Re-engagement in Life Roles with Pain Conditions: Difference between revisions
Michelle Lee (talk | contribs) No edit summary |
Michelle Lee (talk | contribs) No edit summary |
||
| Line 31: | Line 31: | ||
The therapist can assit in the re-engagment of functional and vocational roles in the person with persistent pain. There are several areas in which they can work with indivudals in pain, this can include aiding the acceptance of pain and that there may not be a cure, goal setting, pacing, and self management strategies. | The therapist can assit in the re-engagment of functional and vocational roles in the person with persistent pain. There are several areas in which they can work with indivudals in pain, this can include aiding the acceptance of pain and that there may not be a cure, goal setting, pacing, and self management strategies. | ||
Another essential role the therapist must apply is establishing expectations of the patient. Commonly patients have been to many therapists perviously and had hands on treatments, where treatments were done to them. Re-engagment in activities in patients with persistent pain needs to be self driven with guidance from the therapist, so it is clear to establish this in order to move forward. | |||
=== Acceptance === | === Acceptance === | ||
| Line 47: | Line 49: | ||
This is a vital step in the engaement of the patient with persistent pain. It is essential that the Physiotherapist assist the patient to identify their own goals. This may include prompts from what they perviously could do and to help them to identify what activites they value. This involvement in the decision making process can help with the patient's overall satifaction of the service. The assessment of goals can be done through an informal conversation or though a more formal questionaire - which may help to prompt them with what activities they would like to be able to do again. It is important to remember that the patient is the expert in their own pain so empowering them from the beginning is the key. | This is a vital step in the engaement of the patient with persistent pain. It is essential that the Physiotherapist assist the patient to identify their own goals. This may include prompts from what they perviously could do and to help them to identify what activites they value. This involvement in the decision making process can help with the patient's overall satifaction of the service. The assessment of goals can be done through an informal conversation or though a more formal questionaire - which may help to prompt them with what activities they would like to be able to do again. It is important to remember that the patient is the expert in their own pain so empowering them from the beginning is the key. | ||
Activley involving patients in the decision making and goal setting aims to give autonomy, control and responsibility back to the patient. If the patient is activley identifiing their unique problems they are said to be more likely to find solutions to these problems, again empowering the individual and giving them tools for self-management. This process should be guided by the Physiotherapist not lead and all activities which are avoided by the patient should be identified. The Physiotherapist should then be willing to discuss each of these activities and goals with the patient to help them develop these goals into SMART goals - Specific, Measurable, Achievable, Realistic and Timed. | Activley involving patients in the decision making and goal setting aims to give autonomy, control and responsibility back to the patient. If the patient is activley identifiing their unique problems they are said to be more likely to find solutions to these problems, again empowering the individual and giving them tools for self-management. This process should be guided by the Physiotherapist not lead and all activities which are avoided by the patient should be identified. The Physiotherapist should then be willing to discuss each of these activities and goals with the patient to help them develop these goals into SMART goals - Specific, Measurable, Achievable, Realistic and Timed. | ||
=== Pacing === | |||
Pacing is a tool that can help address the boom and bust cycle or also known as the over-acitivty and under-activity cycles as discussed above. This is a tool that can be used to re-engage patients back into activity gradually and move them away from this boom and bust cycle. (Main et al 2008 page 332) | |||
Most activities are driven and paced through the patient's pain levels. They do an activity until they become fatigued or pain restricts them. This strategy aims to empower the patient to drive a set activity through cognitive awareness, but is essential that this tool does not feed into the avoidance of activities. (McCracken and Samuel 2007 page 333). | |||
=== | Pacing should be set on the goals made in patnership with the patient and can apply to any task. Pacing may include: | ||
*Breaking an activity into smaller parts (e.g ironing - do 2-3 items at a time not the whole basket) | |||
*Alternating activities ( e.g do the 2-3 items of ironing then chop vegetables for tea, then do 2-3 items more of ironing) | |||
*Introducing activity (we know 10 minutes of walking agravates your pain so walk for 7-8 and gradually increase this without causing pain) | |||
*Planning activites ( if you know shopping takes an hour and walking around the supermarket aggravates your pain, shop somewhere where there is a cafe and take a break, make sure you have planned enough time in your day to do so) | |||
It is important to educate the patient on pacing to engage them and to involve pacing to work towards their goal. If they do not fully understand the process they are likely to either not be interested and not engage in the activity or poorly implement the tool and find it unuseful. (lee et al 2009) | |||
Have a look at Peter Moores video on pacing: | |||
{| width="300" align="center" cellpadding="1" cellspacing="1" | |||
|- | |||
| {{#ev:youtube|WxpWyBtYaIs|300}} | |||
|} | |||
Revision as of 13:29, 18 April 2016
Introduction[edit | edit source]
Each and every person has different roles within their life. There are workplace roles and domestic roles within their personal and family lifestyles. These roles are of value to each individual, and can give the individual a sense of purpose. These roles that are developed can be severely impacted by pain and especially persistent pain. (pain book)
Pain does not just impact the individual greatly but also the economy. The cost of musculoskeletal pain in the workplace is significant. Whether the cause of the pain is work related or not, it can have a costly impact on the economy. Work places are trying to implement strategies to keep the cost of return to work (RTW) down by introducing early interventions and keeping people at work with putting supportive measures in place. (pain book ref 1st chapter -23)
Disengagement in Function and Vocational Roles[edit | edit source]
There is a spectrum of which people with chronic pain can sit upon. Those who are actively trying to manage their pain and continue with their roles and others who struggle to find strategies and slowly lose their roles.
