Trochlear Nerve: Difference between revisions
No edit summary |
Nehal Khater (talk | contribs) mNo edit summary |
||
| (17 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Kehinde Fatola|Kehinde Fatola]] <br> | <div class="editorbox"> '''Original Editor '''- [[User:Kehinde Fatola|Kehinde Fatola]] <br> | ||
| Line 4: | Line 6: | ||
== Description == | == Description == | ||
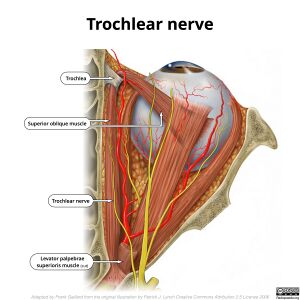
The trochlear nerve is the fourth [[Cranial Nerves|Cranial Nerve]] (CNIV) with the longest intracranial course, but also the thinnest<ref>Joo W, Rhoton Jr AL. [https://pubmed.ncbi.nlm.nih.gov/26223856/ Microsurgical anatomy of the trochlear nerve.] Clinical Anatomy. 2015 Oct;28(7):857-64.</ref>. It has a general somatic efferent (somatic motor) nerve, which innervates a single muscle (superior oblique muscle) on the contralateral side of its origin. <ref>Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. Philadelphia; Lippincott Williams and Wilkins, 2017</ref> | |||
== Course == | |||
[[File:Trochlear-nerve-illustration.jpg|alt=|thumb|300x300px|Trochlear nerve illustration]] | |||
The trochlear nerve appears from the dorsal region of the brainstem around the level of caudal mesencephalon below the inferior colliculus, it winds ventrally around the brainstem and | The trochlear nerve appears from the dorsal region of the brainstem around the level of caudal mesencephalon below the inferior colliculus, it winds ventrally around the brainstem and stretches forward to the eye through the subarachnoid space. It extends between the superior cerebellar and posterior cerebral arteries and penetrates the dura. It thereafter courses through the lateral wall of the cavernous sinus and joins three other cranial nerves – [[Oculomotor Nerve|oculomotor nerve]] (CN III), [[Abducens Nerve|abducens nerves]] (CN VI), as well as the first two branches of the [[Trigeminal Nerve|trigeminal nerve]] (CN V), ophthalmic (V1) and maxillary (V2). They enter the orbit via the superior orbital fissure where the trochlear nerve supplies the superior oblique muscle. <ref>Netter FH. Atlas of Human Anatomy. Philadelphia; Elsevier, 2019</ref> | ||
== Function == | == Function == | ||
The trochlear nerve transmits general somatic efferent impulses, which synapse in the skeletal fibers of the superior oblique muscle. The superior oblique muscles allow for depression, abduction, and medial rotation (intortion) of the eyeball. The superior oblique muscle's body is behind the eyeball, but its tendon (which is guided by the trochlea) approaches it from the front. The tendon attaches to the top (superior aspect) of the eyeball at a 51-degree angle to the eyeball's primary position (looking straight forward). As a result, the pull of the tendon has two components: a forward component that pulls the eyeball downward (depression), and a medial component that rotates the top of the eyeball toward the nose (intorsion). Depending on which way the eye is looking, the relative intensity of these two forces changes. | |||
* The force of depression rises when the eye is adducted (looking toward the nose). | |||
* The force of intorsion increases when the eye is abducted (looking away from the nose), whereas the force of depression diminishes. | |||
Contraction of the superior oblique induces depression and intorsion in nearly equal proportions when the eye is in the primary position (seeing straight ahead). '''In summary''', the superior oblique muscle causes: | |||
# Eyeball depression, especially when the eye is adducted. | |||
# Eyeball intorsion, especially when the eye is abducted. | |||
<div class="row"> | |||
<div class="col-md-6"> {{#ev:youtube|IQxs9PeWb1s|300}} <div class="text-right"><ref>#Trochlear nerve # 4th nerve. Available from: https://www.youtube.com/watch?v=IQxs9PeWb1s [last accessed 24/4/2022]</ref></div></div> | |||
<div class="col-md-6"> {{#ev:youtube|nzrAxyzR6VI|300}} <div class="text-right"><ref>Anatomy Dissected: Cranial Nerve IV (trochlear nerve). Available from: https://www.youtube.com/watch?v=nzrAxyzR6VI&list=PLlnL4HAGL-ONPYJBFq8No4AWJsd-OfYc0&index=4 [last accessed 24/4/2022]</ref></div></div> | |||
</div> | |||
== Clinical | == Clinical relevance == | ||
Trochlear nerve palsy may result from both peripheral – injury to nerve bundles or central – involvement of the trochlear nucleus, and lesions. Acute symptoms may indicate trauma, while chronic symptoms are mostly congenital. Vertical [[diplopia]] whereby injury causes weakness in the downward movement of the eyeball causing double vision due to unopposed actions of the other extraocular muscles, thereby producing two visual fields from either eye. Torsional [[diplopia]] affects the rotation of the eyeball in the plane of the face so that in tilting the head sideways, things look tilted in the affected eyeball while they remain vertical in the unaffected, thereby creating two visual fields. <ref name=":0">Hoya K, Kirino T. Traumatic Trochlear Nerve Palsy Following Minor Occipital Impact. Neurol Med Chir. 2000. 40:358-360.</ref> | |||
Trochlear nerve palsy may result from both peripheral – injury to nerve bundles or central – involvement of the trochlear nucleus, lesions. Acute symptoms may indicate trauma, while chronic symptoms are mostly congenital. Vertical diplopia whereby injury causes weakness in the downward movement of the eyeball causing double vision due to unopposed actions of the other extraocular muscles, thereby producing two visual fields from either eye | {{#ev:youtube|48MSBKRIrno}}<ref>Trochlear Nerve Palsy Rapid Review. Available from: https://www.youtube.com/watch?v=48MSBKRIrno [last accessed 24/4/2022]</ref> | ||
== Assessment == | == Assessment == | ||
