Practical Postural Techniques for Speech Therapists and Physiotherapists: Difference between revisions
No edit summary |
No edit summary |
||
| Line 15: | Line 15: | ||
== Evaluation in the Upright Position == | == Evaluation in the Upright Position == | ||
The visual assessment of a patient should start in an upright, neutral position. In this position, it is important to verify the function of the vestibulospinal reflex.<ref name=":0" /> The vestibulospinal reflex works to maintain balance and posture by coordinating head movement with the action of the spinal muscles.<ref>Casale J, Browne T, Murray I, et al. Physiology, Vestibular System. [Updated 2021 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: | The visual assessment of a patient should start in an upright, neutral position. In this position, it is important to verify the function of the vestibulospinal reflex.<ref name=":0" /> The vestibulospinal reflex works to maintain balance and posture by coordinating head movement with the action of the spinal muscles.<ref>Casale J, Browne T, Murray I, et al. Physiology, Vestibular System. [Updated 2021 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK532978/] </ref> The Rhomberg and Fukuda tests can be used to assess this function.<ref name=":0" /> | ||
=== Rhomberg Test === | === Rhomberg Test === | ||
| Line 170: | Line 170: | ||
== Whole Kinetic Chain == | == Whole Kinetic Chain == | ||
When correcting posture, consider the effect a change has both locally and globally. It is important to try to correct the whole kinetic chain | When correcting posture, consider the effect a change has both locally and globally. It is important to try to correct the whole kinetic chain:<ref name=":0" />For example, when actively correcting an anteversion / hyperlodosis of the lumbar spine (i.e. an inferior part), it may be necessary to correct a position further up the chain, such as a forward head position. | ||
== Nociceptive Stimuli == | == Nociceptive Stimuli == | ||
| Line 248: | Line 248: | ||
** Or all three parts of the larynx | ** Or all three parts of the larynx | ||
Finally assess the larynx when moving into cervical rotation. Repeat this movement, but ask the patient to inspire normally and then do a fast inspiration. Usually in fast inspiration, there will be traction on the inferior part of the larynx and a stabilisation of the upper part. This helps maintain the position of the upper part of the larynx.<ref name=":0" /> | Finally assess the larynx when moving into cervical rotation. Repeat this movement, but ask the patient to inspire normally and then do a fast inspiration. Usually in fast inspiration, there will be traction on the inferior part of the larynx and a stabilisation of the upper part. This helps maintain the position of the upper part of the larynx.<ref name=":0" /> | ||
== Potential Stretches == | |||
Based on the assessment findings, the following stretches can be beneficial for patients with tension / retraction of specific muscle chains.<ref name=":0" /> | |||
=== Anterior Muscle Chain === | |||
* Place two fingers on the inferior part of the mandible | |||
* Extend the cervical spine | |||
* Traction superiorly | |||
* Hold for 30 seconds and repeat three times | |||
=== Anterior Cross Chain === | |||
* Rotate patient's trunk to the ipsilateral side | |||
* Contralateral rotation of the patient's head | |||
* The patient opens his / her mouth | |||
* Anchor the shoulder | |||
* Traction | |||
* Hold for 30 seconds and repeat three times | |||
=== Posterior Cross Chain === | |||
* Ask the patient to open his / her mouth | |||
* Keep tension on the mandible and infrahyoid | |||
* Place the head in slight cervical extension | |||
* Depress the ipsilateral shoulder | |||
* Hold for 30 seconds and repeat three times | |||
== References == | == References == | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Physioplus Content]] | [[Category:Physioplus Content]] | ||
Revision as of 12:27, 14 July 2021
Top Contributors - Jess Bell, Kim Jackson and Kirenga Bamurange Liliane
Introduction[edit | edit source]
There is a known link between posture and vocal quality[1] and posture and swallowing.[2][3] When working with patients who have vocal problems or swallowing dysfunction, it is essential to be able to assess the impact of posture on these functions and vice versa.
This page will discuss the practical components of the postural assessment of a patient that may be useful for speech therapists. The theoretical aspects of the postural assessment are discussed here and here, and deglutition is discussed in detail here.
