Alberta Infant Motor Scale (AIMS): Difference between revisions
No edit summary |
No edit summary |
||
| (20 intermediate revisions by 4 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Objective == | == Objective == | ||
The Alberta Infant Motor Scale (AIMS) is a | The Alberta Infant Motor Scale (AIMS) is a standardised observational examination tool used to assess the maturation of gross motor skills of infants from term (i.e. 40 weeks gestation) to 18 months post-term. The AIMS was developed as a reference guide for the development of infants based on the age related norms of 2200 infants in Alberta, Canada.<ref name=":0">Piper MC, Pinnell LE, Darrah J, Maguire T, Byrne PJ. Construction and validation of the Alberta Infant Motor Scale (AIMS). Can J Public Health. 1992; 83: 46-50.</ref><ref name=":1">Piper MC, Darrah J, editors. Motor assessment of the developing infant. 2<sup>nd</sup> edition. St. Louis, Missouri: Elsevier, Inc., 2022.</ref> | ||
It can be used as a screening tool to detect and track early developmental delays.<ref name=":2">Darrah J, Piper M, Watt MJ. Assessment of gross motor skills of at‐risk infants: predictive validity of the Alberta Infant Motor Scale. Developmental medicine & child neurology. 1998 Jul;40(7):485-91.</ref> <ref name=":3">Albuquerque PL, Lemos A, Guerra MQ, Eickmann SH. Accuracy of the Alberta Infant Motor Scale (AIMS) to detect developmental delay of gross motor skills in preterm infants: a systematic review. Developmental neurorehabilitation. 2015 Jan 2;18(1):15-21.</ref> | It can be used as a screening tool to detect and track early developmental delays.<ref name=":2">Darrah J, Piper M, Watt MJ. Assessment of gross motor skills of at‐risk infants: predictive validity of the Alberta Infant Motor Scale. Developmental medicine & child neurology. 1998 Jul;40(7):485-91.</ref> <ref name=":3">Albuquerque PL, Lemos A, Guerra MQ, Eickmann SH. Accuracy of the Alberta Infant Motor Scale (AIMS) to detect developmental delay of gross motor skills in preterm infants: a systematic review. Developmental neurorehabilitation. 2015 Jan 2;18(1):15-21.</ref> It compares a child's level of motor development against the expected norms for their age in four categories: prone, supine, sitting and standing. | ||
== Intended Population == | == Intended Population == | ||
The AIMS can be used with all infants | [[File:Aims 1.jpg|thumb|alt=|'''Figure.1''' Infant Crawling<ref>Flickr. Thomas Life Crawling. Available from: https://www.flickr.com/photos/thomaslife/2839828469 (accessed 20 July 2022).</ref>]] | ||
The AIMS can be used with all infants aged under 18 months to identify delays or changes in motor skill development. It may be used for infants who:<ref name=":1" /><ref name=":2" /> | |||
* show typical development with no medical concerns | * show typical development with no medical concerns | ||
* | * do not have specific factors in their history, but motor development delays are suspected | ||
* are at higher risk of developmental delay due to | * are at higher risk of developmental delay due to genetic, prenatal, perinatal, neonatal, postnatal, or environmental complications | ||
* have been given a specific diagnosis that | * have been given a specific diagnosis that affects motor skill development (e.g., [[Down Syndrome (Trisomy 21)|Down syndrome]], [[Bronchopulmonary Dysplasia|bronchopulmonary dysplasia]]) | ||
<br> | |||
The AIMS should <u>NOT</u> be used for infants who use altered movement patterns to compensate for functional limitations (e.g., paralysis, [[Spina Bifida|spina bifida]], hypotonia, muscle spasticity) as their unique motor development improvements may not be reflected in the AIMS.<ref name=":1" /> | The AIMS should <u>NOT</u> be used for infants who use altered movement patterns to compensate for functional limitations (e.g., paralysis, [[Spina Bifida|spina bifida]], hypotonia, muscle spasticity) as their unique motor development improvements may not be reflected in the AIMS.<ref name=":1" /> | ||
