Characteristics and Identification of Wound Types: Pressure Injuries and Non-healing Surgical Wounds: Difference between revisions
No edit summary |
No edit summary |
||
| Line 29: | Line 29: | ||
<div class="row"> | <div class="row"> | ||
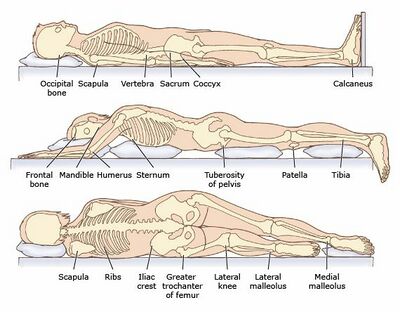
<div class="col-md-6"> [[File:Pressure sore.jpeg|none|thumb|Areas of concern for pressure injuries in bed]]</div> | <div class="col-md-6"> [[File:Pressure sore.jpeg|none|thumb|Areas of concern for pressure injuries in bed|alt=|400x400px]]</div> | ||
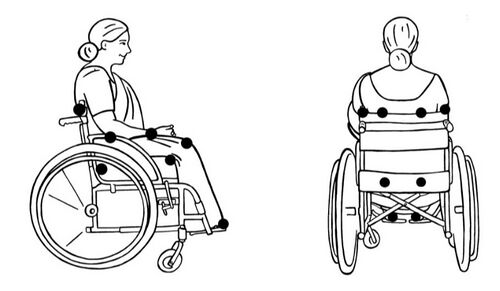
<div class="col-md-6"> [[File:Common Pressure Areas.jpeg|none|thumb|Areas of concern for pressure injuries in sitting]] </div> | <div class="col-md-6"> [[File:Common Pressure Areas.jpeg|none|thumb|Areas of concern for pressure injuries in sitting|alt=|500x500px]] </div> | ||
</div> | </div> | ||
=== Risk factors for pressure injuries === | |||
=== | |||
# Immobility is the primary risk factor. Bodily tissues are only capable of tolerating a certain amount of pressure. That may be a low pressure over a long period of time or a high pressure over a short period of time. Under normal circumstances, our body informs us when it's time to change positions. If there is a lack of mobility or a loss of sensation, a patient may not receive feedback that they need to change position, or they may be unable to change the position for themselves, right? | # Immobility is the primary risk factor. Bodily tissues are only capable of tolerating a certain amount of pressure. That may be a low pressure over a long period of time or a high pressure over a short period of time. Under normal circumstances, our body informs us when it's time to change positions. If there is a lack of mobility or a loss of sensation, a patient may not receive feedback that they need to change position, or they may be unable to change the position for themselves, right? | ||
Revision as of 18:27, 21 September 2022
Top Contributors - Stacy Schiurring, Jess Bell and Kim Jackson
Introduction[edit | edit source]
This article provides information for those rehabilitation professionals who are new to wound care or have been away from the practise and need a review of wound type identification. This article will not go into specifics on wound assessment or treatment.
The five most common types of chronic wounds include (1) arterial ulcers, (2) venous insufficiency ulcers or venous wounds, (3) neuropathic wounds, or diabetic foot ulcers, (4) pressure injuries, formerly known as pressure ulcers, and (5) non-healing surgical wounds.
The terms ulcer and wound will be used interchangeably throughout this article.[1]
Due to the large amount of information to be presented, this topic has been divided into three separate pages. This page will cover pressure injuries and non-healing surgical wounds. To learn more about arterial wounds and venous insufficiency ulcers, please see this article. To learn more about neuropathic wounds, please see this article.
Pressure Injuries[edit | edit source]
Pressure injuries (formally known as pressure ulcers, decubitus ulcers, or bedsores) develop in localised areas when soft tissues are compressed between a bony prominence and an external surface for a prolonged amount of time.[1][2] When the tissue is compressed, blood flow to the area stops or is decreased below a level that is necessary to sustain cell function. This lack of oxygen and nutrients results in cell death.[1] Deep tissue pressure injuries are areas of underlying soft tissue necrosis which present with persistent non-blaunchable deep red or purple areas of intact or non-intact skin, or blood-filled blisters. Deep tissue pressure injuries are a serious form of pressure injury because they start in the underlying tissues and are not visible at the skin's surface until the wound is already quite advanced.[2]
- The term injury is more accurate term than ulcer because this condition does not always present as an open wound, damage can start in the deeper soft tissue layers.
- The term injury also helps focus on wound prevention rather than reactive treatment. Prevention is key to successful management for these wounds.
