calf raises | ||
* Short foot exercises<ref name=":18" /> | * Short foot exercises<ref name=":18" /> | ||
Strength is important and should be included in rehabilitation. | |||
== Example Treatment Protocol == | == Example Treatment Protocol == | ||
Helene Simpson provides an example of her treatment protocol for the management of chronic ankle instability.<ref name=":1" /> | |||
=== General Principles === | === General Principles === | ||
| Line 237: | Line 237: | ||
#* The athlete takes on responsibility | #* The athlete takes on responsibility | ||
# Address postural stability | # Address postural stability | ||
# Include proximal stability, especially | # Include proximal stability, especially hip and knee joints | ||
# Focus on local stabilisers of the ankle and foot | # Focus on local stabilisers of the ankle and foot | ||
# Regaining dorsiflexion range of motion is a priority | # Regaining dorsiflexion range of motion is a priority | ||
| Line 252: | Line 252: | ||
* Walk | * Walk | ||
** Forwards and backwards | ** Forwards and backwards | ||
** Ladder: stride length, “Pink Panther”, heel-toe, big toe, | ** Ladder: stride length, “Pink Panther”, heel-toe, big toe, placing of the foot | ||
'''Postural Control/ Balance''' exercises to include: | '''Postural Control/ Balance''' exercises to include: | ||
| Line 284: | Line 284: | ||
* Single leg activity | * Single leg activity | ||
'''Balance training''' | '''Balance training''' | ||
* Aeroplane, | * Aeroplane, Star Excursion Balance Test | ||
* Bosu ball, Balance pad, Wobble board | * Bosu ball, Balance pad, Wobble board | ||
'''Shoe assessment''' | '''Shoe assessment''' | ||
| Line 306: | Line 306: | ||
[[Category:Ankle]] | [[Category:Ankle]] | ||
[[Category:Ankle - Conditions]] | [[Category:Ankle - Conditions]] | ||
[[Category:Plus Content]] | |||
Latest revision as of 18:06, 7 August 2023
Top Contributors - Ewa Jaraczewska, Jess Bell, Kim Jackson and Matt Huey
Definition of Chronic Ankle Instability (CAI)[edit | edit source]
Chronic ankle instability (CAI) has been defined as “repetitive bouts of lateral ankle instability resulting in numerous ankle sprains.”[1] Chronic instability refers to a feeling of apprehension in the ankle, “giving way” and recurrent ankle sprains, persisting for a minimum of six months after the initial sprain.[2] Symptoms include:[2]
- Lateral ankle pain
- Chronic swelling
- Difficulty walking on uneven terrain
Based on the International Classification of Function, Health and Disability (ICF) model, the effects of CAI on function and health include:
- In terms of impairments:[3]
- Increased ligamentous laxity
- Proprioceptive deficits
- In terms of activity limitations:[3]
- Inability to walk
- Inability to jump
- In terms of participation:[3]
- Cessation of sport
- Withdrawing from or decreasing occupational involvement
- Decreasing levels of exercise
- Change in the type of sport
Long-term Outcomes[edit | edit source]
Patients with CAI experience a reduction in their physical quality of life. Treatments may improve stability, but they take a long time and may require specialised equipment.[2] Konradsen et al.[4] conducted a study that followed-up with patients seven years post-ankle inversion trauma. They found the following:[4]
- 32% of patients reported chronic complaints of pain, swelling or recurrent sprains
- 72% of the subjects with residual disability reported that they were functionally impaired by their ankle
- 4% of patients experienced pain at rest and were severely disabled
- 19% were bothered by repeated inversion injuries
- 43% of these subjects felt that they could compensate by using an external ankle support
- 85% of people who develop CAI after unilateral sprain reported problems in the contralateral ankle
According to Hertel,[5] one sprain guarantees another.[2] And Struijs and Kerkhoffs[6] found that there was a 30% recurrence of sprains within a year of injury.[2]
Additional reported long-term outcomes include:
- Articular cartilage defects on the medial side of the joint due to:[2]
- Tearing of anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL)
- Altering and increasing peak cartilage strain
- Leading to tibiotalar cartilage degeneration (OA)
- Anterior talar positional fault[7]
- Altered movement patterns in unstable ankles:[2]
- Landing in more dorsiflexion in an attempt to minimise reliance on lateral ligaments and increase bony stability
- In drop jump: greater maximum calcaneal eversion and frontal displacement of the body
- Faster time to peak ground reaction force in drop landing
- Greater medial ground reaction force
- Metatarsal height is lowered during the terminal swing of gait
Mechanical and Functional Instability[edit | edit source]
There are two commonly accepted subgroups of CAI: mechanical instability and functional instability.[2][3] In Hertel's[8] model of ankle stability, mechanical and functional instability are part of a continuum. Recurrent sprains occur when both conditions are present.[8]
