Triangular Fibrocartilage Complex Injuries
Original Editor - Kristen Mason
Top Contributors - Kristen Mason, Admin, Kim Jackson, Laura Ritchie, Rachael Lowe, Lucinda hampton, Jess Bell, Shauni Van Overstraeten, 127.0.0.1, Shaimaa Eldib, Evan Thomas, Kai A. Sigel, WikiSysop, Wanda van Niekerk and Joseph Ayotunde Aderonmu
Introduction[edit | edit source]
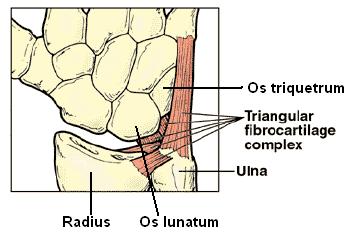
- The triangular fibrocartilage complex (TFCC) is a load-bearing structure between the lunate, triquetrum, and ulnar head.
- The function of the TFCC is to act as a stabilizer for the ulnar aspect of the wrist.
- The TFCC is at risk for either acute or chronic degenerative injury.
- Forced ulnar deviation and positive ulnar variation carry associations with injuries to the TFCC.
- Patients with TFCC injury will present with ulnar-sided wrist pain that may present with clicking or point tenderness between the pisiform and the ulnar head.
- TFCC is reported to accompany distal radius fracture[1]s in 39 to 84% of cases
- MRI imaging is useful as a preliminary diagnostic tool; arthroscopy is the diagnostic gold standard.
- Treatment options include conservative therapies such as rest, NSAIDs, and corticosteroid injections as well as operative management.[2]
- Prognosis for TFCC injury is generally favorable.
This 2 minute video is worth watching
Clinically Relevant Anatomy[edit | edit source]
The Triangular Fibrocartilage Complex is the ligamentous and cartilaginous structures that separate the radiocarpal from the distal radioulnar joint. The TFCC consists of an articular disc, meniscus homologue, ulnocarpal ligament, dorsal & volar radioulnar ligament and extensor carpi ulnaris sheath.
- Origin: Medial border of distal radius
- Insertion: Base of ulnar styloid
- Vascular Supply: central disc is avascular, peripheral blood vessels penetrate TFCC margins
- Function of TFCC: Main stabilizer of distal radioulnar joint (volar portion of TFCC prevents dorsal displacement of ulna and is tight in pronation and dorsal portion of TFCC prevents volar displacement of ulna and is tight in supination). Contributes to ulnocarpal stability[4][5]
Etiology[edit | edit source]
- Occurs with compressive load on TFCC during marked ulnar deviation
- Commonly associated with positive ulnar variance (radial shortening, average of 4.5 mm)
- Forced ulnar deviance (i.e. swinging bat, racket, etc) causes increased load on TFCC[5]
Pathophysiology[edit | edit source]
Anatomically the TFCC includes the triangular fibrocartilage disc, extensor carpi ulnaris tendon subsheath, ulnotriquetral and ulnolunate ligaments, dorsal and volar distal radioulnar ligaments, meniscal homolog, and the ulnocarpal collateral ligament.
- The triangular fibrocartilage disc attachment on the radial side is to hyaline cartilage, which makes this weaker compared to the ulnar side’s bony attachment.
- Positive ulnar variation can leave the TFCC vulnerable to injury.
- Ulnar variation will decrease with supination and increase with pronation.
- Small changes in ulnar length have been shown to have substantial effects on the amount of load to the ulna.
- The extensor carpi ulnaris relies on the TFCC for movement, and thus alteration of the motion of the extensor carpi ulnaris may lead to abnormal force through the TFCC, predisposing it to injury[2]
Clinical Presentation[edit | edit source]
- Patients will complain of ulnar-sided wrist pain that often gets worse with activity.
- There may also be a weakness in the grip, instability, or clicking[6].
- There are some elements of the history which can occur in conjunction with individual sports, for example, baseball-specific acute injury can be due to forced wrist extension while doing a head-first slide or when a hitter attempts to hit an inside pitch and gets “jammed.”
- Chronic injury can occur in baseball players as a result of the heavy load placed on the wrist during the swing. These athletes can sustain TFCC injuries even if they do not have positive ulnar variance[2]
- In gymnastics the TFCC can be injured through overuse injury (both support skills and hanging elements). With repetitive weight bearing (both compressive and tensile), this area can become inflamed and tendonitis/tendonosis can develop in the anchoring wrist ligaments (often misdiagnosed as a wrist sprain).[7]
Diagnostic Procedures[edit | edit source]
Physical Examination[edit | edit source]
On exam, palpation of the TFCC is best with the wrist in pronation. It is between the flexor carpi ulnaris, ulnar styloid, and os pisiform. Several physical exam tests can suggest the diagnosis of TFCC injury. These include:
- TFCC compression test: forearm in the neutral position with ulnar deviation reproduces symptoms
- TFCC stress test: applying a force across the ulna with the wrist in ulnar deviation reproduces symptoms
- Press test: Patient lifts themselves out of a chair using the wrists in an extended position. Pain indicates a positive test.