=== Tool Description === | === Tool Description === | ||
The AIMS is a 58-item observational scoring tool. These | [[File:Aims 2.jpg|thumb|300x300px|alt=|'''Figure.2''' Infant Prone Push Up <ref>Flickr. Thomas Life Cutie Pie. Available from: https://www.flickr.com/photos/thomaslife/2635755242/<nowiki/>(accessed 20 July 2022</ref>]]The AIMS is a 58-item observational scoring tool. These items are divided into four position-centric sub-scales<ref name=":0" />: | ||
# Prone (21 items) | # Prone (21 items) | ||
| Line 28: | Line 30: | ||
=== Equipment Required === | === Equipment Required === | ||
* AIMS Manual | |||
* AIMS | * AIMS Score Sheet and Graph | ||
* Examining table or other raised surface for younger infants | * Examining table or other raised surface for younger infants | ||
* Firm mat or carpet for older infants | * Firm mat or carpet for older infants | ||
| Line 36: | Line 38: | ||
=== Set-up === | === Set-up === | ||
The AIMS can be conducted in the home or | The AIMS can be conducted in the home or clinic. The assessment for younger infants can be performed on an examining table or raised surface. For older infants, the assessment should be conducted on a firm mat or carpeted area of the floor.<ref name=":1" /> | ||
== Method of Use == | == Method of Use == | ||
It is important that the assessor familiarise themselves with the administration and scoring guidelines of the AIMS prior to the assessment. The assessment takes a maximum of 20-30 minutes to complete. The assessor observes the motor patterns of the infant and compares them to the scale sheet.<ref name=":0" /><ref name=":1" /> | |||
=== Scoring === | === Scoring === | ||
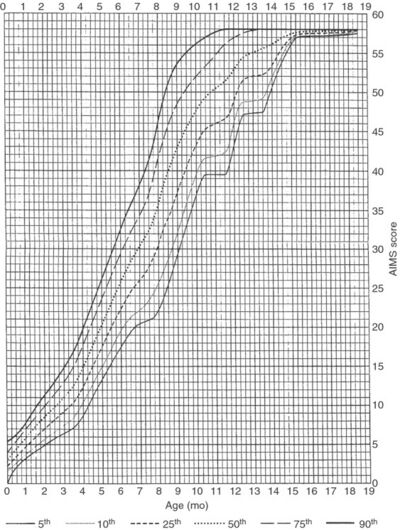
[[File:AIMS graph.jpg|thumb|530x530px|'''Figure 3''': Alberta Infant Motor Scale (AIMS) Centile Ranks Graph.<ref name=":3" />|alt=]]The assessor will preferably complete the scoring after the assessment has finished. | |||
The scoring sheet consists of a photo and a short description of the movement being assessed.<ref name=":1" /> The movements begin with the most basic presentations of prone lying, supine lying, sitting, and standing and progress incrementally to more advanced movements.<ref name=":0" /> | |||
During the assessment, the evaluator observes the movements of the child and scores each movement component as either “observed” or “not observed”. There is no option to score the patient on ‘emerging’ movement patterns. The patient should not be accredited for items reported by | During the assessment, the evaluator observes the movements of the child and scores each movement component as either “observed” or “not observed”. There is no option to score the patient on ‘emerging’ movement patterns. The patient <u>should not</u> be accredited for items reported by parents / caregivers. | ||
The | The least advanced and most advanced movements observed in a given position (prone, supine, sitting, standing) create the ‘motor window’ for the patient in that position. All movements within the motor window for each position must be recorded as "observed" (O) or "not observed" (NO).<ref name=":1" /> | ||
The assessor scores the patient one point for each movement that is “observed” within each motor window. The accumulative score of all four positions provides the 'total score'. The total score is recorded against the corrected gestational age of the patient on a graph of normative data for infant motor function. The graph in ''Figure 3'' contains the percentile (5<sup>th</sup>, 10<sup>th</sup>, 25<sup>th</sup>, 50<sup>th</sup>, 75<sup>th</sup>, 90<sup>th</sup>) norms of infant motor function. The assessor determines at which percentile of motor development the patient is for their age based on the graphed normative values and records it on the scoring sheet.<ref name=":0" /><ref name=":1" /> | |||
== Evidence == | == Evidence == | ||
=== Standardisation === | |||