Mechanical Instability[edit | edit source]
Mechanical instability is referred to as pathological ligamentous laxity about the ankle-joint complex.[9] Mechanical instability may be caused by various anatomic changes that are present in isolation or in combination. They can lead to pathologies that are responsible for ankle instability.[3]
Functional Instability[edit | edit source]
There is no universally approved definition of functional ankle instability.[10] Based on the definition established by Evans et al.,[11] functional instability is a subjective complaint of weakness. Lentell et al.[12] describe functional instability as ankle pain and the perception that the injured ankle is less functional than the other ankle or less functional than pre-injury.[12] Tropp et al.[13] concluded that functional instability could be defined as a joint motion that does not exceed normal physiologic limits but is no longer controlled voluntarily.[13]
Impaired proprioceptive and neuromuscular control can be responsible for functional instability.[8]
Mechanical instability is typically presented as excessive inversion, laxity of the rear foot, and excessive anterior laxity of the talocrural joint. It can be caused by ligament instability or degenerative and chronic inflammatory process. In functional instability, on the other hand, patients complain about the sense of the ankle giving way. The delayed neuromuscular response, proprioceptive deficits or impaired balance can cause this symptom.
Table 1 summarises the causes and results of mechanical and functional ankle instability:[2]
Diagnostic Procedures[edit | edit source]
Diagnostic procedures can help clinicians confirm the presence of various ankle deficiencies, including reduced range of motion and perceived disability. This can help to define/diagnose a specific condition. Clinicians should consider if research findings suggest "consistent positive utility" before deciding which diagnostic tool to use:[14]
- Anterior drawer test: performed in slight knee flexion to relax the gastrocnemius. However, Kovaleski et al.[15] suggest testing with the knee flexed to 90° and the ankle at 10° of plantar flexion to isolate the anterior talofibular ligament.[15] A bilateral comparison is recommended.[14] Excessive anterior translation and a lack of a solid end feel indicate a positive test result.
- Stress radiography: used to quantify the extent of ankle-joint laxity. It shows the separation of the bony joint structures while a force is applied. Clinically, it helps to identify excessive strain within the ligamentous structures. A total anterior translation greater than 9 mm or translation greater than 5 mm (or both) when compared with the contralateral side indicates significant laxity of the anterior talofibular ligament. Pathologic laxity of the calcaneofibular ligament is demonstrated by a talar tilt angle greater than 10°, or an angle that is more than 5° greater than the contralateral limb.[14]
- MRI: not considered conclusive. Negative MRI results must be viewed with caution in a symptomatic patient and arthroscopy should be considered.[16]
- Diagnostic ultrasound: evidence suggests that diagnostic ultrasound offers a moderate to strong confirmation of lateral ligamentous injury.[17] It shows increased lateral ligament length during the anterior drawer and talar tilt tests in individuals with a history of CAI.[18]
- Stable force plates: suggested for gait and hop stability assessment:[19]
- Imaged guided injections of cortisone as a clinical diagnostic tool. The Delphi-based consensus of experts from the European Society of Musculoskeletal Radiology found that intraarticular foot and ankle anaesthetic injections performed under imaging guidance provide precise information about the source of pain.[21]
Physiotherapy Management[edit | edit source]
Conservative management is the treatment of choice for acute lateral ankle injuries - a surgical approach for these injuries is reserved for special cases.[22] Currently available conservative modalities include:[2]
- Neuromuscular training
- Balance training
- Mobilisation
- Neuromuscular control by peronei (theraband and isokinetic training do not affect ankle evertor strength)[2]
- Braces and taping
- Flexibility and strength training
Neuromuscular Training[edit | edit source]
- De Vries et al.[23] found that neuromuscular training alone has a positive short-term outcome and patients had better function.[23] This type of training is a key feature of the majority of conservative treatment regimes.[23][2]
- A study by Kim et al.[24] found that athletes with unstable ankles have an altered gait pattern - i.e. a relatively inverted ankle position during the initial contact and midstance. Engaging in six weeks of neuromuscular training immediately changed the athlete's ankle orientation to a relatively more inverted direction during jump landing. However, there was no effect on walking and running.[24]
