Moro Reflex: Difference between revisions
No edit summary |
(added video reference and other links) |
||
| Line 9: | Line 9: | ||
== Position == | == Position == | ||
'''Head Drop Method''': Supine position. Suspend the baby horizontally, in a symmetrical supine position such that the therapist's one hand behind the chest and the other supports the head. The infant's head should be in the midline position.<ref>Futagi Y, Toribe Y, Suzuki Y. [https://www.hindawi.com/journals/ijpedi/2012/191562/ The grasp reflex and moro reflex in infants: hierarchy of primitive reflex responses.] International journal of pediatrics. 2012 Oct;2012.</ref> | '''Head Drop Method''': Supine position. Suspend the baby horizontally, in a symmetrical supine position such that the therapist's one hand behind the chest and the other supports the head. The infant's head should be in the midline position.<ref name=":0">Futagi Y, Toribe Y, Suzuki Y. [https://www.hindawi.com/journals/ijpedi/2012/191562/ The grasp reflex and moro reflex in infants: hierarchy of primitive reflex responses.] International journal of pediatrics. 2012 Oct;2012.</ref> | ||
It is important to guarantee that both the infant's hands are open at the moment of elicitation of the reflex so as not to produce any asymmetrical response. Also, ensure that the baby is awake and not crying during the examination. | It is important to guarantee that both the infant's hands are open at the moment of elicitation of the reflex so as not to produce any asymmetrical response. Also, ensure that the baby is awake and not crying during the examination. | ||
| Line 30: | Line 30: | ||
===== Abnormal Response ===== | ===== Abnormal Response ===== | ||
Disintegration of the reflex within 2 to 3 months of age. | |||
Persistence of the response beyond 6 months of age. | Persistence of the response beyond 6 months of age. | ||
| Line 39: | Line 39: | ||
This reflex can be stimulated in all neonates during the first 12 weeks of age and disintegrates by 6 months of age. | This reflex can be stimulated in all neonates during the first 12 weeks of age and disintegrates by 6 months of age. | ||
{{#ev:youtube|PTz-iVI2mf4}} | {{#ev:youtube|PTz-iVI2mf4}}<ref>qumar81. Moro Reflex. Available from:https://www.youtube.com/watch?v=PTz-iVI2mf4&ab_channel=qumar81</ref> | ||
The examiner holds the infant in supine position and drops down the head slowly. Abduction of upper extremities followed by extension of arms with finger extended is seen. | |||
== Neural Mechanism == | == Neural Mechanism == | ||
This reflex is primarily elicited | This reflex is primarily elicited with the help of vestibular nuclei. It is mediated by the brainstem and therefore its centre seems to be in the lower region of the pons to the medulla. The efferent pathways of the response seem to originate in the vestibulospinal and/or reticulospinal neurons and the reflex movement is generated by the subcortical structures without cortical participation.<ref name=":0" /> | ||
== The Difference between Moro and Startle Reflex == | == The Difference between Moro and Startle Reflex == | ||
The startle | The startle reflex, the response to a sudden stimulus, is one of the defensive reactions and consists essentially of flexion movements. It differs from the Moro response which is characterized by extension. | ||
The startle reaction is induced by an auditory stimulus which shows clear habituation in premature infants, whereas the Moro reflex does not | |||
The startle reaction | The startle reaction can not be elicited in anencephalic newborns, while the Moro reflex was always elicited in these infants. | ||
== Clinical Significance == | == Clinical Significance == | ||
* The absence or premature disappearance of the Moro reflex can result from a birth injury, severe asphyxia during the birthing process, intracranial hemorrhage, infection, brain malformation, general muscular weakness of any cause, and cerebral palsy of the spastic type. | * The absence or premature disappearance of the Moro reflex can result from a birth injury, severe asphyxia during the birthing process, intracranial hemorrhage, infection, brain malformation, general muscular weakness of any cause, and cerebral palsy of the spastic type. | ||
* Asymmetrical Moro | * Asymmetrical Moro is said to be caused due to a local injury. | ||
* Damage to a peripheral nerve, cervical cord, or a fracture of the clavicle are common causes to an asymmetric Moro and causes inhibition of the reflex on the affected side. | * Damage to a peripheral nerve, cervical cord, or a fracture of the clavicle are common causes which leads to an asymmetric Moro Reflex and causes inhibition of the reflex on the affected side. | ||
* Prolonged retention of the | * Prolonged retention of the reflex is said to be a sign of spastic cerebral palsy. | ||
* | * A study showed a clear association between retained primitive reflexes and delay in motor development in very low birth weight infants.<ref>Edwards CW, Al Khalili Y. [https://www.ncbi.nlm.nih.gov/books/NBK542173/ Moro Reflex]. InStatPearls [Internet] 2020 Aug 30. StatPearls Publishing.</ref> | ||
* A hyperactive response of the reflex is a common feature of neonatal withdrawal from maternal drug abuse including volatile substances, heroin, and opioids and may also be detected in infants with a severe bilateral intrauterine disturbance such as hydranencephaly.<ref name=":0" /> | |||
* ADHD is linked to persistent Moro Reflex in school children.<ref>Konicarova J, Bob P. [https://link.springer.com/article/10.1007/BF03379591 Retained primitive reflexes and ADHD in children]. Activitas Nervosa Superior. 2012 Sep;54(3):135-8.</ref> | |||
== References == | == References == | ||
[[Category:Paediatrics - Assessment and Examination]] | [[Category:Paediatrics - Assessment and Examination]] | ||
[[Category:Neurological - Assessment and Examination]] | [[Category:Neurological - Assessment and Examination]] | ||
Revision as of 19:13, 30 June 2022
Introduction[edit | edit source]
It was first described by Ernst Moro in 1918 and is a primitive infantile reflex. It is easily confused with a startle pattern or reflex. This reflex is said to be of labyrinthine origin.