Time to tissue breakdown[edit | edit source]
The amount of time required for cell death and tissue destruction is variable. It is dependent upon (1) tissue integrity, the (2) amount of pressure, and the (3) duration of pressure. For example, persons who are thin, have multiple comorbidities, and are bed bound may see effects sooner than persons of a different build, health status, and mobility level.
General guidelines for tissue breakdown and recovery: every individual is unique and requires a personalised care plan
- Blanchable erythema occurs after approximately 30 minutes of unrelieved pressure. It requires one hour for tissue recovery once pressure is relieved.
- Tissue ischaemia occurs within two to six hours of unrelieved pressure and is seen as a deeper redness. It requires 36 hours for tissue recovery once pressure is relieved.
- Tissue necrosis occurs after six or more hours of unrelieved pressure. Once necrosis has occurred, recovery may not be possible.
The most common sites of pressure injuries include the (1) sacrum, (2) ischial tuberosities, (3) greater trochanters, and the (4) heels. But keep in mind that pressure injuries can occur on any part of the body where there is unrelieved pressure.
Risk factors for pressure injuries[edit | edit source]
- Immobility is the primary risk factor. Bodily tissues are only capable of tolerating a certain amount of pressure. That may be a low pressure over a long period of time or a high pressure over a short period of time. Under normal circumstances, our body informs us when it's time to change positions. If there is a lack of mobility or a loss of sensation, a patient may not receive feedback that they need to change position, or they may be unable to change the position for themselves, right?
- The next is shear. This occurs when the skin moves in relation to the underlying tissue. You can simulate this by placing your finger on a spot in the back of your hand and moving it back and forth without moving it off of the spot. Shear forces distort both the superficial and deep tissue, and that can result in damage to the capillaries and then reduce the blood flow and oxygen to the tissues. The most common position that increases shear force is the semi-fowler's position. In this position, the skeleton slides down, but the sacral skin stays in place, which stretches the tissues in between. Now, sometimes this is necessary, but we need to mitigate that.
- The next is friction. That occurs when an object moves across the surface of the skin. So you can simulate this by placing your hand in your elbow and rubbing it down towards your wrist. Right? So friction alone does not cause a pressure injury, but it causes an abrasion. This can also wear away the epidermis and that results in a reduced tolerance to the shear forces that occur deeper within the tissue.
- The next is moisture or excess fluid on the skin. So this can be due to exudate, sweating, or incontinence. This causes maceration and reduces the skin's tolerance to shear and friction forces. When moisture is an issue, moisture-wicking briefs can be used when the patient is out of bed. And then just lying on an open chuck pad with no briefs can be used when in bed.
- The next is malnutrition. This can reduce the healing of current wounds, and then also increase the risk of further tissue breakdown. A BMI of less than 18.5 or those that are very thin or cachectic are at higher risk. They have more bony prominences and the tissues are subjected to higher pressures from external sources.
- The next is age. So older patients are at greater risk just due to their decreased healing capacity, reduced skin integrity, increased likelihood of mobility issues, multiple comorbidities, 70% of pressure ulcers occur in those that are over the age of 70.
- Significant or severe systemic disease or multiple comorbidities. So diabetes specifically influences the development of pressure injuries, patients with hip fractures that also have diabetes will develop pressure injuries more often than those with hip fractures who do not have diabetes. So that goes for other comorbidities as well. Those that have current wounds that are due to pressure are at a significantly higher risk for developing more for obvious reasons due to a lack of mobility. Going along those lines, longer stay in the ICU also increases your risk. This is likely due to the severity of the condition, limited mobility, and the sustained positioning that's required for certain procedures. Patients with hypotension. So this is interesting. We always think of hypertension as being a problem, but with these patients, it's actually reduced oxygenation and perfusion of the tissues that may be affecting their ability to heal. So keep that in mind.
The three most common scales that are used to predict pressure injury risk are the
- Braden scale,
- the Waterlow scale and t
- he Norton scale. These scales look at different risk factors for pressure ulcers, and then attempt to predict the risk. Studies have not clearly shown one to be more valid. In fact, they're all relatively weak predictors, however they can still help to highlight risk factors, and that combined with your clinical judgment can help you to determine appropriate prevention measures. Links to these scales can be found in the resources section for this course.
pressure injury management[edit | edit source]
Let's talk about the three most important factors in pressure injury management.