- According to Guzmán-Muñoz et al.,[25] four weeks of neuromuscular training improved postural control in college volleyball players with functional ankle instability (FAI) .[25]
Guide to Neuromuscular Training[edit | edit source]
Neuromuscular training is an "unconscious activation of dynamic restraints in preparation and in response to joint motion and loads to maintain and restore functional joint stability".[2]
Goals of neuromuscular training:
Exercises[edit | edit source]
Exercises are performed in closed chain and functional positions:
- Single limb stance on wobble board or balance mat
- Single limb ball toss
- Single leg theraband kicks and step downs (see Figures with Steps 1-3)
Balance Training[edit | edit source]
- While investigating functional ankle instability and health-related quality of life, Arnold et al.[27] concluded that balance training can affect multiple joints and produce overall improvements.[2]
- McKeon et al.[19] showed that balance training significantly improves static postural control and dynamic postural control.[2]
- A prospective cohort study by Sefton et al.[28] found that rehabilitation affects sensorimotor system function.[2]
- Based on a review of randomised controlled trials, Mollà Casanova et al.[29] concluded that balance training significantly improves functionality, instability, and dynamic balance outcomes in people with chronic ankle instability.[29]
Guide to Balance Training[edit | edit source]
The literature indicates that the following balance measures should guide clinical practice. However, De Vries et al.[23] did not find a correlation with function:
- Centre-of-pressure (COP) excursion[30]
- Time-to-boundary (TTB) after landing[31]
- Peak plantar analysis[32]
- Star Excursion Balance Test (SEBT)
Proprioception[edit | edit source]
Kinesthesia and joint position sense (JPS) are usually impaired in patients with chronic ankle instability.[33] The testing methodology for proprioception includes:
- Kinesthesia: assessed using threshold-to-detection of passive motion[2]
- Joint position sense: assessed using active and passive joint placing reproduction[2]
Therapeutic Interventions[edit | edit source]
- Multi-station exercise regime once per week[2]
- Ankle disc training, balance pad
- Perturbation exercises with elastic tubing[34][2]
- Four exercises including front pull, back pull, crossover and reverse crossover, performed 3 times per week. The standard protocol includes 3 sets of 15 repetitions with a resistance band while standing on the affected leg
- Goal: to maintain alignment and stability
- Outcome: balance improved in 4 weeks
Mobilisation[edit | edit source]
- Limited ankle dorsiflexion during jogging and walking gait is considered a risk factor for recurrent sprains because of the following:[2]
- Inability to reach the closed-packed position of the ankle joint during stance
- Tendency to lock midfoot in supination
- The centre of gravity moves laterally, thus the ankle joint becomes vulnerable to supination and a sprain
- According to Westad et al.,[35] mobilisation with movement (MWM) techniques used to treat peripheral joints were superior to a placebo, but not to other medical or physiotherapy interventions.[35]
- The results of a systematic review and meta-analysis by Weerasekara et al.[36] suggest that a mobilisation with movement intervention immediately benefitted patients with chronic ankle instability by increasing dorsiflexion range of motion.[36]
Therapeutic Interventions[edit | edit source]
Mulligan’s mobilisation with movement (MWM) technique should include the following:
- Fibular glide at distal and proximal tibiofibular joint
- Talar glide
Helene Simpson also recommends using an MWM technique that includes midfoot mobility at the navicular.[2]
Braces and Taping[edit | edit source]
Taping[edit | edit source]
- Delahunt et al.[38] found no change in “actual” stability, but patients' perceptions of stability were significantly improved (56%).[2]
- Hopper et al.[39] found that Mulligan taping had no impact on neuromuscular control during static and dynamic balance.[2]
Therapeutic Intervention[edit | edit source]
The following taping techniques were clinically assessed:[2]
- Lateral subtalar sling (aimed at resisting subtalar inversion)
- Fibular repositioning,[41] but the exact mechanism for reducing the incidence of sprains is unknown
- The application of the Kinesio Taping Method in preventing ankle sprains had no effect on muscle activation of the peroneus (fibularis) longus[43]
Braces[edit | edit source]
No significant effect was found on function and balance when braces were applied.[2] The following findings are of interest:
- Barlow at al.[44] found that braces affect neuromuscular activity during walking, which can assist in decreasing sprains.