When assessing a patient’s posture, it is important to remain two or three metres from the patient in order to observe them fully. If you are using a postural grid app, it is important to be consistent in terms of the patient’s position each time you take pictures.[4] For more information on using digital photography as an aid to postural assessment, please see the following articles:
- Two-dimensional digital photography for child body posture evaluation: standardized technique, reliable parameters and normative data for age 7-10 years[5]
- Spinal postural alignment measurements using markerless digital photography[6]
Evaluation in the Upright Position[edit | edit source]
The visual assessment of a patient should start in an upright, neutral position. In this position, it is important to verify the function of the vestibulospinal reflex.[4] The vestibulospinal reflex works to maintain balance and posture by coordinating head movement with the action of the spinal muscles.[7] The Rhomberg and Fukuda tests can be used to assess this function.[4]
Rhomberg Test[edit | edit source]
The Rhomberg test is performed as follows:[4][8]
- The patient stands with his / her feet together and arms crossed or held next to the body
- This position should be held for 30 seconds with eyes open, and then for 30 seconds with eyes closed
- The therapist observes the patient from the front and back
- In a normal test, there will be a slight, gentle oscillation
- In an abnormal test, the patient:
- Is unable to maintain the test position without opening his / her eyes
- Has to increase his / her base of support to maintain the position
- Experiences large oscillations
If your patient has an abnormal Rhomberg, it is necessary to stop testing and refer on for medical review as it may indicate a neurological problem.[4]
Fukuda Test[edit | edit source]
The Fukuda test evaluates the tension of the rotatory action of the postural chain[4] and is performed as follows:[4][10]
- The patient stands with arms extended in a circle with a radius of one metre
- This circle is divided into sections
- The patient is asked to step in place 50 times with his / her eyes closed and try not to move from his / her initial position
- The room should be quiet and dimly lit in order to reduce the chance that patients use light or sound to orient themselves
- The angle of rotation (i.e. deviation) and the distance of displacement (i.e. lateral shift) is measured
- A result is considered abnormal when a patient:[10]
- Deviates more than 45 degrees
- Has more than a one metre lateral shift
Test Progressions[edit | edit source]
If the patient has a normal Rhomberg and Fukuda test, it is possible to further destabilise the system in order to evaluate the effect of the masticatory system and deglutition on postural control.[4]
Deglutition[edit | edit source]
Repeat the Rhomberg test, but ask the patient to swallow while his / her eyes are closed. Look for:[4]
- Lateral or posterior destabilisation
- Inclination (i.e. bending) or rotation of the head
Teeth in Contact[edit | edit source]
Remain in the Rhomberg position and ask the patient to close his / her mouth. Look for increased tension of the posterior chain.[4]
Decoaptation (i.e. opening) of TMJ[edit | edit source]
While in Rhomberg test position, place two balls of cotton wool between the teeth on each side and observe if this has any impact on postural control.[4]
These progressions can then be assessed during the Fukuda test.
Posterior Analysis[edit | edit source]
The posterior observation provides information about:[4]
- Tension in the shoulder elevators or altered scapula position
- Head inclination
- Asymmetry of the pelvis - e.g. lateral displacement
- Asymmetry in the lumbar paravertebral muscle mass
- A difference in the space between the arms and the trunk on each side
- Feet, ankle, knee alignment / position
Once you have completed a basic visual assessment, ask the patient to breathe in and out. Look specially for any elevation of the shoulder instead of lateral movement of the ribs.
