Retinoblastoma
Original Editor - Kapil Narale
Top Contributors - Kapil Narale and Kim Jackson
Introduction[edit | edit source]
Retinoblastoma (historically called glioma retinae) is a malignant tumor that occurs in the developing retina. [1] It is the most common ocular cancer that occurs in the pediatric population, generally under 5 years of age. [1][2] It is lethal if it is left untreated. [2] Retinoblastoma can be unifocal or multifocal. It is seen that 60% of individuals have unilateral retinoblastoma, and are diagnosed at 24 months, while 40% of individuals have bilateral retinoblastoma and are diagnosed at 15 months. When retinoblastoma has a genetic onset, there can be a risk of retinoblastoma and/or non-ocular tumors. [1]
Common Terminology[edit | edit source]
Retinoblastoma can be classified into various types:
Unilateral - one eye is affected. About 60% of affected individuals have unilateral retinoblastoma when diagnosed at 24 months. With unilateral retinoblastoma, the tumor is usually unifocal, which means that there is only one tumor present. It is possible that there may be multifocal tumors in one eye, which would be a unilateral multifocal retinoblastoma. In most people who have unilateral retinoblastoma, without the presence of family history, if the tumor is large, it is impossible to determine if it is a single tumor.
Bilateral - both eyes are affected. About 40% of affected individuals have bilateral retinoblastoma when diagnosed at 15 months. In children with bilateral, retinoblastoma, both eyes are affected when the condition is first diagnosed. It is possible that both eyes may present with multiple tumors. It is also possible that some children may initially have unilateral retinoblastoma, and may develop a tumor in their unaffected eye.
Trilateral - if bilateral, or seldom unilateral, retinoblastoma and a pinealoblastoma develop.
Retinoma and associated eye lesions - benign retinal tumors (retinoma) which cease in growth may be present in retinal scars. Calcified phthisic eyes may occur from automatic ceasing of retinoblastoma relating to vascular occlusion. The spectrum of RB1 pathogenic variants in those with retinoma and a family history of retinoblastoma, and individuals who had retinoma in one eye and either retinoma or retinoblastoma in the other eye present similarly to individuals with bilateral retinoblastoma. [1]
Pinealoblastomas - This occurs in "retina-like" tissue in the pineal gland. If there is a simultaneous occurrence of pinealoblastomas or primitive neuroectodermal tumors and retinoblastoma, this would be classified as trilateral retinoblastoma. This is a rare condition, and is generally fatal, whereas retinoblastoma of the eye can be cured. [1]
Epidemiology[edit | edit source]
In high-income countries, retinoblastoma is known to be a curable disease, with close to 100% chance of survival. However, in middle- and low-income countries, the prognosis is extremely low. In addition, more than 80% of cases occur in these countries. [2]
It is estimated that the majority of retinoblastoma cases occur in Asia (53%), then Africa (29%), Latin America (8%), North America (3%), and Europe (6%). With this information, it is seen that global retinoblastoma patient survival is <30%. It is seen that the survival rate is 40% (23‑70%) in low‑income countries, while it is 79% (54‑93%) in upper‑middle‑income countries. [2]
The incidence of retinoblastoma can be between 1 in 15 000 to 1 in 20 000 live births, therefore there is a very low chance of it occurring. [1]
Family History[edit | edit source]
Heritable retinoblastoma can be transmitted via autosomal dominance. It is common that only one offspring in a family can be affected, which would be known as a simplex case. An RB1 pathogenic variant may be inherited from an affected parent. There is a 50% chance for each child of an affected parent to inherit the RB1 pathogenic variant.
Mode of Inheritance[edit | edit source]
Genetically transmitted retinoblastoma is an autosomal dominant disorder.
Genetically spreading the disorder within a family can occur through:
- Genetic transmission through parents
- Depending on the genotype and phenotype of the parents, can be transmitted to siblings of an affected individual.
- Genetic transmission to the offspring of the affected individual
- Can be genetically spread to other family members depending on the parents of the affected individual, and the parent's families.