- Feger at al.[45] investigated the effect of ankle braces on lower extremity muscle activities during functional exercises:
- Forward lunge: reduction of muscle activity during pre‐initial contact in the lateral gastrocnemius and post‐initial contact in the peroneus longus.
- Star excursion balance test: less muscle activity of the peroneus longus, lateral gastrocnemius, rectus femoris, and gluteus medius during balance anterior reach.
- Anterior reach: significant reduction of the thigh muscles and total muscle activity.
- Posterolateral reach: considerable reduction of gluteus medius activity.
- Single limb eyes closed balance, star excursion balance posteromedial reach, or during lateral hop exercises: no differences between braced and unbraced conditions.
- Janssen et al.[46] submitted a protocol to assess the effect of braces vs. neuromuscular exercises.[2]According to their 2014 publication[47]: "bracing was found superior to neuromuscular training in reducing the incidence but not the severity of self-reported recurrent ankle sprains after usual care".[47]
- Fuerst et al.[48] argued that individuals with ankle instability may benefit from a semi-rigid ankle brace to keep ankle inversion angles "in a range that is comparable to values of healthy people".[48]
Therapeutic intervention[edit | edit source]
- Measurements to assess the effectiveness of using braces in patients with chronic ankle instability are not sensitive enough to assess dynamic stability.[2]
- Helene Simpson suggests to continue to use braces:[2]
- Based on data from acute ankle sprains and prevention of recurrent sprains for one year post-injury
- Cost-effectiveness and time efficiency
Flexibility and Strength Training[edit | edit source]
Flexibility:
Traditional concepts of flexibility exercises in chronic ankle instability include stretches of the soleus and gastrocnemius, performed 3 times for 30 seconds.[2] A new protocol suggests including plantar fascia stretches and walking backwards.[49] Helene Simpson recommends neural roll-down and toe extension stretches (flexor hallucis longus and big toe extension).[2]
Strength:
A meta-analysis by Arnold et al.[50] on concentric evertor strength deficits found:
- No cause and effect between deficits and loss of functional stability
- Not easy to detect evertor weakness
- Isokinetic testing at slow speeds might maximise differences
- Weakness of invertors
During strengthening exercises, muscle co-contraction is essential. Treatment protocols should include:
- Bilateral calf raises
- Short foot exercises[49]
Strength is important and should be included in rehabilitation.