The data used to develop the AIMS was based on the assessments of 2202 infants aged less than 18 months who were living in Alberta, Canada between 1990 and 1992.<ref name=":0" /> The normative values from this group were expressed as the mean, standard deviation, and percentile rank for the total score for each month of age, and time norms for the achievement of each item.<ref name=":5" /> These reference figures and norms with percentile ranks are accessible in the AIMS Manual.<ref name=":5">Eliks M, Gajewska E. [https://www.frontiersin.org/articles/10.3389/fneur.2022.927502/full The Alberta Infant Motor Scale: A tool for the assessment of motor aspects of neurodevelopment in infancy and early childhood.] Frontiers in Neurology. 2022;13.</ref> | |||
The interrater and test-retest reliability of the original scale and was found to be 0.99.<ref name=":5" /> The concurrent validity of the original scale was assessed against the Bayley Scales of Infant and Toddler Development (BSID) and the Peabody Development Motor Scales (PDSM). Concurrent validity with the BSID was 0.98, and 0.97 with the PDSM.<ref name=":5" /> | |||
Re-evaluation of the scale was performed in 2014.<ref name=":5" /> Developmental norms were assessed in 650 infants from Alberta over a two year period.<ref name=":4">Darrah J, Bartlett D, Maguire TO, Avison WR, Lacaze‐Masmonteil T. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4293464/ Have infant gross motor abilities changed in 20 years? A re‐evaluation of the Alberta Infant Motor Scale normative values]. Developmental Medicine & Child Neurology. 2014 Sep;56(9):877-81.</ref> Darrah et al.<ref name=":4" /> reported a correlation coefficient of 0.99 between the original and re-evaluation groups, and concluded that the validity of the initial research was unchanged.<ref name=":4" /> | |||
Normative development of infants in other countries have been assessed using the AIMS. Results from these studies have formed population-specific normative values for several of these countries, such as Netherlands,<ref>van Iersel PA, la Bastide-van Gemert S, Wu YC, Hadders-Algra M. Alberta Infant Motor Scale: Cross-cultural analysis of gross motor development in Dutch and Canadian infants and introduction of Dutch norms. Early Human Development. 2020 Dec 1;151:105239.</ref> Brazil,<ref>Gontijo AP, de Melo Mambrini JV, Mancini MC. Cross-country validity of the Alberta Infant Motor Scale using a Brazilian sample. Brazilian Journal of Physical Therapy. 2021 Jul 1;25(4):444-9.</ref><ref>Valentini NC, Saccani R. Brazilian validation of the alberta infant motor scale. Physical therapy. 2012 Mar 1;92(3):440-7.</ref> Serbia,<ref>Lackovic M, Nikolic D, Filimonovic D, Petronic I, Mihajlovic S, Golubovic Z, Pavicevic P, Cirovic D. Reliability, consistency and temporal stability of Alberta Infant Motor Scale in Serbian infants. Children. 2020 Mar 2;7(3):16.</ref> Korea,<ref>Ko J, Lim HK. Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis. International Journal of Environmental Research and Public Health. 2022 Feb 4;19(3):1767.</ref> Greece,<ref>Syrengelas D, Kalampoki V, Kleisiouni P, Manta V, Mellos S, Pons R, Chrousos GP, Siahanidou T. Alberta Infant Motor Scale (AIMS) performance of greek preterm infants: comparisons with full-term infants of the same nationality and impact of prematurity-related morbidity factors. Physical therapy. 2016 Jul 1;96(7):1102-8.</ref> Poland,<ref>Eliks M, Sowińska A, Gajewska E. The Polish version of the Alberta Infant Motor Scale: cultural adaptation and validation. Frontiers in Neurology.:1504.</ref> Spain,<ref>Morales-Monforte E, Bagur-Calafat C, Suc-Lerin N, Fornaguera-Martí M, Cazorla-Sánchez E, Girabent-Farrés M. The Spanish version of the Alberta infant motor scale: validity and reliability analysis. Developmental Neurorehabilitation. 2017 Feb 17;20(2):76-82.</ref> Thailand,<ref>Aimsamrarn P, Janyachareon T, Rattanathanthong K, Emasithi A, Siritaratiwat W. Cultural translation and adaptation of the Alberta Infant Motor Scale Thai version. Early Human Development. 2019 Mar 1;130:65-70.</ref> and Taiwan.<ref>Jeng SF, Yau KI, Chen LC, Hsiao SF. Alberta infant motor scale: reliability and validity when used on preterm infants in Taiwan. Physical therapy. 2000 Feb 1;80(2):168-78.</ref> | |||