People in pain can become aware of the stigma and prejudges that society can label them with. Pain is invisible and is a very personal experience; what may effect one person in one way does not necessarily affect another in the same, which can lead to negative opinions being formed.
Fear of pain also plays a vital role in function and engagement in activities of daily living. Fear of pain has been said to be more disabling than the pain itself ( vlaeyen and linton 2000). Fear of pain can then trigger fear avoidance behaviours, which can then lead into a downward spiral of the ‘Pain Cycle’ (strong 1989). People then start to avoid activities and situations where their pain may become irritated or where they feel they may be exposed to negative stigma or comments, such as exercise, social situations, and domestic chores.
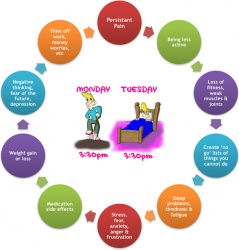
Take a look at the Pain Cycle by the Peter Moore from the Pain Toolkit.
Alongside the Pain Cycle people can find themselves in a boom and bust pattern, where for example; Monday their pain is undercontrol, so they get as much done as they can, but Tuesday their pain is aggravated so they spend the next 2 days resting and recoving. This can lead to a lack of fitness so the next time their pain is undercontrol they can't do as much due to the lack of strength and fitness and their pain is aggravated much sooner and this goes on. Take a look at the explantion in this this video clip.
Role of the Physiotherapist / Physical Therapist [edit | edit source]
The therapist can assit in the re-engagment of functional and vocational roles in the person with persistent pain. There are several areas in which they can work with indivudals in pain, this can include aiding the acceptance of pain and that there may not be a cure, goal setting, pacing, and self management strategies.
Another essential role the therapist must apply is establishing expectations of the patient. Commonly patients have been to many therapists perviously and had hands on treatments, where treatments were done to them. Re-engagment in activities in patients with persistent pain needs to be self driven with guidance from the therapist, so it is clear to establish this in order to move forward.
Acceptance[edit | edit source]
'Acceptance has been said to be an important step in sucessful adjustment' (pain book). It has also been linked with decreased levels of pain, decrease levels of disability, increased engagement in activity and decreased levels of depression and anxity.
Acceptance as mentioned above has been said to be the key to sucessful adjustment. There is currently a lot of work on Acceptance and Commitment Therapy (ACT) being used with people who have persistant pain. In summary this approach looks at the person accepting they have pain and being mindful about what they are experiencing. A person who applies restrictions to the things they value in life such as "I can't do X, Y or Z until I get rid of my pain" is seen as a form of non-acceptance of a sence that is unavoidable. This then inducing the suffering experienced from pain. ACT aims to promote the psychological flexibility and mindfulness of thoughts, feelings and behaviours associated with pain. (ACT PHD PDF)
Goal Setting [edit | edit source]
This is a vital step in the engaement of the patient with persistent pain. It is essential that the Physiotherapist assist the patient to identify their own goals. This may include prompts from what they perviously could do and to help them to identify what activites they value. This involvement in the decision making process can help with the patient's overall satifaction of the service. The assessment of goals can be done through an informal conversation or though a more formal questionaire - which may help to prompt them with what activities they would like to be able to do again. It is important to remember that the patient is the expert in their own pain so empowering them from the beginning is the key.
Activley involving patients in the decision making and goal setting aims to give autonomy, control and responsibility back to the patient. If the patient is activley identifiing their unique problems they are said to be more likely to find solutions to these problems, again empowering the individual and giving them tools for self-management. This process should be guided by the Physiotherapist not lead and all activities which are avoided by the patient should be identified. The Physiotherapist should then be willing to discuss each of these activities and goals with the patient to help them develop these goals into SMART goals - Specific, Measurable, Achievable, Realistic and Timed.
Pacing[edit | edit source]
Pacing is a tool that can help address the boom and bust cycle or also known as the over-acitivty and under-activity cycles as discussed above. This is a tool that can be used to re-engage patients back into activity gradually and move them away from this boom and bust cycle. (Main et al 2008 page 332)
Most activities are driven and paced through the patient's pain levels. They do an activity until they become fatigued or pain restricts them. This strategy aims to empower the patient to drive a set activity through cognitive awareness, but is essential that this tool does not feed into the avoidance of activities. (McCracken and Samuel 2007 page 333).
Pacing should be set on the goals made in patnership with the patient and can apply to any task. Pacing may include:
- Breaking an activity into smaller parts (e.g ironing - do 2-3 items at a time not the whole basket)
- Alternating activities ( e.g do the 2-3 items of ironing then chop vegetables for tea, then do 2-3 items more of ironing)
- Introducing activity (we know 10 minutes of walking agravates your pain so walk for 7-8 and gradually increase this without causing pain)
- Planning activites ( if you know shopping takes an hour and walking around the supermarket aggravates your pain, shop somewhere where there is a cafe and take a break, make sure you have planned enough time in your day to do so)
It is important to educate the patient on pacing to engage them and to involve pacing to work towards their goal. If they do not fully understand the process they are likely to either not be interested and not engage in the activity or poorly implement the tool and find it unuseful. (lee et al 2009)
Have a look at Peter Moores video on pacing: