Motor Learning Principles to Alter Gait Deviations: Difference between revisions
No edit summary |
(added three updated references) |
||
| (38 intermediate revisions by 3 users not shown) | |||
| Line 3: | Line 3: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
The development of gait deviations can be a normal part of the aging process. | The development of gait deviations can be a normal part of the aging process. Research has shown that approximately 85% of persons aged 60 years ambulate with "normal gait". However, that number decreases to 20% by age 85.<ref name=":0">Ataullah AHM, De Jesus O. Gait Disturbances. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan Available:https://www.ncbi.nlm.nih.gov/books/NBK560610/#article-22020.r6 (accessed 12/07/2022)</ref> A 2018 systematic review by Herssens et al.<ref name=":3" /> looked at development of gait deviations across the lifespan. They found as people age, they tend to develop a "cautious gait pattern" which is characterised by (1) decreased walking speed, (2) decreased cadence, (3) decreased step or stride length, and (4) increased step time.<ref name=":3">Herssens N, Verbecque E, Hallemans A, Vereeck L, Van Rompaey V, Saeys W. [https://repository.uantwerpen.be/docman/irua/5a1b16/152210_2019_06_13.pdf Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review]. Gait & posture. 2018 Jul 1;64:181-90.</ref> Gait deviations can also have a developmental, musculoskeletal, or neurological aetiology.<ref name=":0" /> <blockquote>'''From a rehabilitation perspective, reasons to alter an individual's gait deviation include:'''<ref name=":1" /> | ||
# To improve pain | # To improve pain | ||
| Line 13: | Line 13: | ||
# To prevent injury | # To prevent injury | ||
# To improve safety | # To improve safety | ||
# To decrease need for assistive devices | # To decrease the need for assistive devices | ||
</blockquote> | </blockquote> | ||
== Motor Learning == | == Motor Learning == | ||
Motor learning differs from symptom modification. | Motor learning differs from symptom modification. A '''symptom modification procedure''' can quickly but temporarily alter an individual's performance, often within a single treatment session.<ref name=":1">Howell, D. Gait Analysis. Motor Learning Principles to Alter Gait Deviations. Plus. 2022.</ref> | ||
'''Motor learning''' can be defined as: "a change in the capability of a person to perform a skill that must be inferred from a relatively permanent improvement in performance as a result of practice or experience."<ref>Angin S, Simsek I, editors. Comparative kinesiology of the human body: normal and pathological conditions. Academic Press; 2020 Mar 17. p453-466.</ref> Performance tends to improve as an individual practices a new skill. While these improvements can occur quickly they also tend to be temporary in nature. | '''Motor learning''' can be defined as: "a change in the capability of a person to perform a skill that must be inferred from a relatively permanent improvement in performance as a result of practice or experience."<ref>Angin S, Simsek I, editors. Comparative kinesiology of the human body: normal and pathological conditions. Academic Press; 2020 Mar 17. p453-466.</ref> Performance tends to improve as an individual practices a new skill. While these improvements can occur quickly they also tend to be temporary in nature. True learning occurs when practice continues repeatedly. This allows the new skill to be sustained over time. To learn more about motor learning and motor learning theories, please read [[Motor Learning - Back to the Basics|this article]]. | ||
The most effective way to progress from performance to learned behaviour is to use scientific principles and theories of motor learning. | The most effective way to progress from performance to learned behaviour is to use scientific principles and theories of motor learning. However, translating theory to clinical practice provides an opportunity for creativity on the part of the rehabilitation professional. The use of language, cues, feedback, and or prompts are particularly powerful tools.<ref name=":1" /> | ||
The following optional video provides a summary and comparison of performance and learning. This video is geared towards a sports medicine audience. | |||
{{#ev:youtube| D0jbODh3kQc |500}}<ref>YouTube. Difference between learning and performance. Sport Science Collective. Available from: https://www.youtube.com/watch?v=D0jbODh3kQc [last accessed 17/07/2022]</ref> | |||
== Putting Theory into Practice == | == Putting Theory into Practice == | ||
When adapting motor learning theory into clinical practice, it can be helpful to use a framework to shape how learning will occur. Like any rehabilitation plan | When adapting motor learning theory into clinical practice, it can be helpful to use a framework to shape how learning will occur. Like any rehabilitation care plan, this framework will be individualised to best meet the needs of the patient, i.e. the learner. The rehabilitation professional, i.e. the teacher, can gain insight into the learner's needs during the patient interview and evaluation, and continuously reassess for needed changes or adjustments as therapy progresses. <blockquote>'''Considerations for both teacher and learner:'''<ref name=":1" /> | ||