=== Resources === | |||
== Resources == | |||
{{#ev:youtube|5QTnUqdZSbA|250}} <div class="row"><div class="col-md-6 col-md-offset-3"><div class="text-right"><ref>Warren McAdams, PT, DPT. Alberta Infant motor Scale (AIMS). Available from: https://youtu.be/5QTnUqdZSbA[last accessed 22/07/22]</ref></div></div></div> | {{#ev:youtube|5QTnUqdZSbA|250}} <div class="row"><div class="col-md-6 col-md-offset-3"><div class="text-right"><ref>Warren McAdams, PT, DPT. Alberta Infant motor Scale (AIMS). Available from: https://youtu.be/5QTnUqdZSbA[last accessed 22/07/22]</ref></div></div></div> | ||
== References == | == References == | ||
<references /> | |||
[[Category:Paediatrics]] | |||
[[Category:Paediatrics - Outcome Measures]] | |||
[[Category:Course Pages]] | |||
Latest revision as of 02:57, 22 May 2023
Original Editor - Padraig O Beaglaoich
Top Contributors - Padraig O Beaglaoich, Naomi O'Reilly, Robin Tacchetti and Jess Bell
Objective[edit | edit source]
The Alberta Infant Motor Scale (AIMS) is a standardised observational examination tool used to assess the maturation of gross motor skills of infants from term (i.e. 40 weeks gestation) to 18 months post-term. The AIMS was developed as a reference guide for the development of infants based on the age related norms of 2200 infants in Alberta, Canada.[1][2]
It can be used as a screening tool to detect and track early developmental delays.[3] [4] It compares a child's level of motor development against the expected norms for their age in four categories: prone, supine, sitting and standing.
Intended Population[edit | edit source]

The AIMS can be used with all infants aged under 18 months to identify delays or changes in motor skill development. It may be used for infants who:[2][3]
- show typical development with no medical concerns
- do not have specific factors in their history, but motor development delays are suspected
- are at higher risk of developmental delay due to genetic, prenatal, perinatal, neonatal, postnatal, or environmental complications
- have been given a specific diagnosis that affects motor skill development (e.g., Down syndrome, bronchopulmonary dysplasia)
The AIMS should NOT be used for infants who use altered movement patterns to compensate for functional limitations (e.g., paralysis, spina bifida, hypotonia, muscle spasticity) as their unique motor development improvements may not be reflected in the AIMS.[2]
Tool Description[edit | edit source]

The AIMS is a 58-item observational scoring tool. These items are divided into four position-centric sub-scales[1]:
- Prone (21 items)
- Supine (9 items)
- Sitting (12 items)
- Standing (16 items)
Equipment Required[edit | edit source]
- AIMS Manual
- AIMS Score Sheet and Graph
- Examining table or other raised surface for younger infants
- Firm mat or carpet for older infants
- Low bench or chair for some items on the scale
- Toys appropriate for infants younger than 18 months[2]
Set-up[edit | edit source]
The AIMS can be conducted in the home or clinic. The assessment for younger infants can be performed on an examining table or raised surface. For older infants, the assessment should be conducted on a firm mat or carpeted area of the floor.[2]
Method of Use[edit | edit source]
It is important that the assessor familiarise themselves with the administration and scoring guidelines of the AIMS prior to the assessment. The assessment takes a maximum of 20-30 minutes to complete. The assessor observes the motor patterns of the infant and compares them to the scale sheet.[1][2]
Scoring[edit | edit source]
The assessor will preferably complete the scoring after the assessment has finished.