- The first is offloading. These ones need to be offloaded close to a hundred percent of the time to be able to heal, except for specific procedures that won't allow it. Sufficient offloading requires a thorough assessment of the wound, the patient's mobility, and any other factors that may affect that offloading plan. Strategies should be implemented on all surfaces that the patient uses, so bed, wheelchair, bedside chair, couch, recliner, et cetera. Offloading may be accomplished through surface overlays, cushions, positioning, or mobilisation or all of the above.
- The next is adequate hydration and nutrition. So we've discussed this already, but nutrition is essential for both healing damaged tissue and for maintaining the health of undamaged tissue. Malnutrition leads to low protein and vitamin stores, which is going to impact wound healing. It also leads to weight loss, and then that exacerbates the bony prominences and further increases the risk of pressure injury. Protein or amino acids supplements may be beneficial to promote healing in those that are malnourished. These patients should receive a thorough nutritional assessment by a dietitian and a customised nutrition plan. But if that is not possible where you are, some of these basic recommendations can help.
- The third is prevention. So prevent any further ulcers. This is going to look different depending on every patient, their status, their skin assessment, their mobility and moisture assessment, education, all of these things. So we need to take that into consideration, but prevention is the key to avoid complications, improve quality of life, and reduce cost. It's estimated that the cost to prevent pressure ulcers is two to three times less the cost to treat them. You can find more information from the National Pressure Injury Preventions programme on how to prevent ulcers and those are included in the resources section for this course.
Non-Healing Surgical Wounds[edit | edit source]
non-healing surgical wounds These wounds occur when a surgical incision does not heal as expected.
- The prevalence of these types of wounds varies by surgery type and by location, depending on local surgical practices, general population health, and the area you're working. You may see a lot of these types of wounds or none at all.
factors that will increase the risk of a surgical wound not healing[edit | edit source]
- infection. This is typically seen within 30 days after surgery or within 90 days, if a prosthetic has been implanted.
- A weakened immune system, this goes along the lines of infection.
- Steroid use,
- multiple comorbidities, especially diabetes,
- smoking. It's important to know that abstinence from smoking for as little as four weeks will significantly improve incisional healing.
- Poor nutrition and hydration, which we've discussed previously.
- Older age, which is reduces our healing capacity.
- Being overweight or obese,
- surgeries lasting over two hours, emergency surgeries, abdominal surgery, or inadequate perfusion to the wound site for whatever reason.
signs of a non-healing surgical wound[edit | edit source]
- fever,
- excess drainage from the wound, especially purulent drainage or pus.
- Increased temperature at the wound site.
- Foul odour, that's going to indicate an infection possibly.
- And dehiscence or opening of the wound edges at the surgical incision. This most often occurs early in the healing process, about three to 10 days after surgery, but it can occur later, especially in the cases of latent infection. So something to keep in mind. Dehiscence is more commonly seen in abdominal, pelvic, or vascular surgeries. It also increases with age and those with a higher BMI.
management of non-healing surgical wounds[edit | edit source]
Let's cover the three most important factors for management of non-healing surgical wounds: The first is
- follow the surgeon's orders. So this may be recommendations or restrictions that could put undue stress on the areas it heals. It could include compression, weight bearing, tension on the skin or sutures, or possibly lifting restrictions. This is something you should work with the surgeon to kind of come up with a plan together.
- The second is nutrition. The body needs more protein, vitamins, and minerals than usual when attempting to heal tissue. So limit sugary, processed, and inflammatory foods. Increase water, plants, and protein, and then general protein requirements are 1.2 to 2 grams of protein per kilogram of body weight. And general water requirements are 30 to 40 millilitres per kilogram of body weight per day. So it might be beneficial to take a protein or amino acid supplement, pre and post-op, but this should always be discussed with the dietitian and surgeon first.
- The final recommendation is education. So these patients need to know about home management, any restrictions, dressing, cleaning, infection prevention, weight-bearing restrictions, anything that goes along with their particular surgery that they've had. Education is key because I find that if you can provide them with extra information, it's going to put them now on a good path, but if you don't provide them with enough information, they're kind of going to fill in the gaps on their own. And who knows where that's going to lead. If this is something that you're not comfortable with, please reach out to another professional that is and connect that patient with that person.
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Palmer, D. Characteristics and Identification of Wound Types. Physiotherapy Wound Care Programme. Plus. 2022.
- ↑ 2.0 2.1 Wound Source. Pressure Injuries, Deep Tissue Pressure Injury (DTPI). Available from: https://www.woundsource.com/patientcondition/pressure-injuries-deep-tissue-pressure-injury-dtpi (accessed 21/09/2022).