# Focus of | # Focus of attention: internal versus external | ||
# Sensory | # Sensory preference | ||
# | # Analogy | ||
# | # Explicit versus implicit learning | ||
# Exploratory learning | # Exploratory learning | ||
# | # Segmental sequencing: part versus whole | ||
# Mindset attitude | # Mindset attitude | ||
# Autonomy | # Autonomy | ||
# | # Providing cues, prompts, and feedback | ||
</blockquote> | </blockquote> | ||
=== Focus of | === Focus of attention: internal versus external === | ||
<blockquote>'''Two types of focus of attention:''' | <blockquote>'''Two types of focus of attention:'''<ref>Werner I, Federolf P. Focus of Attention in Coach [https://www.mdpi.com/2411-5142/8/1/7/pdf Instructions for Technique Training in Sports: A Scrutinized Review of Review Studies]. Journal of Functional Morphology and Kinesiology. 2023 Jan 8;8(1):7.</ref> | ||
# '''External focus of attention''' is directed towards the effect of the movement on the environment. | # '''External focus of attention''' is directed towards the effect of the movement on the environment. | ||
# '''Internal focus of attention''' is directed towards components of the body's movement | # '''Internal focus of attention''' is directed towards components of the body's movement. | ||
</blockquote> | </blockquote> | ||
The following optional video provides a summary and comparison of internal and external focus of attention. This video is geared towards a sports medicine audience. | |||
{{#ev:youtube| S3sAvtIJHsM |500}}<ref>YouTube. How Does Attention Affect Motor Skill Learning and Performance? Sport Science Collective. Available from: https://www.youtube.com/watch?v=S3sAvtIJHsM [last accessed 17/07/2022]</ref> | |||
A 15-year review of literature found that research on focus of attention has consistently shown that an external focus enhances motor performance and learning when compared to internal focus.<ref>Wulf G. [http://gwulf.faculty.unlv.edu/wp-content/uploads/2018/11/Wulf_AF_review_2013.pdf Attentional focus and motor learning: a review of 15 years]. International Review of sport and Exercise psychology. 2013 Sep 1;6(1):77-104.</ref> However, there are some conflicting and contradictory opinions regarding this opinion. Historically, physiotherapists have underutilised the concept of external focus of attention during cueing, prompting, and feedback.<ref name=":1" /> | |||
Kal and colleagues<ref name=":4" /> published a series of studies observing interactions between physiotherapists and patients with stroke. Specifically they assessed how the physiotherapists worded their feedback and cues during therapy interventions. They found that only 33% of the therapists were using an external focus of attention, and often after a cue with external focus, the feedback would frequently shift back to an internal focus.<ref name=":4">Kal E, van den Brink H, Houdijk H, van der Kamp J, Goossens PH, van Bennekom C, Scherder E. [https://bura.brunel.ac.uk/bitstream/2438/20074/2/FullText.pdf How physical therapists instruct patients with stroke: an observational study on attentional focus during gait rehabilitation after stroke]. Disability and rehabilitation. 2018 May 8;40(10):1154-65.</ref> For rehabilitation practice, an individualised use of attentional focus instructions may be more effective than an exclusive reliance on external focus instructions, especially if a patient's motor, sensory, and attentional functioning may be impaired.<ref>Kal E, Houdijk H, van der Kamp J, Verhoef M, Prosée R, Groet E, Winters M, van Bennekom C, Scherder E. [https://vbn.aau.dk/ws/files/334793016/FullText.pdf Are the effects of internal focus instructions different from external focus instructions given during balance training in stroke patients? A double-blind randomized controlled trial.] Clinical rehabilitation. 2019 Feb;33(2):207-21.</ref> When used appropriately, both external and internal focus of attention can improve performance and learning.<ref name=":1" /> | |||
Piccoli et al.<ref name=":5" /> looked at focus on attention in patients with neurological central nervous system (CNS) deficits as compared to those with musculoskeletal disorders. When comparing patients with stroke or idiopathic Parkinson's disease (PD) to healthy subjects, there was conflicting evidence over which focus of attention strategy produced better clinical outcomes. External focus of attention did not always improve motor learning compared to internal focus of attention due to the pathological motor impairments of stroke and PD. Changes in sensory pathways, including vision and proprioception, were also found to affect attentional strategy use. This study found that external focus of attention is more effective than internal focus of attention in affecting motor learning in patients with musculoskeletal disorders.<ref name=":5">Piccoli A, Rossettini G, Cecchetto S, Viceconti A, Ristori D, Turolla A, Maselli F, Testa M. [https://www.mdpi.com/2411-5142/3/3/40/pdf Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: A systematic review]. Journal of Functional Morphology and Kinesiology. 2018 Jul 25;3(3):40.</ref> | |||
There is research to suggest that novice learners are likely to do better with an internal focus of attention, whereas experts do better with external focus of attention. There is also evidence that younger learners likely do better with an external focus, whereas older learners can do well with external and or internal.<ref name=":1" /> | |||
Gose et al.<ref name=":6" /> have suggested that the dichotomy between external focus of attention and internal focus of attention functions as a spectrum. They suggest that seeing focus of attention as a binary paradigm overlooks the dynamic and constantly changing interactions between the individual, the task, and the environment.<ref name=":6">Gose R, Abraham A. Looking beyond the binary: an extended paradigm for focus of attention in human motor performance. Experimental Brain Research. 2021 Jun;239(6):1687-99.</ref> Whether the chosen focus of attention is internal or external, clinicians should use words that are consistent with the patient's preferred sensory learning system.<ref name=":1" /> | |||
=== Sensory Preference === | === Sensory Preference === | ||
<blockquote>'''Three sensory systems involved in mobility:'''<ref name=":1" /> | |||
# Visual | # Visual | ||
# Auditory | # Auditory | ||
# | # Kinaesthetic | ||
</blockquote> | </blockquote> | ||
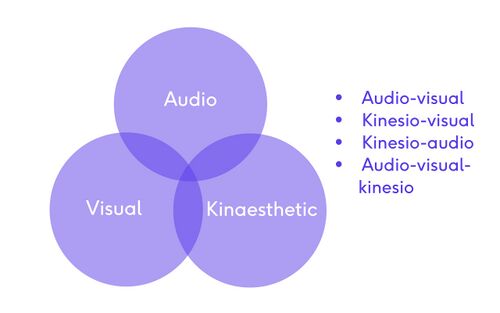
[[File:Sensory learning.jpg|thumb|500x500px|Potential overlap of the preferred sensory system allows for creativity during therapeutic interventions.]] | |||
Ciraolo et al.<ref name=":7" /> found that the majority of people have a preferred sensory system. The visual system was the most commonly preferred sensory system.<ref name=":7">Ciraolo MF, O’Hanlon SM, Robinson CW, Sinnett S. [https://www.mdpi.com/2411-5150/4/1/14/pdf Stimulus onset modulates auditory and visual dominance]. Vision. 2020 Feb 29;4(1):14.</ref> If a patient's preferred sensory system can be identified, the rehabilitation professional can fine tune their cueing, prompting, and feedback style.<ref>Chouhan N, Shan R, Gupta M, Rashid S, Manhas M. [https://scholar.google.com/scholar?output=instlink&q=info:3UoHwNnpkngJ:scholar.google.com/&hl=en&as_sdt=0,44&as_ylo=2022&scillfp=11440700864907149161&oi=lle Evaluation of preferred learning styles among undergraduate students of government medical college, Jammu]. Natl J Physiol Pharm Pharmacol. 2023;13.</ref> | |||
In the clinical setting, a simple way to determine a person's preferred sensory system can be to ask: "What three adjectives would you use to describe a day at the beach?"<ref name=":1" /> | |||
* If they describe: "It's warm, the sand is between my toes, I feel the breeze on my ear," they tend to be a kinaesthetic learner. | |||
* If they describe: "I hear the waves crashing, the kids are squealing on the beach, and the seagulls are calling out," they tend to be an auditory learner. | |||
* If they describe: "The sky is blue, the sand is brown, I see the waves rolling in," they tend to be a visual learner. | |||
* Some patients may give descriptors for multiple sensory systems | |||
** For example: a patient can have a kinesio-visual, kinesio-audio, or audio-visual-kinesio sensory preference. | |||
=== Analogy === | |||
* Analogy identifies a target image which connects new information to old information | |||
* The best image will connect to something that is familiar to the learner | |||
* Language used should be consistent with the client's preferred sensory system | |||
* It is preferable to have the image external to the body | |||
* The analogy wording should be short in length, this allows it to be used like a mantra during gait training<ref name=":1" /> | |||
'''Examples of how analogy can be used in gait training:'''<ref name=":1" /> | |||
{| class="wikitable" | |||
|+ | |||
!'''Desired gait outcome''' | |||
!'''Analogy''' | |||
|- | |||
|To keep daylight between the knees | |||
|"Walk as if you are wearing a full diaper" | |||
|- | |||
|A stable pelvis | |||
|"Imagine your pelvis is a bucket full of water, don't let it spill out the side" | |||
|- | |||
|Forward kneecap/leg alignment | |||
|"Keep the kneecap pointing down that road like a headlight. Don't let the headlight veer off to either side" | |||
|- | |||
|Proper step or stride length | |||
|"Image you are walking along a railroad line, stepping on each railroad tie" | |||
|- | |||
|Increased hip and or knee flexion | |||
|"Walk as if you are walking in deep snow" | |||
|} | |||
=== Explicit versus implicit learning === | |||
* Explicit learning is at a conscious level whereas implicit is unconscious | |||