The scoring sheet consists of a photo and a short description of the movement being assessed.[2] The movements begin with the most basic presentations of prone lying, supine lying, sitting, and standing and progress incrementally to more advanced movements.[1]
During the assessment, the evaluator observes the movements of the child and scores each movement component as either “observed” or “not observed”. There is no option to score the patient on ‘emerging’ movement patterns. The patient should not be accredited for items reported by parents / caregivers.
The least advanced and most advanced movements observed in a given position (prone, supine, sitting, standing) create the ‘motor window’ for the patient in that position. All movements within the motor window for each position must be recorded as "observed" (O) or "not observed" (NO).[2]
The assessor scores the patient one point for each movement that is “observed” within each motor window. The accumulative score of all four positions provides the 'total score'. The total score is recorded against the corrected gestational age of the patient on a graph of normative data for infant motor function. The graph in Figure 3 contains the percentile (5th, 10th, 25th, 50th, 75th, 90th) norms of infant motor function. The assessor determines at which percentile of motor development the patient is for their age based on the graphed normative values and records it on the scoring sheet.[1][2]
Evidence[edit | edit source]
Standardisation[edit | edit source]
The data used to develop the AIMS was based on the assessments of 2202 infants aged less than 18 months who were living in Alberta, Canada between 1990 and 1992.[1] The normative values from this group were expressed as the mean, standard deviation, and percentile rank for the total score for each month of age, and time norms for the achievement of each item.[7] These reference figures and norms with percentile ranks are accessible in the AIMS Manual.[7]
The interrater and test-retest reliability of the original scale and was found to be 0.99.[7] The concurrent validity of the original scale was assessed against the Bayley Scales of Infant and Toddler Development (BSID) and the Peabody Development Motor Scales (PDSM). Concurrent validity with the BSID was 0.98, and 0.97 with the PDSM.[7]
Re-evaluation of the scale was performed in 2014.[7] Developmental norms were assessed in 650 infants from Alberta over a two year period.[8] Darrah et al.[8] reported a correlation coefficient of 0.99 between the original and re-evaluation groups, and concluded that the validity of the initial research was unchanged.[8]
Normative development of infants in other countries have been assessed using the AIMS. Results from these studies have formed population-specific normative values for several of these countries, such as Netherlands,[9] Brazil,[10][11] Serbia,[12] Korea,[13] Greece,[14] Poland,[15] Spain,[16] Thailand,[17] and Taiwan.[18]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 Piper MC, Pinnell LE, Darrah J, Maguire T, Byrne PJ. Construction and validation of the Alberta Infant Motor Scale (AIMS). Can J Public Health. 1992; 83: 46-50.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 Piper MC, Darrah J, editors. Motor assessment of the developing infant. 2nd edition. St. Louis, Missouri: Elsevier, Inc., 2022.
- ↑ 3.0 3.1 Darrah J, Piper M, Watt MJ. Assessment of gross motor skills of at‐risk infants: predictive validity of the Alberta Infant Motor Scale. Developmental medicine & child neurology. 1998 Jul;40(7):485-91.
- ↑ 4.0 4.1 Albuquerque PL, Lemos A, Guerra MQ, Eickmann SH. Accuracy of the Alberta Infant Motor Scale (AIMS) to detect developmental delay of gross motor skills in preterm infants: a systematic review. Developmental neurorehabilitation. 2015 Jan 2;18(1):15-21.