Assessment[edit | edit source]
Prior to examining the patient, a thorough assessment must be completed. If there is any family history of the condition, a germline mutation may be present, and the child may need to undergo systemic chemotherapy to prevent pineoblastoma, even with a unilateral presentation of the disease. [2]
An in-depth evaluation is warranted prior to determining the degree of the necessary treatment, and minimise and prevent any occurrences of secondary complications. [2]
The treatment decision for retinoblastoma is dependent on the International Classification of Retinoblastoma (ICRB) classification (similar to the ICF), the presence of extraocular clinical factors, germline test results, family psychosocial status, and available medical facility resources. If there is presence of a germline disease, genetic testing should be conducted in all cases of retinoblastoma, for the patient and the rest of their family. [2]
All patients should go through a baseline high‑resolution simple and contrast‑enhanced magnetic resonance imaging (MRI) of the brain and orbits. Special attention should be given for pineoblastoma or any features of disruption to the optic nerve. [2]
As a part of the assessment, complete blood count, urine sample, and a general physical examination are performed by the pediatric oncologist. Subsequent to the general physical examination, a detailed examination using anesthesia is conducted, where ICRB staging is confirmed, and the first treatment can be administered. [2]
Signs, Symptoms and Findings[edit | edit source]
Signs that retinoblastoma can be ruled in include: [1]
- Leukocoria (white pupillary reflex)
- Strabismus (may occur with or before leukocoria)
- Change in eye appearance
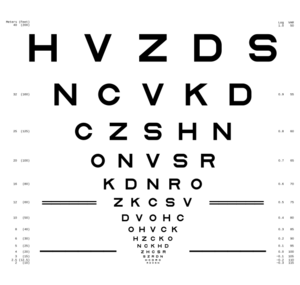
- Reduced visual acuity
Signs that infrequently occur include, glaucoma, orbital cellulitis, uveitis, hyphema, or vitreous hemorrhage. As mentioned, it is most common in children under 5 years of age. Abnormal occurrences are more common in older children.
Heritable retinoblastoma can be ruled in with:
- Diagnosis of retinoblastoma, including unilateral (unifocal and multifocal) and bilateral involvement
- Retinoma
- Family history of retinoblastoma
Diagnosis[edit | edit source]
Retinoblastoma can be diagnosed via proband by retinal examination with the pupils dilatated. This would be conducted by an ophthalmologist or optometrist. The individual would need to be examined under anaesthesia to confirm the diagnosis and the extent of the disease. A biopsy may allow the tumor to spread past the eye, thus putting the individual's life at risk, thus should be avoided. [1]
The diagnosis of heritable retinoblastoma is determined via genetic transmission of retinoblastoma or retinoma and a family history of retinoblastoma. However, it is seen that many individuals with retinoblastoma are without a family history of the condition. In order to determine if the retinoblastoma is heritable, individuals would need to have a heterozygous germline RB1 pathogenic variant identified on molecular genetic testing. Identification of an RB1 pathogenic variant through the genetic transmission can facilitate early diagnosis and screening for family members at risk for retinoblastoma. [1]
Examination of the fundus of the eye through indirect ophthalmoscopy can be used as a method of diagnosis. This can be confirmed with imaging studies, which will also help confirm the stage of the tumor. [1]
In a developing retina, retinoblastomas can form subsequent to biallelic inactivation of RB1 in a cone cell precursor. Genetic retinoblastoma can be diagnosed in a proband, with retinoblastoma or retinoma, which is a benign potential precursor to retinoblastoma, and a family history of retinoblastoma or a heterozygous germline pathogenic variant in RB1 which can be denoted by molecular genetic testing. Epigenetic hypermethylation of the RB1 promotor results in inactivation of RB1. This cannot be transmitted by the germline. A non-genetic onset of retinoblastoma can occur with MYCN in a developing retinal cone cell. [1]
The following sequence has been outlined for those with retinoblastoma and/or genetically caused retinoblastoma, which outlines the genetic risk of a germline pathogenic variant in RB1: [1]
| Hx | Individual with unknown or insufficient evidence of a constitutional (germline) RB1 pathogenic variant |
|---|---|
| Ho | Individual who did not inherit a known familial germline RB1 pathogenic variant which can be confirmed by molecular genetic testing |
| Ho* | Individual with unilateral retinoblastoma or retinoma without a germline RB1 pathogenic variant identified with molecular genetic testing; residual risk of mosaicism is <1% |
| H1 | Individual with bilateral retinoblastoma, trilateral retinoblastoma (retinoblastoma with intracranial central nervous system midline embryonic tumor), retinoblastoma and with a family history, or denotation of a germline RB1 pathogenic variant |
Testing Approaches[edit | edit source]
Molecular genetic testing approaches for heritable retinoblastoma include single gene testing, and chromosomal microarray (CMA): [1]
Single-gene testing [1]
- This can be carried out on individuals with bilateral, unilateral familial, or unilateral multifocal retinoblastoma. Within this process, sequence analysis and gene-targeted deletion/duplication analysis of RB1 are administered on peripheral blood DNA.
- For individuals with unilateral unifocal retinoblastoma and without a family history
- With an unavailable tumor tissue, sequence analysis and gene-targeted deletion/duplication analysis of RB1 are administered on peripheral blood DNA.
- With the availability of the tumor tissue, sequence analysis and gene-targeted deletion/duplication analysis of RB1 are performed on tumor DNA.
- With the identification of pathogenic variants, the testing of DNA from blood is carried out to identify these variants.
- If pathogenic variants are not detected in the tumor, methylation analysis of the RB1 promoter CpG island is carried out, which denotes epigenetic inactivation of RB1 resulting from hypermethylation of the RB1 promoter. If hypermethylation is not depicted at the promoter, the DNA from the tumor is analysed for the amplification of MYCN. This leads to the cause of unilateral, non-heritable retinoblastoma without RB1 pathogenic variants in 1.5% of individuals with isolated unilateral retinoblastoma.
Chromosomal Microarray [1]
- This method uses oligonucleotide or SNP arrays, instead of sequence analysis, to detect genome-wide large deletions/duplications (including RB1). CMA may be appropriate in individuals who have retinoblastoma relating to a developmental delay, and/or other congenital anomalies.
Differential Diagnosis[edit | edit source]
There are many childhood ocular hereditary conditions that can represent retinoblastoma. These conditions are: [1]
- NDP-related persistent fetal vasculature and NDP-related Coats disease
- Tuberous sclerosis complex
- Norrie disease
- Incontinentia pigmenti
- Familial exudative vitreoretinopathy
- Von Hippel-Lindau syndrome
- Ocular infestation by Toxocara canis
Treatment[edit | edit source]
Although, as mentioned, retinoblastoma can be lethal if it is left untreated, having an early diagnosis can help reduce morbidity and increase quality of life. It is best when the patient receives multidisciplinary care from various healthcare professionals such as ophthalmologist, pediatric oncologist, pathologist, and radiation oncologist. Treatment options can be dependent on tumor stage, number of tumor foci (unifocal, unilateral multifocal, or bilateral), localisation and size of the tumor(s) within the eye(s), vitreous seeding presence, any possibility of effective vision, intensity and type of extraocular extension, and available resources. Therefore, the initial goal of treatment would be to save the individual's life, followed by their sight. [1]
The response to the initial treatment can be an indication of long‑term prognosis. The decision made by the ocular oncologist, in regards to treatment, would be crucial, as the therapy provided would need to be a sufficient strength, while minimising any secondary toxic effects. [2] Enucleation has been the preferred mode of treatment, for advanced retinoblastoma, in low-middle-income countries. however, over the last 30 years, the globe-savaging techniques have been used. [2]
Although the management of retinoblastoma may differ from place to place, and from clinic to clinic, the overall structure of treatment involves a similar framework. [2]
There are various treatment options that can be utilized, which include, [1][2]
- Intravenous Chemotherapy (IVC)
- Intra-arterial Chemotherapy (IAC), in addition to or followed by laser or cryotherapy
- Intraocular Chemotherapy
- Intravitreal Chemotherapy
- Precision Intravitreal Chemotherapy
- Intracameral Chemotherapy
- Focal Therapies
- Cryotherapy,
- Transpupillary Thermotherapy (TTT)
- External Beam Radiotherapy - this would be used as a last resort
- Plaque Radiotherapy
- Enucleation
Treatment Agents to Avoid[edit | edit source]
In individuals who have genetically transmitted retinoblastoma, it is best to avoid radiation especially from x-rays, CT scans, and external beam radiation, and DNA disrupting agents such as tobacco or UV light. This will help reduce any risks of future malignant neoplasms. It is possible that cancer risk may be minimised with limiting chemotherapy. [1]
Intravenous Chemotherapy[edit | edit source]
Intravenous Chemotherapy (IVC) is an important mechanism for retinoblastoma therapy. It consists of 2-4 chemotherapeutic agents, which are given monthly via a central or peripheral catheter for 6-9 continuous cycles. The most commonly used method consists of 3 drugs, vincristine, etoposide, carboplatin (VEC). There ae cases where cyclophosphamide may replace vincristine when there may be a concern for neurotoxicity. Despite this, vincristine is more likely to cause myelosupression and hemorrhagic cystitis. Another difference between VEC and cyclophosphamide is that transfusion of blood components may be necessary, granulocyte colony‑stimulating factor is usually not needed with standard VEC doses, but should be used with cyclophosphamide.
Intravenous chemotherapy is known to effectively reduce tumor size, therefore can be referred to as chemo-reduction.
Focal consolidation with thermotherapy, involving cryotherapy or transpupillary thermotherapy (TTT), can help with tumor control. Cryotherapy followed by chemotherapy is seen to heighten drug availability to the intraocular spaces when given within 48 hours of the thermal disruption.
Indications for IVC consist of,
- Patients with bilateral disease,
- Confirmed germline mutation,
- Family history of retinoblastoma, or
- Instances with possible optic nerve or choroidal invasion.
Patients weighing less than 6 kg that are awaiting intra‑arterial chemotherapy (IAC). This is referred to as ‘bridge therapy’. As well, IVC acts as protection with preventing long‑term secondary cancers, metastases, and pineoblastoma.
Signs, symptoms, and side effects of systemic chemotherapies can include transient alopecia, cytopenia, and fever. Systemic toxicity of IVC for retinoblastoma can generally be mild.
A scheduled prophylaxis is administered for pneumocystis jirovecii pneumonia. Side effects or symptoms such as chemotherapy‑induced nausea, emesis, and constipation may be medically managed.
In terms of effects on the renal system, long‑term renal toxicity is unlikely to occur if chemotherapeutic agents are provided in proper amounts and concentrations.
Infertility is unlikely to occur with recommended doses of IVC. There can be a risk of infertility in males with the addition of melphalan, especially with a total dose of 140 mg/m2.
Another rare condition following the use of IVC is secondary acute myelogenous leukemia. This is correlated with increased doses of chemotherapy, with simultaneous external beam radiotherapy (EBRT) and other facilitating factors and conditions.
Intra-Arterial Chemotherapy[edit | edit source]
Intra-arterial Chemotherapy (IAC) is used especially for unilateral tumors. This method is known to be more expensive, due to its sophisticated procedure. Due to its expense and specialisation required, it is not used in developing countries. [1]
It is performed in an angiography suite by an experienced neurosurgeon or interventional neuroradiologist. A microcatheter is directed by fluoroscopy to specifically guide the chemotherapeutic agents into the ophthalmic artery. [1]
IAC is seen to have a 10x higher chemotherapy dose, compared to IVC, that is transmitted into the eye. As mentioned for the IVC treatment, the chemotherapy treatment has 1-3 drugs transmitted into the eye, once a month, for an average of 3 sessions. [1]
IAC has been more commonly used over the past decade, especially due to its efficacy with globe salvage in advanced retinoblastoma cases and refractory tumors. [1]
Indications for IAC can include first‑line, and globe salvage therapies. It can be used as a primary therapy for non‑germline, unilateral, or as a secondary therapy for unilateral or bilateral advanced recalcitrant disease facing enucleation. IAC has high efficacy from preventing sub retinal and vitreous seeds, especially when proximal to the retina. [1]
IAC can also be used as tandem therapy for advanced bilateral cases, minimal exposure (<2 cycles), and for a repeat treatment after an initial IAC treatment. However, tandem therapy may be questionable because of increased vascular toxicity in the eye with better acuity, an effect on pineoblastoma prevention that is unknown, and minimal effect on pre‑existing metastases, which can lead to higher chance of child mortality. [1]
High risk retinoblastoma needs enucleation performed, and an additional 6‑9 cycles of high‑dose IVC to prevent metastatic disease. IAC is generally used for patients older than 3 or 4 months old, because of the smaller size and strength of vessels in younger individuals. In the younger individuals, bridge therapy with IVC is provided until the individual reaches a weight of 6 kg. [1]
Signs, Symptoms, Side-effects[edit | edit source]
Even though there is a localised delivery of chemotherapeutic agents, systemic toxicity is generally observed after IAC. [1]
Transient neutropenia has been observed in 12% of patients. [1]
Femoral artery occlusion and blue toe syndrome can occur. This can be managed and prevented using anticoagulation. [1]
Complications that are more severe such as carotid artery dissection, stroke, and death, are possible, but hardly occur. The selection of appropriate treatments for individual patients is important. Undetected extraocular extension, optic nerve or massive choroidal invasion could lead to metastasis if a patient is treated with the use of IAC without systemic chemotherapy. [1]
Periocular side effects are generally self‑limited. These include, [1]
- Periorbital edema,
- Cutaneous hyperemia,
- Madarosis,
- Blepharoptosis,
- Scalp hair loss, and
- Extraocular dysmotility.
Serious ophthalmic vascular impairments can include, [1]
- Choroidal occlusive vasculopathy,
- Branch or central retinal artery occlusion,
- Ophthalmic artery spasm or occlusion, or
- Vitreous hemorrhage, among others
Of the individuals treated primarily with IAC, rhegmatogenous retinal detachment, which may be secondary due to accelerated tumor regression of endophytic tumors, is reported in 8‑16% of cases. [1]
Vascular impairments are not associated with reduced globe salvage, but can limit visual acuity. Risk for vascular impairments is similar whenever the IAC treatment is used. [1]
Intraocular Chemotherapy[edit | edit source]
Intravitreal Chemotherapy[edit | edit source]
Intravitreal Chemotherapy (IvitC) was found to be effective when used with IAC. This combination helped to save many damaged eyes. [2]
Indications for IvitC is the identification of a refractory or reemergent vitreous seeds subsequent to other interventions. It is hardly used as a primary intervention, but as a globe salvage therapy, if there is uncertainty of the initial tumor. Contraindications include. identification of a tumor or vitreous seeds at the planned site of needle entry, tumor invasion of the pars plana, and anterior chamber seeding. This can be safely administered with a thorough examination and the use of ultrasound bimicroscopy. [1]
Melphalan and/or topotecan are the most common pharmacological agents used in IvitC. The recommended doses, to effectively control vitreous seeds and prevent any toxic side effects, are 20‑30 μg, every 2‑4 weeks. [1]
Precision Intravitreal Chemotherapy[edit | edit source]
Precision Intravitreal Chemotherapy (p-IvitC) was initially used to treat localised vitreous seeding. This method is a modification of the general treatment for diffuse vitreous seeds. It was developed to administer chemotherapeutic agents to a single or localised group of vitreous seeds under indirect ophthalmoscopy. This is done instead of aiming the needle toward the center of the globe and spreading the agent(s) within the vitreous cavity. [1]
Intracameral Chemotherapy[edit | edit source]
Intracameral Chemotherapy (IcamC) was developed to administer a precise dosage of the pharmacological agent in the anterior chamber. [1]
Oral acetazolamide is given before the injection which helps to dampen aqueous humor secretion and prevent dilution of the agent. Aqueous humor is removed from the anterior and posterior chambers via a transcorneal method, using a specific needle. Prior to removal of the needle, a syringe exchange is used to deposit a similar volume of aqueous with melphalan or topotecan. Subsequent to the injection and upon removal of the needle, cryotherapy is used at the entrance of the anterior chamber. [1]
It was shown in one case that IcamC can also be used along with plaque radiotherapy, which resulted in maintenance of tumor control after 3 years follow‑up. [1]
Possible side effects can include, iris heterochromia and progressive cataract formation in the infected eye, which can be seen with stable corneal endothelial cell density after a 5‑years follow‑up. Use of topotecan may produce reduced adverse effects and could be as effective as melphalan. In these cases, a transcorneal approach with administration in the anterior chamber aqueous is carried out, and repeated on a monthly basis. [1]
Focal Therapies[edit | edit source]
These methods are used for tumor consolidation in addition to IVC or IAC. [1]
Focal therapies include cryotherapy and transpupillary thermotherapy (TTT). The use of these therapies results in some chorioretinal scarring, and also a reduced visual field or visual acuity if the lesions are managed inside the macula. [1]
With the involvement of both eyes, there should be consideration of alternative chemotherapy‑based intervention procedures for tumors involving the fovea. [1]
Cryotherapy[edit | edit source]
Cryotherapy is a reliable and frequently used treatment method. Indications include, management of small tumors and foci of sub retinal or preretinal seeds. Chemo-cryo is a modality that can be used which provides cryotherapy to the peripheral ora serrata, on the same day as IVC. This helps to improve the drug concentration. The method is carried out under direct ophthalmoscopy. [1]
Cryotherapy is generally used in conjunction with a type of chemotherapy, and not used on its own. It is generally used with IVC, and can be used with IAC. [1]
A major consequence after extensive use of cryotherapy can be exudative and rhegmatogenous retinal detachment. [1]
Transpupillary Thermotherapy[edit | edit source]
Transpupillary Thermotherapy (TTT) has become more prominent than laser photocoagulation for retinoblastoma intervention. Similar to cryotherapy, it can be used as an adjunct with chemotherapy for initial stages of treatment for small tumors which are under 3mm in diameter and 2 mm in thickness. TTT is also supplied via indirect ophthalmoscopy. There are various sessions administered over 4 week intervals. This helps produce a grey-white uptake, which would result in a flat scar or a calcified tumor. [1]
Consequences that are possible with TTT include, iris atrophy, anterior or posterior synechiae, and focal cataract. Consequences with an increased severity which may lead to loss of sight, but seldom occurs when the technique is properly carried out. This can include retinal vein occlusion, vitreous hemorrhage, retinal neovascularisation, vitreoretinal traction, and retinal detachment. [1]
External Beam Radiotherapy[edit | edit source]
External beam radiotherapy (EBRT) was used as globe salvage therapy before the use of IVC. Currently, EBRT is seldom used due to numerous side effects, and the many positive outcomes of efficacious chemotherapy treatments. However, EBRT is used in extraocular tumor extension, orbital recurrence, and positive optic nerve margin upon enucleation. [1]
With combining the use of EBRT and IVC for the management of orbital retinoblastoma, tumor control is effective in 71% of patients. [1]
Side effects from radiation with the use of ERBT include, [1]
- Tear deficiency,
- Dry eye syndrome,
- Filamentary,
- Keratopathy,
- Cataracts,
- Radiation retinopathy,
- Optic neuropathy, and
- Orbital growth retardation causing facial deformity.