- Supination test: Patient grabs the underside of a table with the forearms supinated; this causes a load on the TFCC and dorsal impingement, which will cause pain if there is a peripheral, dorsal tear.
- Piano key test: Place both hands on an exam table and press the palms on the table. If the distal ulna is prominent on the affected side, this suggests distal radioulnar joint instability which can have associations with TFCC injury. If the palms are relaxed and the ulnar head goes back to normal position, this is a positive test
- Grind test: Compress the radius and ulna and have the patient rotate the forearm. Pain could indicate a degenerative process[2]
Diagnostic Imaging[edit | edit source]
- Radiographs: may reveal avulsion of ulnar styloid, scaphoid fracture, distal radial fracture, volar tilt of lunate or triquetrum; ulnar variance.
- Triple Injection Arthrography: identification of tear (low specificity).
- MRI: identification of tear (high sensitivity and specificity).
Outcome Measures[edit | edit source]
- DASH Outcome Measure
- Modified Mayo Wrist Score
- Activities of Daily Living Score [8][9]
Management / Interventions[edit | edit source]
Conservative Treatment[edit | edit source]
- The rehabilitation program should consist of rest, activity modification to remove the inciting force of injury, ice application and splint immobilisation for 3 to 6 weeks
- After the immobilisation, the patient should receive physical therapy[10]
Surgical Intervention[edit | edit source]
Surgical options should be a consideration if conservative treatment fails or if there is DRUJ instability. Surgical treatment will depend on the Palmer classification of the injury [11]
- The Palmer classification is the most recognized scheme for TFCC lesions ,It divides them into these two categories (with subdivisions, beyond the scope of this articles):
Traumatic and Degenerative .This classification provides an accurate anatomic description of tears, it does not guide treatment or indicate prognosis
Common surgical options include arthroscopic repair, arthroscopic debridement, ulnar shortening, and the Wafer procedure.
A debridement is a surgical option that induces bleeding to stimulate healing. Debridement has beneficial outcomes for central TFCC tears but has been shown to have worse outcomes in degenerative tears or patients with higher positive ulnar variance.
Physiotherapy[edit | edit source]
- Initial treatment includes rest, physical therapy, and corticosteroid injections.
- The length of time to attempt conservative treatment before advancing to surgical options varies.
- Six months of conservative treatment is reasonable if there is not DRUJ (distal radioulnar joint) instability.[2]
Post-Operative Rehabilitation[edit | edit source]
Recovery after surgery varies, but typically four to six weeks should be expected for arthroscopy and approximately three months for an open approach. Patients will undergo physical therapy after the procedure. The exact time to begin physical therapy and the length of physical therapy depends on the type of surgery performed and the surgeon’s preference.[2]
For type 1 injuries
- Wrist will be immobilised for 1 week after the arthroscopy.
- After one week, range of motion exercises can be started.[12][13]
- A TFCC tear is a common injury in golf, boxing, tennis, water skiing, gymnastics, pole vaulting and hockey.
- Golf players and tennis players who suffer from a stable TFCC tear are able to start light activity ball contact at 3 weeks after the arthroscopy. They can return to their normal sports activity in 4 to 6 weeks.[14]
- When the symptoms remain, ulnocarpal corticosteroid injection can be an option.[15][16]
For more severe injuries, post-operative immobilisation in a Muenster cast for 4 weeks may be considered.
- After 4 weeks: the wrist is placed in a short arm splint or Versa wrist splint, which allows progressive motion to the wrist.
- The immobilisation will decrease the wrist pain and aggravation, which could improve healing.
- Some types of splints will help stabilise the wrist, which will lead to an improvement in hand function.[17]
- Patients can then start with range of motion and grip-strengthening exercises.[18][19]
- Therapists are more likely to give eccentric grip strengthening exercises, because this will have an influence on the co-activation pattern of the wrist-flexors, which help stabilise the wrist.[20][21][22]
- Other co-activation exercises can also be included to improve the global wrist stability.[23]
At 8 weeks post operative:
- Active muscle training should be started
- A graded pain-free exercise program is recommended.
- Physiotherapy management should include patient education and activity modification.[24]
- Isometric exercises should be included to help strengthen the area and reduce the risk of instability.[25][26]
- In particular, unilateral isometric exercises are beneficial as they have been found to increase voluntary muscle activation bilaterally. This may be because the motor cortex is stimulated, resulting in greater neuromuscular control.[27][28] In addition, controlled isometric activation of pronator quadratus in supination and neutral wrist position will help to stabilise the distal radioulnar joint (DRUJ). This can be used pre- and postoperatively in patients with TFCC injuries.[29]
- At 3 months: postoperatively patients are likely to resume normal activity.