Profile Analysis[edit | edit source]
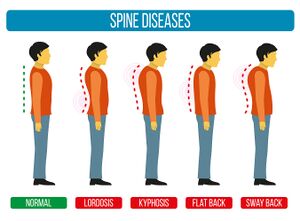
From the side (see Figure 2), the therapist should observe the patient’s alignment, looking specifically at:[4][12]
- Head position
- Cervical spine alignment
- Thoracic spine alignment
- Lumbar spine alignment
Then consider if and how this position changes during swallowing, respiration and singing.[4]
On inspiration, look for:[4]
- Changes to the neutral position
- Retraction of the anterior part of the laryngeal chain
On swallowing, look for any large excursions:[4]
- Slight flexion of the head during swallowing can be normal, but it can indicate retraction of the anterior laryngeal chain
- This type of retraction can be modified with re-education and with manual therapy
Frontal Analysis[edit | edit source]
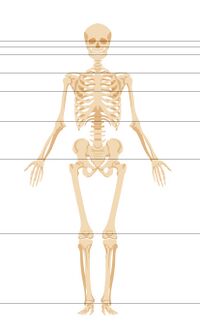
When observing a patient from the front, it is important to check if the following points are horizontally aligned (see Figure 2):[4]
- Bi-pupilar line
- Bi-condylar line
- Bi-mammillary line
- Bi-styloid line
- Bi-iliac line
- Bi-patellar line
- Bi-malleolar line
In order to further challenge the postural system while observing the patient in this position, ask the patient to open and close his / her mouth. Look for normal descent of the larynx and observe and palpate the anterior part of the hyoid.[4]
Next check for movement during respiration and fast inspiration. Check if there is more movement in the upper chest, the lateral part of the chest or in the abdomen. Singers tend to use the inferior part of their abdomen more for inspiration than their upper chest.[4]
During respiration, it is important to also observe the upper part of the neck and the head. Look for any flexion or extension (particularly during fast inspiration).[4]
It is not possible to assess the diaphragm directly. However, it is possible to observe the muscles in the abdomen and use specific reference points in order to observe the effect of displacement of the visceral muscles during inspiration.[4]
Analysis in Sitting[edit | edit source]
Specific postural patterns may be apparent in sitting including a forward head position. If a patient spends a lot of time in this position, his / her anterior chain may be retracted. You can observe sitting in profile or from the front.[4]
Ask the patient to correct his / her posture, and see if he / she can maintain this position. Then assess inspiration in sitting. Check for:[4]
- The amount of movement on inspiration - the abdomen moves less freely in sitting
- Extension of the head
- Forward position of the head
- Elevation of the shoulders
- Tension of the anterior neck
Then assess swallowing in the sitting position. During swallowing, look for:[4]
- Neutral position of the head
- Correct movement of the larynx and hyoid
- Any compensations (rotation, flexion, bending of the head)
Finally, test glissato (glide from one pitch to another) and staccato (short, separate notes). During glissato, look for:[4]
- Extension, flexion, or rotation during phonation
- Any tension of the perilaryngeal muscle masses (best observed from in front of the patient)
It is possible to ask the patient to increase the glissato range in order to evaluate perilaryngeal muscle effort and the impact of this range on the cervical spine - in individuals who have no dysfunction, the client will be able to maintain a neutral position at higher pitches.[4]
During staccato, look at the movement of the larynx:[4]
- The larynx should elevate and descend
- Check for any lateral movement or rotation of the larynx
It can be difficult to assess movement of the larynx, but it is possible to palpate movement with one finger. While palpating, also assess for any lateral tension or pain from the perilaryngeal muscles, the hyoid and hyoid muscles.[4]
When asking patients to correct their posture, there are three potential outcomes:[4]
- The patient can actively correct the problem without the help of the therapist
- For these patients, it is useful to prioritise active rehabilitation
- The patient can correct his / her posture, but only with the help of the therapist
- If there is pain, treatment priority is given to techniques that ease pain and to increase range of motion with passive manual therapy
- Once pain is better managed, it is possible to move on to active rehabilitation
- The patient cannot correct his / her posture or if he / she can move, this postural correction causes pain
- In these cases, treatment priority is on pain management, often with medical treatments (medication, surgery)
- Passive treatments may be beneficial to maintain range of motion / proprioceptive control
When there is pain, it is necessary to consider red flags:[4]
Necessary Compensations[edit | edit source]
In some instances, compensation may be necessary to achieve respiration or swallowing. When there is a neurological problem, it is important to respect the condition of the patient and to maintain respiration / deglutition, even if there are postural compensations.[4]
Whole Kinetic Chain[edit | edit source]
When correcting posture, consider the effect a change has both locally and globally. It is important to try to correct the whole kinetic chain:[4]For example, when actively correcting an anteversion / hyperlodosis of the lumbar spine (i.e. an inferior part), it may be necessary to correct a position further up the chain, such as a forward head position.
Nociceptive Stimuli[edit | edit source]
The temporomandibular joint (TMJ), the masticatory system, masticatory muscles (e.g. masseter, temporalis, digastric etc) and trigger points can be sources of pain.[4][15][16] In order to assess these areas:[4]
- Place two fingers anteriorly to the ear in order to palpate the articular zone of the TMJ
- Move slightly anterior to palpate the TMJ capsule
- Move slightly anteriorly again, to palpate masseter.