Example Treatment Protocol[edit | edit source]
Helene Simpson provides an example of her treatment protocol for the management of chronic ankle instability.[2]
General Principles[edit | edit source]
- Goal setting is critical
- Team effort
- The athlete takes on responsibility
- Address postural stability
- Include proximal stability, especially hip and knee joints
- Focus on local stabilisers of the ankle and foot
- Regaining dorsiflexion range of motion is a priority
- Include cardio-vascular fitness
- Integrate exercises into the gym to improve compliance
- Assess footwear and sports-specific technique
Phase 1[edit | edit source]
Cardio-vascular fitness to include:
- Cycling
- Hydrotherapy or swimming
- Walk
- Forwards and backwards
- Ladder: stride length, “Pink Panther”, heel-toe, big toe, placing of the foot
Postural Control/ Balance exercises to include:
- Pilates
- Short foot exercises
- Tibialis posterior re-education
Strengthening exercises to include:
- Leg press
- Calf raises, theraband exercises
- Hamstring curls
- Bridging (glutes)
- Abdominal
- Neurodynamics and Flexibility
Phase 2[edit | edit source]
Cardio-vascular fitness
- Running
- Elliptical
- Stepper
- Rowing machine
Functional strength
- Modified lunges
- Squats: bilateral, single leg
- Single leg activity
Balance training
- Aeroplane, Star Excursion Balance Test
- Bosu ball, Balance pad, Wobble board
Shoe assessment
Phase 3[edit | edit source]
Cardio-vascular
- Sport-specific drills and skills
- Endurance
- Terrain
Balance/ function/ agility
- Jumping, skipping, landing
- Multiple hops
- Vertical jumps
Integration of sport specific activities, but without compromising the quality of movement.
Pain monitoring
References[edit | edit source]
- ↑ Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train. 2002 Dec;37(4):364-375.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 2.24 2.25 2.26 2.27 2.28 2.29 2.30 2.31 2.32 2.33 Simpson H. Chronic Ankle Instability Course. Physiopedia 2022
- ↑ 3.0 3.1 3.2 3.3 3.4 Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. Journal of athletic training. 2011 Mar;46(2):133-41.
- ↑ 4.0 4.1 Konradsen L, Bech L, Ehrenbjerg M, Nickelsen T. Seven years follow-up after ankle inversion trauma. Scand J Med Sci Sports. 2002 Jun;12(3):129-35.
- ↑ Hertel J. Immobilisation for acute severe ankle sprain. Lancet. 2009 Feb 14;373(9663):524-6.
- ↑ Struijs PA, Kerkhoffs GM. Ankle sprain. BMJ Clin Evid. 2010 May 13;2010:1115.
- ↑ Wikstrom EA, Hubbard TJ. Talar positional fault in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010 Aug;91(8):1267-71.
- ↑ 8.0 8.1 8.2 Hertel J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J Athl Train. 2002 Dec;37(4):364-375
- ↑ Tropp H. Commentary: Functional Ankle Instability Revisited. J Athl Train. 2002 Dec;37(4):512-515.
- ↑ Konradsen L. Factors Contributing to Chronic Ankle Instability: Kinesthesia and Joint Position Sense. J Athl Train. 2002 Dec;37(4):381-385.
- ↑ Evans GA, Hardcastle P, Frenyo AD. Acute rupture of the lateral ligament of the ankle. To suture or not to suture? J Bone Joint Surg Br. 1984 Mar;66(2):209-12
- ↑ 12.0 12.1 Lentell G, Katzman LL, Walters MR. The Relationship between Muscle Function and Ankle Stability. J Orthop Sports Phys Ther. 1990;11(12):605-11.
- ↑ 13.0 13.1 Tropp H, Odenrick P, Gillquist J. Stabilometry recordings in functional and mechanical instability of the ankle joint. Int J Sports Med. 1985 Jun;6(3):180-2.
- ↑ 14.0 14.1 14.2 Gribble PA. Evaluating and differentiating ankle instability. Journal of athletic training. 2019 Jun;54(6):617-27.
- ↑ 15.0 15.1 Kovaleski JE, Norrell PM, Heitman RJ, Hollis JM, Pearsall AW. Knee and ankle position, anterior drawer laxity, and stiffness of the ankle complex. J Athl Train. 2008 May-Jun;43(3):242-8.
- ↑ Joshy S, Abdulkadir U, Chaganti S, Sullivan B, Hariharan K. Accuracy of MRI scan in the diagnosis of ligamentous and chondral pathology in the ankle. Foot Ankle Surg. 2010 Jun;16(2):78-80.
- ↑ Oae K, Takao M, Uchio Y, Ochi M. Evaluation of anterior talofibular ligament injury with stress radiography, ultrasonography and MR imaging. Skeletal Radiol. 2010 Jan;39(1):41-7.