* Implicit learning tends to be more durable | |||
* "Some experts argue that if you have an analogy, it's thought to be more implicit, more automatic, you can kind of keep it in the back of your mind."<ref name=":1" /> | |||
The dichotomy of implicit learning versus explicit learning can be a spectrum of learning. Both can occur simultaneously, but with increased practice and reinforcement of the new gait pattern, more implicit learning will occur.<ref name=":1" /><ref>Dawidowicz G, Shaine Y, Mawase F. [https://www.biorxiv.org/content/biorxiv/early/2021/05/27/2021.05.27.445962.full.pdf Separation of multiple motor memories through implicit and explicit processes]. Journal of Neurophysiology. 2022 Feb 1;127(2):329-40.</ref> | |||
'''Examples of implicit learning in physiotherapy:'''<ref name=":1" /> | |||
* Barefoot running | |||
* Backwards walking | |||
* Split treadmill walking | |||
* Constraint therapy | |||
* Robotic gait training | |||
* Metronome or music with a strong beat for altering cadence | |||
The following optional video offers a short discussion of explicit and implicit learning. This video is geared towards a sports medicine audience. | |||
{{#ev:youtube| Dl1QPTdTxkw |500}}<ref>YouTube. Coaching Science. Explicit Vs Implicit Learning. Sport Science Collective. Available from: https://www.youtube.com/watch?v=Dl1QPTdTxkw [last accessed 17/07/2022]</ref> | |||
=== Exploratory learning === | === Exploratory learning === | ||
<blockquote>'''Exploratory learning involves the following:'''<ref>Edutech Wiki. Exploratory learning. Available from: https://edutechwiki.unige.ch/en/Exploratory_learning (accessed 16/07/22).</ref> | |||
* Learners can and should take control of their own learning | |||
* Knowledge is rich and multidimensional | |||
* Learners approach the learning task in very diverse ways | |||
* Learning should feel natural and un-coaxed | |||
</blockquote> | |||
This optional video provides a concise discussion on exploratory learning or "learning by doing." | |||
{{#ev:youtube| CJN9QKukfPc |500}}<ref>YouTube. Experiential Learning Explained - Definition & Theory. Adventure Associates. Available from: https://www.youtube.com/watch?v=CJN9QKukfPc [last accessed 17/07/2022]</ref> | |||
=== | === Segmental sequencing: part versus whole === | ||
Different gait deviations need different types of sequencing practice:<ref name=":1" /> | |||
* The '''whole method''' involves completing the entire task together at one time | |||
** Spatial temporal deviations tend to respond better to the whole method | |||
* The '''part method''' involves the movement being completed whole, then broken down into parts, then practised as whole again | |||
** When deviations are less related to spatial temporal components, individuals tend to do better with breaking the task down into parts | |||
** When disparate body regions are involved, individuals tend to do well by breaking the task into parts | |||
** When breaking a task down into parts, use the patient's preferred sensory system to facilitate learning | |||
=== Mindset attitude === | === Mindset attitude === | ||
There is growing evidence that using positive language and encouraging a positive mindset gives better results; positive language is better than negative language. While both ways of communicating can give good results, using a positive mindset and minimising nocebic words tends to be more efficient and have longer lasting results.<ref name=":1" /> | |||
{| class="wikitable" | |||
|+ | |||
!'''Placebo – Positive - Affirmation''' | |||
!'''Nocebo – Negative''' | |||
|- | |||
|See that, do that | |||
|See that, don’t do that | |||
|- | |||
|Hear that, do that | |||
|Hear that, don't do that | |||
|- | |||
|Feel that, do that | |||
|Feel that, don't do that | |||
|- | |||
|New way | |||
|Old way | |||
|- | |||
|Less or no pain | |||
|With pain | |||
|} | |||
Wulf et al.<ref name=":2" /> proposed the OPTIMAL (Optimizing Performance through Intrinsic Motivation and Attention for Learning) theory of motor learning. This theory involves:<ref name=":2">Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: [https://link.springer.com/article/10.3758/s13423-015-0999-9 The OPTIMAL theory of motor learning. Psychonomic bulletin & review]. 2016 Oct;23(5):1382-414.</ref> | |||
# Conditions that enhance expectancies for future performance | |||
# Variables that influence learners' autonomy | |||
# External focus of attention on the intended movement task | |||
This theory suggests that motivational and attentional factors contribute to improved performance and learning by encouraging the combination of goals and actions. The use of a positive mindset is associated with dopamine release which is temporally associated with skill practice. Expected success can enhance the learner's expectations that they will have positive results in a similar task in the future. This helps to consolidate memories and learning retention.<ref name=":2" /> Setting appropriately challenging but attainable goals and subgoals can further encourage and motivate a patient.<ref name=":1" /> | |||