- It takes a further 3 to 4 months to return to normal sports activities.[30]
Passive Mobilisation[edit | edit source]
Initially, a traction of the radiocarpal and the midcarpal joints can be used to determine whether this provokes pain.[31][32]
- To promote the wrist flexion, a dorsal sliding technique can be used.
- To promote the wrist extension, the volar sliding technique can be used.
- To promote the radial deviation the ulnar sliding technique can be used.
- To promote the ulnar deviation, the radial sliding technique can be used.

General Mobility Exercises[edit | edit source]
The patient should perform general mobility exercises[33][34][35]:
- Wrists rotations.
- Horizontal ulnar and radial deviation.
- Active pronation and supination.
- Stretching flexion and extension of the wrist.
Strengthening Exercises[edit | edit source]
At the end of the therapy, then move on to Strengthening exercises. The following exercises are all done with a weight in the hands or with a terra tire.[36]
- Flexion and extension.
- Pronation and supination.
Differential Diagnosis[edit | edit source]
- Hypothenar hammer syndrome: Differentiate because there may be discoloration, fingertip ulcers, or splinter hemorrhages on the fourth or fifth digits. Angiogram may be able to diagnose this condition.
- Ulnar carpal impingement: Differentiate because this is commonly a result of ulnar shortening due to surgical resection from a prior injury.
- Ulnar extensor or flexor muscle tendonitis: Movements that cause the muscle to fire will provoke the pain. Pain may radiate along the muscle belly depending on the degree of inflammation.
- DRUJ chondral lesions or osteoarthritis: Differentiate via radiographic evidence suggestive of a chondral lesion or osteoarthritis.
- Ulnar Styloid Impingement Syndrome: Symptoms consistent with TFCC injury, but the TFCC is intact.[2]
Conclusion[edit | edit source]
- The best outcomes with TFCC injuries will occur when other etiologies of ulnar-sided wrist pain are ruled out with initiation of conservative treatment.
- If the patient does not improve under conservative management, the next step is a surgical consultation obtained in a timely fashion.
- If an MRI is obtained (read by a radiologist who has experience with TFCC injuries).
- An interprofessional team of a nurse, physical or occupational therapist, and physician will provide the best follow-up care[2].
References[edit | edit source]
- ↑ Im J, Kang SJ, Lee SJ. A comparative study between conservative and surgical treatments of triangular fibrocartilage complex injury of the wrist with distal radius fractures. Clin Orthop Surg. 2021 Mar;13(1):105-9.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 Casadei K, Kiel J. Triangular fibrocartilage complex (TFCC) injuries. InStatPearls [Internet] 2020 Jan 20. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK537055/ (last accessed 5.4.2020)
- ↑ Marpole Physio What is a Triangular Fibrocartilage Complex Injury of the Wrist Available from: https://www.youtube.com/watch?v=pnk9cB9kMy8 (last accessed 5.4.2020)
- ↑ Verheyden JR, Palmer AK. EMedicine. Triangular Fibrocartilage Complex. http://emedicine.medscape.com/article/1240789-overview. (accessed 25 June 2009).
- ↑ 5.0 5.1 Wheeless CR. Wheeless' Textbook of Orthopaedics. Triangular Fibrocartilage Complex. http://www.wheelessonline.com/ortho/triangular_fibrocartilage_complex (accessed 25 June 2009).
- ↑ UK Orthopaedic Surgery & Sports Medicine. Health in Sports Report-Issue 6: Triangular Fibrocartilage Complex (TFCC) Injury. http://ukhealthcare.uky.edu/sportsmedicine/health_in_sports/issue6.asp (accessed 25 June 2009).
- ↑ Gymnastics Injuries TFCC Available from:https://gymnasticsinjuries.wordpress.com/tag/tfcc/ (last accessed 6.4.2020)
- ↑ Reiter A, Wolf MB, Schmid U, Frigge A, Dreyhaupt J, Hahn P, et al. Arthroscopic repair of palmer 1B triangular fibrocartilage complex tears. Arthroscopy. 2008;24(11):1244-1250.
- ↑ Estrella EP, Hung LK, Ho PC, Tse WL. Arthroscopic repair of triangular fibrocartilage complex tears. Arthroscopy. 2007;23(7):729-737.
- ↑ Parmelee-Peters, K., & Eathorne, S. (2005). The Wrist: Common Injuries and Management. Primary Care, Clinics in Office Practice, 35-70.