The clinical implications of CN IV palsy are indicated by superior oblique weakness. This muscle depresses and abducts the eyeball when working independently. The extraocular muscles, on the other hand, synergistically move the eye. As a result, the trochlear nerve is tested by having the patient look 'down and in,' as the superior oblique contributes the most to this motion. Reading the newspaper and descending the stairs are two common hobbies that necessitate convergent gaze. [[Diplopia]] is a critical sign of CN IV palsy when these tasks are performed. <ref name=":0" /> | |||
== Treatment == | |||
[[Eye muscle exercise|Exercises]] may be prescribed to strengthen the superior oblique muscle. | [[Eye muscle exercise|Exercises]] may be prescribed to strengthen the superior oblique muscle. | ||
== References == | == References == | ||
<references /> | |||
[[Category:Nerves]] | |||
[[Category:Anatomy]] | |||
[[Category:Neurology]] | |||
[[Category:Neurological - Assessment and Examination]] | |||
Latest revision as of 17:21, 24 April 2022
Description[edit | edit source]
The trochlear nerve is the fourth Cranial Nerve (CNIV) with the longest intracranial course, but also the thinnest[1]. It has a general somatic efferent (somatic motor) nerve, which innervates a single muscle (superior oblique muscle) on the contralateral side of its origin. [2]
Course[edit | edit source]
The trochlear nerve appears from the dorsal region of the brainstem around the level of caudal mesencephalon below the inferior colliculus, it winds ventrally around the brainstem and stretches forward to the eye through the subarachnoid space. It extends between the superior cerebellar and posterior cerebral arteries and penetrates the dura. It thereafter courses through the lateral wall of the cavernous sinus and joins three other cranial nerves – oculomotor nerve (CN III), abducens nerves (CN VI), as well as the first two branches of the trigeminal nerve (CN V), ophthalmic (V1) and maxillary (V2). They enter the orbit via the superior orbital fissure where the trochlear nerve supplies the superior oblique muscle. [3]
Function[edit | edit source]
The trochlear nerve transmits general somatic efferent impulses, which synapse in the skeletal fibers of the superior oblique muscle. The superior oblique muscles allow for depression, abduction, and medial rotation (intortion) of the eyeball. The superior oblique muscle's body is behind the eyeball, but its tendon (which is guided by the trochlea) approaches it from the front. The tendon attaches to the top (superior aspect) of the eyeball at a 51-degree angle to the eyeball's primary position (looking straight forward). As a result, the pull of the tendon has two components: a forward component that pulls the eyeball downward (depression), and a medial component that rotates the top of the eyeball toward the nose (intorsion). Depending on which way the eye is looking, the relative intensity of these two forces changes.
- The force of depression rises when the eye is adducted (looking toward the nose).
- The force of intorsion increases when the eye is abducted (looking away from the nose), whereas the force of depression diminishes.
Contraction of the superior oblique induces depression and intorsion in nearly equal proportions when the eye is in the primary position (seeing straight ahead). In summary, the superior oblique muscle causes:
- Eyeball depression, especially when the eye is adducted.
- Eyeball intorsion, especially when the eye is abducted.
Clinical relevance[edit | edit source]
Trochlear nerve palsy may result from both peripheral – injury to nerve bundles or central – involvement of the trochlear nucleus, and lesions. Acute symptoms may indicate trauma, while chronic symptoms are mostly congenital. Vertical diplopia whereby injury causes weakness in the downward movement of the eyeball causing double vision due to unopposed actions of the other extraocular muscles, thereby producing two visual fields from either eye. Torsional diplopia affects the rotation of the eyeball in the plane of the face so that in tilting the head sideways, things look tilted in the affected eyeball while they remain vertical in the unaffected, thereby creating two visual fields. [6]
Assessment[edit | edit source]
The clinical implications of CN IV palsy are indicated by superior oblique weakness. This muscle depresses and abducts the eyeball when working independently. The extraocular muscles, on the other hand, synergistically move the eye. As a result, the trochlear nerve is tested by having the patient look 'down and in,' as the superior oblique contributes the most to this motion. Reading the newspaper and descending the stairs are two common hobbies that necessitate convergent gaze. Diplopia is a critical sign of CN IV palsy when these tasks are performed. [6]
Treatment[edit | edit source]
Exercises may be prescribed to strengthen the superior oblique muscle.
References[edit | edit source]
- ↑ Joo W, Rhoton Jr AL. Microsurgical anatomy of the trochlear nerve. Clinical Anatomy. 2015 Oct;28(7):857-64.
- ↑ Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. Philadelphia; Lippincott Williams and Wilkins, 2017
- ↑ Netter FH. Atlas of Human Anatomy. Philadelphia; Elsevier, 2019
- ↑ #Trochlear nerve # 4th nerve. Available from: https://www.youtube.com/watch?v=IQxs9PeWb1s [last accessed 24/4/2022]
- ↑ Anatomy Dissected: Cranial Nerve IV (trochlear nerve). Available from: https://www.youtube.com/watch?v=nzrAxyzR6VI&list=PLlnL4HAGL-ONPYJBFq8No4AWJsd-OfYc0&index=4 [last accessed 24/4/2022]
- ↑ 6.0 6.1 Hoya K, Kirino T. Traumatic Trochlear Nerve Palsy Following Minor Occipital Impact. Neurol Med Chir. 2000. 40:358-360.
- ↑ Trochlear Nerve Palsy Rapid Review. Available from: https://www.youtube.com/watch?v=48MSBKRIrno [last accessed 24/4/2022]