=== Autonomy === | === Autonomy === | ||
Providing the patient with a choice, i.e. some control of conditions, can enhance their learning and motivation. This can include choice in: (1) instructional language, (2) sensory preference, and (3) practice conditions. Therapeutic interventions need to be designed for the individual characteristics and adjusted based on the individual's response. One size does not fit all.<ref name=":1" /> | |||
=== Providing cues, prompts, and feedback<ref name=":1" /> === | |||
* Begin with an external focus of attention | |||
* Include an image or an analogy | |||
* Use positive placebo language | |||
* Use the individual's preferred learning sensory system | |||
* Enhance autonomy | |||
* Make cues, prompts and feedback short | |||
* Use contrast | |||
* Facilitate exploration | |||
* Provide opportunity to use implicit instinctual learning | |||
== Resources == | == Resources == | ||
'''Optional Recommended Reading:''' | |||
*Piccoli A, Rossettini G, Cecchetto S, Viceconti A, Ristori D, Turolla A, Maselli F, Testa M. [https://www.mdpi.com/2411-5142/3/3/40/pdf Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: A systematic review]. Journal of Functional Morphology and Kinesiology. 2018 Jul 25;3(3):40. | *Piccoli A, Rossettini G, Cecchetto S, Viceconti A, Ristori D, Turolla A, Maselli F, Testa M. [https://www.mdpi.com/2411-5142/3/3/40/pdf Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: A systematic review]. Journal of Functional Morphology and Kinesiology. 2018 Jul 25;3(3):40. | ||
*Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: [https://link.springer.com/article/10.3758/s13423-015-0999-9 The OPTIMAL theory of motor learning. Psychonomic bulletin & review]. 2016 Oct;23(5):1382-414. | |||
'''Clinical Resources:''' | |||
* {{pdf|Motor_Learning_Example.pdf|Instructive Motor Learning Example of Contralateral Pelvic Drop}} | |||
* {{pdf|Template_motor_learning.pdf|Blank Instructive Motor Learning Template}} | |||
'''Optional Video:''' | |||
Please enjoy this podcast interview of Gaby Wulf and Rebecca Lewthwaite as they discuss their OPTIMAL Theory of Motor Learning. This interview covers many of the topics overviewed in this article and gives great insight into the OPTIMAL Theory. | |||
{{#ev:youtube| _BGNVfQDkdc |500}}<ref>YouTube. Interview with Gaby Wulf & Rebecca Lewthwaite, OPTIMAL Theory of Motor Learning. Available from: https://www.youtube.com/watch?v=_BGNVfQDkdc [last accessed 17/07/2022]</ref> | |||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
[[Category:Gait]] | |||
Latest revision as of 06:15, 28 January 2023
Top Contributors - Stacy Schiurring, Kim Jackson and Jess Bell
Introduction[edit | edit source]
The development of gait deviations can be a normal part of the aging process. Research has shown that approximately 85% of persons aged 60 years ambulate with "normal gait". However, that number decreases to 20% by age 85.[1] A 2018 systematic review by Herssens et al.[2] looked at development of gait deviations across the lifespan. They found as people age, they tend to develop a "cautious gait pattern" which is characterised by (1) decreased walking speed, (2) decreased cadence, (3) decreased step or stride length, and (4) increased step time.[2] Gait deviations can also have a developmental, musculoskeletal, or neurological aetiology.[1]
From a rehabilitation perspective, reasons to alter an individual's gait deviation include:[3]
- To improve pain
- To improve endurance
- To improve efficiency
- To improve performance
- To improve quality of movements
- To prevent injury
- To improve safety
- To decrease the need for assistive devices
Motor Learning[edit | edit source]
Motor learning differs from symptom modification. A symptom modification procedure can quickly but temporarily alter an individual's performance, often within a single treatment session.[3]
Motor learning can be defined as: "a change in the capability of a person to perform a skill that must be inferred from a relatively permanent improvement in performance as a result of practice or experience."[4] Performance tends to improve as an individual practices a new skill. While these improvements can occur quickly they also tend to be temporary in nature. True learning occurs when practice continues repeatedly. This allows the new skill to be sustained over time. To learn more about motor learning and motor learning theories, please read this article.
The most effective way to progress from performance to learned behaviour is to use scientific principles and theories of motor learning. However, translating theory to clinical practice provides an opportunity for creativity on the part of the rehabilitation professional. The use of language, cues, feedback, and or prompts are particularly powerful tools.[3]
The following optional video provides a summary and comparison of performance and learning. This video is geared towards a sports medicine audience.
Putting Theory into Practice[edit | edit source]
When adapting motor learning theory into clinical practice, it can be helpful to use a framework to shape how learning will occur. Like any rehabilitation care plan, this framework will be individualised to best meet the needs of the patient, i.e. the learner. The rehabilitation professional, i.e. the teacher, can gain insight into the learner's needs during the patient interview and evaluation, and continuously reassess for needed changes or adjustments as therapy progresses.
Considerations for both teacher and learner:[3]
- Focus of attention: internal versus external
- Sensory preference
- Analogy
- Explicit versus implicit learning
- Exploratory learning
- Segmental sequencing: part versus whole
- Mindset attitude
- Autonomy
- Providing cues, prompts, and feedback
Focus of attention: internal versus external[edit | edit source]
Two types of focus of attention:[6]
- External focus of attention is directed towards the effect of the movement on the environment.
- Internal focus of attention is directed towards components of the body's movement.
The following optional video provides a summary and comparison of internal and external focus of attention. This video is geared towards a sports medicine audience.
A 15-year review of literature found that research on focus of attention has consistently shown that an external focus enhances motor performance and learning when compared to internal focus.[8] However, there are some conflicting and contradictory opinions regarding this opinion. Historically, physiotherapists have underutilised the concept of external focus of attention during cueing, prompting, and feedback.[3]
Kal and colleagues[9] published a series of studies observing interactions between physiotherapists and patients with stroke. Specifically they assessed how the physiotherapists worded their feedback and cues during therapy interventions. They found that only 33% of the therapists were using an external focus of attention, and often after a cue with external focus, the feedback would frequently shift back to an internal focus.[9] For rehabilitation practice, an individualised use of attentional focus instructions may be more effective than an exclusive reliance on external focus instructions, especially if a patient's motor, sensory, and attentional functioning may be impaired.[10] When used appropriately, both external and internal focus of attention can improve performance and learning.[3]
Piccoli et al.[11] looked at focus on attention in patients with neurological central nervous system (CNS) deficits as compared to those with musculoskeletal disorders. When comparing patients with stroke or idiopathic Parkinson's disease (PD) to healthy subjects, there was conflicting evidence over which focus of attention strategy produced better clinical outcomes. External focus of attention did not always improve motor learning compared to internal focus of attention due to the pathological motor impairments of stroke and PD. Changes in sensory pathways, including vision and proprioception, were also found to affect attentional strategy use. This study found that external focus of attention is more effective than internal focus of attention in affecting motor learning in patients with musculoskeletal disorders.[11]
There is research to suggest that novice learners are likely to do better with an internal focus of attention, whereas experts do better with external focus of attention. There is also evidence that younger learners likely do better with an external focus, whereas older learners can do well with external and or internal.[3]
Gose et al.[12] have suggested that the dichotomy between external focus of attention and internal focus of attention functions as a spectrum. They suggest that seeing focus of attention as a binary paradigm overlooks the dynamic and constantly changing interactions between the individual, the task, and the environment.[12] Whether the chosen focus of attention is internal or external, clinicians should use words that are consistent with the patient's preferred sensory learning system.[3]
Sensory Preference[edit | edit source]
Three sensory systems involved in mobility:[3]
- Visual
- Auditory
- Kinaesthetic
Ciraolo et al.[13] found that the majority of people have a preferred sensory system. The visual system was the most commonly preferred sensory system.[13] If a patient's preferred sensory system can be identified, the rehabilitation professional can fine tune their cueing, prompting, and feedback style.[14]
In the clinical setting, a simple way to determine a person's preferred sensory system can be to ask: "What three adjectives would you use to describe a day at the beach?"[3]
- If they describe: "It's warm, the sand is between my toes, I feel the breeze on my ear," they tend to be a kinaesthetic learner.
- If they describe: "I hear the waves crashing, the kids are squealing on the beach, and the seagulls are calling out," they tend to be an auditory learner.
- If they describe: "The sky is blue, the sand is brown, I see the waves rolling in," they tend to be a visual learner.
- Some patients may give descriptors for multiple sensory systems
- For example: a patient can have a kinesio-visual, kinesio-audio, or audio-visual-kinesio sensory preference.