- ↑ Croy T, Saliba SA, Saliba E, Anderson MW, Hertel J. Differences in lateral ankle laxity measured via stress ultrasonography in individuals with chronic ankle instability, ankle sprain copers, and healthy individuals. J Orthop Sports Phys Ther. 2012 Jul;42(7):593-600.
- ↑ 19.0 19.1 McKeon PO, Ingersoll CD, Kerrigan DC, Saliba E, Bennett BC, Hertel J. Balance training improves function and postural control in those with chronic ankle instability. Med Sci Sports Exerc. 2008 Oct;40(10):1810-9.
- ↑ Vicon. Vicon Gait and Posture Biomechanics. 2018. Available from: https://www.youtube.com/watch?v=D6JMr-ZPbjQ [last accessed 9/07/2022]
- ↑ Sconfienza LM, Adriaensen M, Albano D, Alcala-Galiano A, Allen G, et al. Clinical indications for image-guided interventional procedures in the musculoskeletal system: a Delphi-based consensus paper from the European Society of Musculoskeletal Radiology (ESSR)-part VI, foot and ankle. Eur Radiol. 2022 Feb;32(2):1384-94.
- ↑ Aicale R, Maffulli N. Chronic lateral ankle instability: a topical review. Foot & Ankle International. 2020 Dec;41(12):1571-81.
- ↑ 23.0 23.1 23.2 23.3 de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011 Aug 10;(8):CD004124.
- ↑ 24.0 24.1 Kim E, Choi H, Cha JH, Park JC, Kim T. Effects of Neuromuscular Training on the Rear-foot Angle Kinematics in Elite Women Field Hockey Players with Chronic Ankle Instability. J Sports Sci Med. 2017 Mar 1;16(1):137-146.
- ↑ 25.0 25.1 Guzmán-Muñoz E, Daigre-Prieto M, Soto-Santander K, Concha-Cisternas Y, Méndez-Rebolledo G, Sazo-Rodríguez S, Valdés-Badilla P. The effects of neuromuscular training on the postural control of university volleyball players with functional ankle instability: A pilot study. Archivos de medicina del deporte. 2019;35(5):283-7
- ↑ Loudon JK, Santos MJ, Franks L, Liu W. The effectiveness of active exercise as an intervention for functional ankle instability: a systematic review. Sports Med. 2008;38(7):553-63.
- ↑ Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011 Nov-Dec;46(6):634-41.
- ↑ Sefton JM, Yarar C, Hicks-Little CA, Berry JW, Cordova ML. Six weeks of balance training improves sensorimotor function in individuals with chronic ankle instability. J Orthop Sports Phys Ther. 2011 Feb;41(2):81-9.
- ↑ 29.0 29.1 Mollà-Casanova S, Inglés M, Serra-Añó P. Effects of balance training on functionality, ankle instability, and dynamic balance outcomes in people with chronic ankle instability: systematic review and meta-analysis. Clinical Rehabilitation. 2021 Dec;35(12):1694-709.
- ↑ Yousefi M, Sadeghi H, Ilbiegi S, Ebrahimabadi Z, Kakavand M, Wikstrom EA. Center of pressure excursion and muscle activation during gait initiation in individuals with and without chronic ankle instability. Journal of Biomechanics,2020, 18.
- ↑ Hertel J, Olmsted-Kramer LC, Challis JH. Time-to-boundary measures of postural control during single-leg quiet standing. J Appl Biomech. 2006 Feb;22(1):67-73.
- ↑ Orlin MN, McPoil TG. Plantar Pressure Assessment. Physical Therapy 2000; 80( 4): 399–409
- ↑ Ma T, Li Q, Song Y, Hua Y. Chronic ankle instability is associated with proprioception deficits: a systematic review and meta-analysis. Journal of sport and health science. 2021 Mar 1;10(2):182-91.
- ↑ Han K, Ricard MD, Fellingham GW. Effects of a 4-week exercise program on balance using elastic tubing as a perturbation force for individuals with a history of ankle sprains. J Orthop Sports Phys Ther. 2009 Apr;39(4):246-55.
- ↑ 35.0 35.1 Westad K, Tjoestolvsen F, Hebron C. The effectiveness of Mulligan's mobilisation with movement (MWM) on peripheral joints in musculoskeletal (MSK) conditions: A systematic review. Musculoskeletal Science and Practice. 2019 Feb 1;39:157-63
- ↑ 36.0 36.1 Weerasekara I, Deam H, Bamborough N, Brown S, Donnelly J, Thorp N, Rivett DA. Effect of Mobilisation with Movement (MWM) on clinical outcomes in lateral ankle sprains: a systematic review and meta-analysis. The Foot. 2020 Jun 1;43:101657.
- ↑ Hubbard TJ, Cordova M. Effect of ankle taping on mechanical laxity in chronic ankle instability. Foot Ankle Int. 2010 Jun;31(6):499-504.
- ↑ Delahunt E, McGrath A, Doran N, Coughlan GF. Effect of taping on actual and perceived dynamic postural stability in persons with chronic ankle instability. Arch Phys Med Rehabil. 2010 Sep;91(9):1383-9.
- ↑ Hopper D, Samsson K, Hulenik T, Ng C, Hall T, Robinson K. The influence of Mulligan ankle taping during balance performance in subjects with unilateral chronic ankle instability. Phys Ther Sport. 2009 Nov;10(4):125-30.
- ↑ UCO GATP. Sunderland Special Strip 2 SubTalar Sling - Side View. 2017. Available from: https://www.youtube.com/watch?v=hTQjt7vGNCw [last accessed 13/7/2022]
- ↑ Moiler K, Hall T, Robinson K. The role of fibular tape in the prevention of ankle injury in basketball: A pilot study. J Orthop Sports Phys Ther. 2006 Sep;36(9):661-8.
- ↑ Brooke Larson. Fibular Repositioning Taping Technique. 2018. Available from: https://www.youtube.com/watch?v=CRuWvtMmPKw[last accessed 13/7/2022]
- ↑ Briem K, Eythörsdöttir H, Magnúsdóttir RG, Pálmarsson R, Rúnarsdöttir T, Sveinsson T. Effects of Kinesio tape compared with nonelastic sports tape and the untaped ankle during a sudden inversion perturbation in male athletes. J Orthop Sports Phys Ther. 2011 May;41(5):328-35.
- ↑ Barlow G, Donovan L, Hart JM, Hertel J. Effect of lace-up ankle braces on electromyography measures during walking in adults with chronic ankle instability. Physical Therapy in Sport. 2015 Feb 1;16(1):16-21.
- ↑ Feger MA, Donovan L, Hart JM, Hertel J. Effect of ankle braces on lower extremity muscle activation during functional exercises in participants with chronic ankle instability. Int J Sports Phys Ther. 2014 Aug;9(4):476-87
- ↑ Janssen KW, van Mechelen W, Verhagen EA. Ankles back in a randomized controlled trial (ABrCt): braces versus neuromuscular exercises for the secondary prevention of ankle sprains. Design of a randomised controlled trial. BMC Musculoskelet Disord. 2011 Sep 27;12:210.
- ↑ 47.0 47.1 Janssen KW, van Mechelen W, Verhagen EA. Bracing superior to neuromuscular training for the prevention of self-reported recurrent ankle sprains: a three-arm randomised controlled trial. Br J Sports Med. 2014 Aug;48(16):1235-9.
- ↑ 48.0 48.1 Fuerst P, Gollhofer A, Wenning M, Gehring D. People with chronic ankle instability benefit from brace application in the highly dynamic change of direction movements. Journal of Foot and Ankle Research. 2021 Dec;14(1):1-1.
- ↑ 49.0 49.1 Lee KY, Lee HJ, Kim SE, Choi PB, Song SH, Jee YS. Short-term rehabilitation and ankle instability. Int J Sports Med. 2012 Jun;33(6):485-96.
- ↑ Arnold BL, Linens SW, de la Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J Athl Train. 2009 Nov-Dec;44(6):653-62.