- ↑ Kavi Sachar, Ulnar-Sided Wrist Pain: Evaluation and Treatment of Triangular Fibrocartilage Complex Tears, Ulnocarpal Impaction Syndrome, and Lunotriquetral Ligament Tears, journal of hand surgery, july 2012,
- ↑ Rettig AC, Athletic Injuries of the wrist and hand, part 1: traumatic injuries of the wrist. Am J Sports Med 2003:31(6):1038-48
- ↑ de Araujo W, Poehling GG, Kuzma GR., New Tuohy Needle Technique for Triangular Fibrocartilage Complex Repair: Preliminary Studies, Arthroscopy. 1996 Dec 12, 699-703.
- ↑ Rettig AC, Athletic Injuries of the wrist and hand, part 1: traumatic injuries of the wrist. Am J Sports Med 2003:31(6):1038-48
- ↑ Kavi Sachar, Ulnar-Sided Wrist Pain: Evaluation and Treatment of Triangular Fibrocartilage Complex Tears, Ulnocarpal Impaction Syndrome, and Lunotriquetral Ligament Tears, journal of hand surgery, july 2012
- ↑ de Araujo W, Poehling GG, Kuzma GR., New Tuohy Needle Technique for Triangular Fibrocartilage Complex Repair: Preliminary Studies, Arthroscopy. 1996 Dec 12, 699-703.
- ↑ Prosser R, Herbert R, LaStayo PC., Current Practice in the Diagnosis and Treatment of Carpal Instability—Results of a Survey of Australian Hand Therapists, Journal of hand therapy, 2007 Jul-Sep 20, 239-42
- ↑ Rettig AC, Athletic Injuries of the wrist and hand, part 1: traumatic injuries of the wrist. Am J Sports Med 2003:31(6):1038-48
- ↑ Corso SJ, Savoie FH, Geissler WB, Whipple TL, Jiminez W, Jenkins N., A rthroscopic Repair of Peripheral Avulsions of the Triangular Fibrocartilage Complex of the Wrist: A Multicenter Study, the journal of arthroscopy and related surgery, 1997 Feb, 78-84.
- ↑ Prosser R, Herbert R, LaStayo PC., Current Practice in the Diagnosis and Treatment of Carpal Instability—Results of a Survey of Australian Hand Therapists, Journal of hand therapy, 2007 Jul-Sep 20, 239-42
- ↑ Hagert E., Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on the Rehabilitation of the Wrist, Journal of Hand Therapy, 2010 Jan-Mar 23, 2-16
- ↑ Prof. Dr. R. Meeusen, Praktijkgids pols- en handletsels, VUB, p131-151
- ↑ Hagert E., Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on the Rehabilitation of the Wrist, Journal of Hand Therapy, 2010 Jan-Mar 23, 2-16
- ↑ Prosser R, Herbert R, LaStayo PC., Current Practice in the Diagnosis and Treatment of Carpal Instability—Results of a Survey of Australian Hand Therapists, Journal of hand therapy, 2007 Jul-Sep 20, 239-42
- ↑ Hagert E., Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on the Rehabilitation of the Wrist, Journal of Hand Therapy, 2010 Jan-Mar 23, 2-16
- ↑ Prosser R, Herbert R, LaStayo PC., Current Practice in the Diagnosis and Treatment of Carpal Instability—Results of a Survey of Australian Hand Therapists, Journal of hand therapy, 2007 Jul-Sep 20, 239-42
- ↑ Hagert E., Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on the Rehabilitation of the Wrist, Journal of Hand Therapy, 2010 Jan-Mar 23, 2-16
- ↑ Lee M, Gandevia SC, Carroll TJ., Unilateral strength training increases voluntary activation of the opposite untrained limb., Clin Neurophysiol. 2009;120:802–8.
- ↑ Hagert E., Proprioception of the Wrist Joint: A Review of Current Concepts and Possible Implications on the Rehabilitation of the Wrist, Journal of Hand Therapy, 2010 Jan-Mar 23, 2-16
- ↑ Rettig AC, Athletic Injuries of the wrist and hand, part 1: traumatic injuries of the wrist. Am J Sports Med 2003:31(6):1038-48
- ↑ Prof. Dr. R. Meeusen, Praktijkgids pols- en handletsels, VUB, p131-151.
- ↑ Wadsworth, C., The wrist and hand examination ans Interpretaion, J. Orthopedic and sports physical therapy, 1983, 108-20
- ↑ Leger AB, Milner TE. , Muscle function at the wrist after eccentric exercise, Medicine and Science in Sports and Exercise, 2001;33:612–20.
- ↑ Prof. Dr. R. Meeusen, Praktijkgids pols- en handletsels, VUB, p131-151.
- ↑ Wadsworth, C., The wrist and hand examination ans Interpretaion, J. Orthopedic and sports physical therapy, 1983, 108-20
- ↑ Prof. Dr. R. Meeusen, Praktijkgids pols- en handletsels, VUB, p131-151.