Analogy[edit | edit source]
- Analogy identifies a target image which connects new information to old information
- The best image will connect to something that is familiar to the learner
- Language used should be consistent with the client's preferred sensory system
- It is preferable to have the image external to the body
- The analogy wording should be short in length, this allows it to be used like a mantra during gait training[3]
Examples of how analogy can be used in gait training:[3]
| Desired gait outcome | Analogy |
|---|---|
| To keep daylight between the knees | "Walk as if you are wearing a full diaper" |
| A stable pelvis | "Imagine your pelvis is a bucket full of water, don't let it spill out the side" |
| Forward kneecap/leg alignment | "Keep the kneecap pointing down that road like a headlight. Don't let the headlight veer off to either side" |
| Proper step or stride length | "Image you are walking along a railroad line, stepping on each railroad tie" |
| Increased hip and or knee flexion | "Walk as if you are walking in deep snow" |
Explicit versus implicit learning[edit | edit source]
- Explicit learning is at a conscious level whereas implicit is unconscious
- Implicit learning tends to be more durable
- "Some experts argue that if you have an analogy, it's thought to be more implicit, more automatic, you can kind of keep it in the back of your mind."[3]
The dichotomy of implicit learning versus explicit learning can be a spectrum of learning. Both can occur simultaneously, but with increased practice and reinforcement of the new gait pattern, more implicit learning will occur.[3][15]
Examples of implicit learning in physiotherapy:[3]
- Barefoot running
- Backwards walking
- Split treadmill walking
- Constraint therapy
- Robotic gait training
- Metronome or music with a strong beat for altering cadence
The following optional video offers a short discussion of explicit and implicit learning. This video is geared towards a sports medicine audience.
Exploratory learning[edit | edit source]
Exploratory learning involves the following:[17]
- Learners can and should take control of their own learning
- Knowledge is rich and multidimensional
- Learners approach the learning task in very diverse ways
- Learning should feel natural and un-coaxed
This optional video provides a concise discussion on exploratory learning or "learning by doing."
Segmental sequencing: part versus whole[edit | edit source]
Different gait deviations need different types of sequencing practice:[3]
- The whole method involves completing the entire task together at one time
- Spatial temporal deviations tend to respond better to the whole method
- The part method involves the movement being completed whole, then broken down into parts, then practised as whole again
- When deviations are less related to spatial temporal components, individuals tend to do better with breaking the task down into parts
- When disparate body regions are involved, individuals tend to do well by breaking the task into parts
- When breaking a task down into parts, use the patient's preferred sensory system to facilitate learning
Mindset attitude[edit | edit source]
There is growing evidence that using positive language and encouraging a positive mindset gives better results; positive language is better than negative language. While both ways of communicating can give good results, using a positive mindset and minimising nocebic words tends to be more efficient and have longer lasting results.[3]
| Placebo – Positive - Affirmation | Nocebo – Negative |
|---|---|
| See that, do that | See that, don’t do that |
| Hear that, do that | Hear that, don't do that |
| Feel that, do that | Feel that, don't do that |
| New way | Old way |
| Less or no pain | With pain |
Wulf et al.[19] proposed the OPTIMAL (Optimizing Performance through Intrinsic Motivation and Attention for Learning) theory of motor learning. This theory involves:[19]
- Conditions that enhance expectancies for future performance
- Variables that influence learners' autonomy
- External focus of attention on the intended movement task
This theory suggests that motivational and attentional factors contribute to improved performance and learning by encouraging the combination of goals and actions. The use of a positive mindset is associated with dopamine release which is temporally associated with skill practice. Expected success can enhance the learner's expectations that they will have positive results in a similar task in the future. This helps to consolidate memories and learning retention.[19] Setting appropriately challenging but attainable goals and subgoals can further encourage and motivate a patient.[3]
Autonomy[edit | edit source]
Providing the patient with a choice, i.e. some control of conditions, can enhance their learning and motivation. This can include choice in: (1) instructional language, (2) sensory preference, and (3) practice conditions. Therapeutic interventions need to be designed for the individual characteristics and adjusted based on the individual's response. One size does not fit all.[3]
Providing cues, prompts, and feedback[3][edit | edit source]
- Begin with an external focus of attention
- Include an image or an analogy
- Use positive placebo language
- Use the individual's preferred learning sensory system
- Enhance autonomy
- Make cues, prompts and feedback short
- Use contrast
- Facilitate exploration
- Provide opportunity to use implicit instinctual learning
Resources[edit | edit source]
Optional Recommended Reading:
- Piccoli A, Rossettini G, Cecchetto S, Viceconti A, Ristori D, Turolla A, Maselli F, Testa M. Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: A systematic review. Journal of Functional Morphology and Kinesiology. 2018 Jul 25;3(3):40.
- Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychonomic bulletin & review. 2016 Oct;23(5):1382-414.
Clinical Resources:
- Instructive Motor Learning Example of Contralateral Pelvic Drop
- Blank Instructive Motor Learning Template
Optional Video:
Please enjoy this podcast interview of Gaby Wulf and Rebecca Lewthwaite as they discuss their OPTIMAL Theory of Motor Learning. This interview covers many of the topics overviewed in this article and gives great insight into the OPTIMAL Theory.
References[edit | edit source]
- ↑ 1.0 1.1 Ataullah AHM, De Jesus O. Gait Disturbances. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan Available:https://www.ncbi.nlm.nih.gov/books/NBK560610/#article-22020.r6 (accessed 12/07/2022)
- ↑ 2.0 2.1 Herssens N, Verbecque E, Hallemans A, Vereeck L, Van Rompaey V, Saeys W. Do spatiotemporal parameters and gait variability differ across the lifespan of healthy adults? A systematic review. Gait & posture. 2018 Jul 1;64:181-90.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 Howell, D. Gait Analysis. Motor Learning Principles to Alter Gait Deviations. Plus. 2022.
- ↑ Angin S, Simsek I, editors. Comparative kinesiology of the human body: normal and pathological conditions. Academic Press; 2020 Mar 17. p453-466.
- ↑ YouTube. Difference between learning and performance. Sport Science Collective. Available from: https://www.youtube.com/watch?v=D0jbODh3kQc [last accessed 17/07/2022]
- ↑ Werner I, Federolf P. Focus of Attention in Coach Instructions for Technique Training in Sports: A Scrutinized Review of Review Studies. Journal of Functional Morphology and Kinesiology. 2023 Jan 8;8(1):7.
- ↑ YouTube. How Does Attention Affect Motor Skill Learning and Performance? Sport Science Collective. Available from: https://www.youtube.com/watch?v=S3sAvtIJHsM [last accessed 17/07/2022]
- ↑ Wulf G. Attentional focus and motor learning: a review of 15 years. International Review of sport and Exercise psychology. 2013 Sep 1;6(1):77-104.
- ↑ 9.0 9.1 Kal E, van den Brink H, Houdijk H, van der Kamp J, Goossens PH, van Bennekom C, Scherder E. How physical therapists instruct patients with stroke: an observational study on attentional focus during gait rehabilitation after stroke. Disability and rehabilitation. 2018 May 8;40(10):1154-65.
- ↑ Kal E, Houdijk H, van der Kamp J, Verhoef M, Prosée R, Groet E, Winters M, van Bennekom C, Scherder E. Are the effects of internal focus instructions different from external focus instructions given during balance training in stroke patients? A double-blind randomized controlled trial. Clinical rehabilitation. 2019 Feb;33(2):207-21.
- ↑ 11.0 11.1 Piccoli A, Rossettini G, Cecchetto S, Viceconti A, Ristori D, Turolla A, Maselli F, Testa M. Effect of attentional focus instructions on motor learning and performance of patients with central nervous system and musculoskeletal disorders: A systematic review. Journal of Functional Morphology and Kinesiology. 2018 Jul 25;3(3):40.
- ↑ 12.0 12.1 Gose R, Abraham A. Looking beyond the binary: an extended paradigm for focus of attention in human motor performance. Experimental Brain Research. 2021 Jun;239(6):1687-99.
- ↑ 13.0 13.1 Ciraolo MF, O’Hanlon SM, Robinson CW, Sinnett S. Stimulus onset modulates auditory and visual dominance. Vision. 2020 Feb 29;4(1):14.
- ↑ Chouhan N, Shan R, Gupta M, Rashid S, Manhas M. Evaluation of preferred learning styles among undergraduate students of government medical college, Jammu. Natl J Physiol Pharm Pharmacol. 2023;13.
- ↑ Dawidowicz G, Shaine Y, Mawase F. Separation of multiple motor memories through implicit and explicit processes. Journal of Neurophysiology. 2022 Feb 1;127(2):329-40.
- ↑ YouTube. Coaching Science. Explicit Vs Implicit Learning. Sport Science Collective. Available from: https://www.youtube.com/watch?v=Dl1QPTdTxkw [last accessed 17/07/2022]
- ↑ Edutech Wiki. Exploratory learning. Available from: https://edutechwiki.unige.ch/en/Exploratory_learning (accessed 16/07/22).
- ↑ YouTube. Experiential Learning Explained - Definition & Theory. Adventure Associates. Available from: https://www.youtube.com/watch?v=CJN9QKukfPc [last accessed 17/07/2022]
- ↑ 19.0 19.1 19.2 Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: The OPTIMAL theory of motor learning. Psychonomic bulletin & review. 2016 Oct;23(5):1382-414.
- ↑ YouTube. Interview with Gaby Wulf & Rebecca Lewthwaite, OPTIMAL Theory of Motor Learning. Available from: https://www.youtube.com/watch?v=_BGNVfQDkdc [last accessed 17/07/2022]