- ↑ Flickr. Thomas Life Crawling. Available from: https://www.flickr.com/photos/thomaslife/2839828469 (accessed 20 July 2022).
- ↑ Flickr. Thomas Life Cutie Pie. Available from: https://www.flickr.com/photos/thomaslife/2635755242/(accessed 20 July 2022
- ↑ 7.0 7.1 7.2 7.3 7.4 Eliks M, Gajewska E. The Alberta Infant Motor Scale: A tool for the assessment of motor aspects of neurodevelopment in infancy and early childhood. Frontiers in Neurology. 2022;13.
- ↑ 8.0 8.1 8.2 Darrah J, Bartlett D, Maguire TO, Avison WR, Lacaze‐Masmonteil T. Have infant gross motor abilities changed in 20 years? A re‐evaluation of the Alberta Infant Motor Scale normative values. Developmental Medicine & Child Neurology. 2014 Sep;56(9):877-81.
- ↑ van Iersel PA, la Bastide-van Gemert S, Wu YC, Hadders-Algra M. Alberta Infant Motor Scale: Cross-cultural analysis of gross motor development in Dutch and Canadian infants and introduction of Dutch norms. Early Human Development. 2020 Dec 1;151:105239.
- ↑ Gontijo AP, de Melo Mambrini JV, Mancini MC. Cross-country validity of the Alberta Infant Motor Scale using a Brazilian sample. Brazilian Journal of Physical Therapy. 2021 Jul 1;25(4):444-9.
- ↑ Valentini NC, Saccani R. Brazilian validation of the alberta infant motor scale. Physical therapy. 2012 Mar 1;92(3):440-7.
- ↑ Lackovic M, Nikolic D, Filimonovic D, Petronic I, Mihajlovic S, Golubovic Z, Pavicevic P, Cirovic D. Reliability, consistency and temporal stability of Alberta Infant Motor Scale in Serbian infants. Children. 2020 Mar 2;7(3):16.
- ↑ Ko J, Lim HK. Reliability Study of the Items of the Alberta Infant Motor Scale (AIMS) Using Kappa Analysis. International Journal of Environmental Research and Public Health. 2022 Feb 4;19(3):1767.
- ↑ Syrengelas D, Kalampoki V, Kleisiouni P, Manta V, Mellos S, Pons R, Chrousos GP, Siahanidou T. Alberta Infant Motor Scale (AIMS) performance of greek preterm infants: comparisons with full-term infants of the same nationality and impact of prematurity-related morbidity factors. Physical therapy. 2016 Jul 1;96(7):1102-8.
- ↑ Eliks M, Sowińska A, Gajewska E. The Polish version of the Alberta Infant Motor Scale: cultural adaptation and validation. Frontiers in Neurology.:1504.
- ↑ Morales-Monforte E, Bagur-Calafat C, Suc-Lerin N, Fornaguera-Martí M, Cazorla-Sánchez E, Girabent-Farrés M. The Spanish version of the Alberta infant motor scale: validity and reliability analysis. Developmental Neurorehabilitation. 2017 Feb 17;20(2):76-82.
- ↑ Aimsamrarn P, Janyachareon T, Rattanathanthong K, Emasithi A, Siritaratiwat W. Cultural translation and adaptation of the Alberta Infant Motor Scale Thai version. Early Human Development. 2019 Mar 1;130:65-70.
- ↑ Jeng SF, Yau KI, Chen LC, Hsiao SF. Alberta infant motor scale: reliability and validity when used on preterm infants in Taiwan. Physical therapy. 2000 Feb 1;80(2):168-78.
- ↑ Warren McAdams, PT, DPT. Alberta Infant motor Scale (AIMS). Available from: https://youtu.be/5QTnUqdZSbA[last accessed 22/07/22]