Ask the patient to open his / her mouth and feel for movement of the TMJ - the mandible condyle rotates at the beginning of the movement and then slides forward.[17][18]
To further assess the TMJ:[4]
- Place two fingers in the patient’s mouth
- Look for symmetry of movement between sides
- Feel for cracking / other noises of the TMJ or pain etc
- Assess masseter bulk / size and compare sides
- Look for fibrosis, adhesions or trigger points
Ask the patient to maximally open his / her mouth and measure this distance with the finger test:[4]
- Two fingers = the minimum normal
- Three fingers = normal (when this is pain free, without problems)[19][20]
It is useful to assess for muscle hardness and trigger points in muscles such as:[4][15][21]
- Masseter
- Temporalis
- Pterygoids
- Mylohyoid
- Sternocleidomastoid
Trigeminal Nerve[edit | edit source]
The following points may be painful on palpation if there is an activation of the trigeminal nerve in cases of TMJ:[4]
- Orbicular / ophthalmic area
- Maxillary part of the trigeminal nerve
- Middle and upper part of sternocleidomastoid
To determine if a radicular problem may be causing a patient’s symptoms (rather than TMJ or laryngeal system dysfunction), the Spurling’s test can be used.[22] Pain in neck or cervical spine frequently indicates articular pain only. A positive Spurling’s is when there is a reproduction of radiculopathy symptoms (often referring to the arm).[4][22]
Neck Range of Motion[edit | edit source]
Starting with extension, look for:[4]
- Lateralisation of the larynx
- Ipsilateral traction
- Tension of the hyoid muscles, scalenes
- Upper chest compensation
Then ask the patient to flex. Look for:[4]
- Posterior tension
- Alteration of the posterior masses
Ask the patient to rotate and look for:[4]
- Anterior displacement of the head, which may be caused by tension of sternocleidomastoid, the peri-laryngeal area and the scalenes
- Compensation from the shoulder and other parts of the chest
Ask the patient to maintain a neutral position and to then move into side bending. Typically, a patient should be able to side bend and remain facing forwards (i.e. no rotation).
While assessing the cervical spine, also look at the movement of the larynx:[4]
- Place three fingers on the hyoid, thyroid cartilage, cricoid cartilage
- Have the patient breathe in and out
- On inspiration, it is important to determine if there is traction and which parts are affected:
- The cricoid
- The thyroid cartilage
- Or the hyoid, thyroid cartilage and the cricoid
Then ask the patient to move into cervical assessment and assess the movement of the larynx:[4]
- Look for lateralisation and displacement and consider where it occurs:
- Upper part only (hyoid)
- Middle part only (thyroid)
- Or all three parts of the larynx
Finally assess the larynx when moving into cervical rotation. Repeat this movement, but ask the patient to inspire normally and then do a fast inspiration. Usually in fast inspiration, there will be traction on the inferior part of the larynx and a stabilisation of the upper part. This helps maintain the position of the upper part of the larynx.[4]
Potential Stretches[edit | edit source]
Based on the assessment findings, the following stretches can be beneficial for patients with tension / retraction of specific muscle chains.[4]
Anterior Muscle Chain[edit | edit source]
- Place two fingers on the inferior part of the mandible
- Extend the cervical spine
- Traction superiorly
- Hold for 30 seconds and repeat three times
Anterior Cross Chain[edit | edit source]
- Rotate patient's trunk to the ipsilateral side
- Contralateral rotation of the patient's head
- The patient opens his / her mouth
- Anchor the shoulder
- Traction
- Hold for 30 seconds and repeat three times
Posterior Cross Chain[edit | edit source]
- Ask the patient to open his / her mouth
- Keep tension on the mandible and infrahyoid
- Place the head in slight cervical extension
- Depress the ipsilateral shoulder
- Hold for 30 seconds and repeat three times
References[edit | edit source]
- ↑ Caçador M, Paço J. The influence of posture and balance on voice: a review: A influência da postura e do equilíbrio na voz: revisão. Gaz Med [Internet]. 2018;5(2).
- ↑ Bordoni B, Morabito B, Mitrano R, Simonelli M, Toccafondi A. The anatomical relationships of the tongue with the body system. Cureus. 2018;10(12):e3695.
- ↑ Alghadir AH, Zafar H, Al-Eisa ES, Iqbal ZA. Effect of posture on swallowing. Afr Health Sci. 2017;17(1):133-7.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 4.23 4.24 4.25 4.26 4.27 4.28 4.29 4.30 4.31 4.32 4.33 4.34 4.35 4.36 4.37 4.38 4.39 4.40 4.41 4.42 4.43 4.44 4.45 Banfi M. Practical Assessment for Postural Principles Useful in Speech Therapy Course. Physioplus, 2021.