Position[edit | edit source]
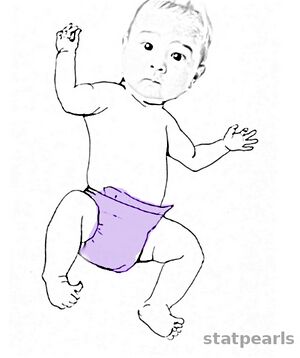
Head Drop Method: Supine position. Suspend the baby horizontally, in a symmetrical supine position such that the therapist's one hand behind the chest and the other supports the head. The infant's head should be in the midline position.[1]
It is important to guarantee that both the infant's hands are open at the moment of elicitation of the reflex so as not to produce any asymmetrical response. Also, ensure that the baby is awake and not crying during the examination.
Baby Drop Method: Same as the head drop method.
Stimulus[edit | edit source]
Head Drop Method: Dropping of the head of the baby by a few centimetres.
Baby Drop Method: The therapist lowers their hands rapidly about 10 to 20 cm and brings them to an abrupt halt.
Subcutaneous Stimulus: Painful stimulus to the subcutaneous tissue of the epigastrium.( considered to be a more sensitive technique)
Response[edit | edit source]
Normal Response[edit | edit source]
Initial Phase: Abduction of the upper extremities and extension of the arms. The fingers extend, and there is a slight extension of the neck and spine.
After Phase: Arms adduct and the hands come to the front of the body before returning to the infant's side.
Abnormal Response[edit | edit source]
Disintegration of the reflex within 2 to 3 months of age.
Persistence of the response beyond 6 months of age.
Asymmetrical response.
Duration[edit | edit source]
This reflex can be stimulated in all neonates during the first 12 weeks of age and disintegrates by 6 months of age.
The examiner holds the infant in supine position and drops down the head slowly. Abduction of upper extremities followed by extension of arms with finger extended is seen.
Neural Mechanism[edit | edit source]
This reflex is primarily elicited with the help of vestibular nuclei. It is mediated by the brainstem and therefore its centre seems to be in the lower region of the pons to the medulla. The efferent pathways of the response seem to originate in the vestibulospinal and/or reticulospinal neurons and the reflex movement is generated by the subcortical structures without cortical participation.[1]
The Difference between Moro and Startle Reflex[edit | edit source]
The startle reflex, the response to a sudden stimulus, is one of the defensive reactions and consists essentially of flexion movements. It differs from the Moro response which is characterized by extension.
The startle reaction is induced by an auditory stimulus which shows clear habituation in premature infants, whereas the Moro reflex does not
The startle reaction can not be elicited in anencephalic newborns, while the Moro reflex was always elicited in these infants.
Clinical Significance[edit | edit source]
- The absence or premature disappearance of the Moro reflex can result from a birth injury, severe asphyxia during the birthing process, intracranial hemorrhage, infection, brain malformation, general muscular weakness of any cause, and cerebral palsy of the spastic type.
- Asymmetrical Moro is said to be caused due to a local injury.
- Damage to a peripheral nerve, cervical cord, or a fracture of the clavicle are common causes which leads to an asymmetric Moro Reflex and causes inhibition of the reflex on the affected side.
- Prolonged retention of the reflex is said to be a sign of spastic cerebral palsy.
- A study showed a clear association between retained primitive reflexes and delay in motor development in very low birth weight infants.[3]
- A hyperactive response of the reflex is a common feature of neonatal withdrawal from maternal drug abuse including volatile substances, heroin, and opioids and may also be detected in infants with a severe bilateral intrauterine disturbance such as hydranencephaly.[1]
- ADHD is linked to persistent Moro Reflex in school children.[4]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Futagi Y, Toribe Y, Suzuki Y. The grasp reflex and moro reflex in infants: hierarchy of primitive reflex responses. International journal of pediatrics. 2012 Oct;2012.
- ↑ qumar81. Moro Reflex. Available from:https://www.youtube.com/watch?v=PTz-iVI2mf4&ab_channel=qumar81
- ↑ Edwards CW, Al Khalili Y. Moro Reflex. InStatPearls [Internet] 2020 Aug 30. StatPearls Publishing.
- ↑ Konicarova J, Bob P. Retained primitive reflexes and ADHD in children. Activitas Nervosa Superior. 2012 Sep;54(3):135-8.