- ↑ Stolinski L, Kozinoga M, Czaprowski D, Tyrakowski M, Cerny P, Suzuki N et al. Two-dimensional digital photography for child body posture evaluation: standardized technique, reliable parameters and normative data for age 7-10 years. Scoliosis Spinal Disord. 2017;12:38.
- ↑ Hida M, Wada C, Imai R, Kitagawa K, Okamatsu S, Ohnishi T et al. Spinal postural alignment measurements using markerless digital photography. J Orthop Surg (Hong Kong). 2020;28(3):2309499020960834.
- ↑ Casale J, Browne T, Murray I, et al. Physiology, Vestibular System. [Updated 2021 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK532978/]
- ↑ Forbes J, Cronovich H. Romberg Test. [Updated 2020 Sep 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: [/www.ncbi.nlm.nih.gov/books/NBK563187/|https://www.ncbi.nlm.nih.gov/books/NBK563187/]
- ↑ Clinical Examination Videos. Rombergs test/sign - Proprioception balance test. Available from: https://www.youtube.com/watch?v=H8VbKdRS-hg [last accessed 14/7/2021]
- ↑ 10.0 10.1 Zhang YB, Wang WQ. Reliability of the Fukuda stepping test to determine the side of vestibular dysfunction. J Int Med Res. 2011;39(4):1432-7.
- ↑ NEUROLOGY MADE INTERESTING. Fukuda stepping test aka Unterberger test. Available from: https://www.youtube.com/watch?v=ljGJbokAOXM [last accessed 14/7/2021]
- ↑ Czaprowski D, Stoliński Ł, Tyrakowski M, Kozinoga M, Kotwicki T. Non-structural misalignments of body posture in the sagittal plane. Scoliosis Spinal Disord. 2018;13:6.
- ↑ Finucane LM, Downie A, Mercer C, Greenhalgh SM, Boissonnault WG, Pool-Goudzwaard AL et al. International framework for red flags for potential serious spinal pathologies. J Orthop Sports Phys Ther. 2020;50(7):350-372.
- ↑ Rushton A, Rivett D, Carlesso L, Flynn T, Hing W, Kerry R. International Framework for Examination of the Cervical Region for potential of vascular pathologies of the neck prior to Orthopaedic Manual Therapy (OMT) Intervention: International IFOMPT Cervical Framework. International Federation of Orthopaedic Manipulative Physical Therapists (IFOMPT). 2020.
- ↑ 15.0 15.1 Zieliński G, Byś A, Szkutnik J, Majcher P, Ginszt M. Electromyographic patterns of masticatory muscles in relation to active myofascial trigger points of the upper trapezius and temporomandibular disorders. Diagnostics (Basel). 2021;11(4):580.
- ↑ Procópio Pinheiro R, Gaubeur MA, Itezerote AM, Saleh SO, Hojaij F et al. Anatomical study of the innervation of the masseter muscle and its correlation with myofascial trigger points. J Pain Res. 2020;13:3217-26.
- ↑ Reboredo V. Physiology of the Temporomandibular Joint Course. Physioplus, 2021.
- ↑ Bordoni B, Varacallo M. Anatomy, Head and Neck, Temporomandibular Joint. [Updated 2021 Feb 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: /www.ncbi.nlm.nih.gov/books/NBK538486/|https://www.ncbi.nlm.nih.gov/books/NBK538486/
- ↑ Agrawal J, Shenai PK, Chatra L, Kumar PY. Evaluation of normal range of mouth opening using three finger index: South India perspective study. Indian J Dent Res. 2015;26(4):361-5.
- ↑ Zawawi KH, Al-Badawi EA, Lobo SL, Melis M, Mehta NR. An index for the measurement of normal maximum mouth opening. J Can Dent Assoc. 2003;69(11):737-41.
- ↑ Okada-Ogawa A, Sekine N, Watanabe K, Kohashi R, Asano S, Iwata K et al. Change in muscle hardness after trigger point injection and physiotherapy for myofascial pain syndrome. J Oral Sci. 2019 Mar 28;61(1):36-44. doi: 10.2334/josnusd.17-0453. Epub 2018 Dec 20. PMID: 30568046.
- ↑ 22.0 22.1 Jones SJ, Miller JMM. Spurling Test. [Updated 2020 Sep 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: /www.ncbi.nlm.nih.gov/books/NBK493152/|https://www.ncbi.nlm.nih.gov/books/NBK493152/