The most critical side effects of EBRT are the future development of second primary tumors within the field of radiation. This is mainly a concern in patients with germline retinoblastoma. There is a risk of 53% by the age of 50, thus leading patients with germline mutation to die from the cause of secondary cancers than from retinoblastoma. [1]
The most frequently occurring second primary tumor is osteosarcoma, which can be followed by other bone tumors, soft tissue sarcoma, melanoma, and epithelial tumors, which can be bladder, breast, colorectal, kidney, lung, nasal cavity, prostate, retroperitoneum, thyroid, tongue, or uterus tumors. Because of the various side effects, it is recommended that EBRT be avoided if there are other available effective treatment methods. [1]
Plaque Radiotherapy[edit | edit source]
Plaque radiotherapy (brachytherapy) was primarily used as a globe salvage therapy for a recurring tumor occurring subsequent to EBRT. [1]
This is generally used as a secondary treatment for medium sized chemoresistant tumors (≤16 mm in largest basal diameter and 4-9 mm in thickness) with or without localised vitreous or subretinal seeding, following recurrence subsequent to IVC or IAC. This method is also carried out to manage diffuse anterior segment retinoblastoma with or without IVC, without the presence of choroidal or retinal tumors. [1]
Secondary plaque radiotherapy can be administered 1‑2 months subsequent to IVC to help decrease side effects. [1]
This therapy takes 2-4 days to fully administer the dose, as opposed to EBRT. Many serious side effects are prevented with plaque radiotherapy, in comparison to EBRT. This would include ipsilateral orbit, and facial hypoplasia, as well as recurring or secondary cancers. [1]
The efficacy of plaque radiotherapy as a secondary treatment subsequent to IAC is 79%, especially with the presence of localszed vitreous seeding. [1]
Even though there is a high efficacy of plaque radiotherapy, there are possible side effects of the treatment. These side effects can include: [1]
- Cataracts (20‑43%),
- Radiation maculopathy (25%),
- Radiation papillopathy (26%), and
- Vitreous hemorrhage (54%).
There is a higher incidence of radiation retinopathy of 40% and cataract formation of 43% with secondary plaque radiotherapy, as opposed to with primary plaque radiotherapy, at 27% and 33%, respectively.
Enucleation[edit | edit source]
Enucleation is a historically used method for the treatment of retinoblastoma, as there have been many advances in treatment methods. However, it is used due to poor tumor visualisation (from vitreous hemorrhage), indication of extraocular extensions, optic nerve or choroid possibly being invaded, or recalcitrant tumors that have developed where previous globe salvage therapies has not been effective (IAC, IvitC, plaque radiotherapy, etc). [1]
Side effects of this treatment include, [1]
- Chemosis,
- Conjunctival cysts,
- Pyogenic granuloma,
- Blepharoptosis,
- Lagophthalmos,
- Superior sulcus defect,
- Enophthalmos,
- Symblepharon,
- Implant exposure, and
- Infection.
Urgent wound care and repair would be required for orbital implant exposures. Infections can be treated topically or systemically using antibiotics. The removal of implants can be necessary in critical infectious conditions. If there is continuous contact of the prosthesis followed by giant papillary conjunctivitis, this can be treated with antibiotic‑steroid creams and an extensive use of lubricants. [1]
With the removal of the eye, there can be functional, physical, and psychological effects that occur. Prosthetic rehabilitation is important for the individual. Having cosmetic rehabilitation carried out after the enucleation is recommended for the first 6 weeks. When there are reduced risks for dehiscence, bleeding or infection, molds are created for a custom ocular prosthesis. An early prosthesis insertion is also shown to increase the individual's quality of life. [1]
Ongoing Evaluation and Assessment[edit | edit source]
These steps should be performed before diagnosis and continuously after initial diagnosis as a means of reassessment. [1]
The extent of the tumor inside and outside of the eye should be determined. The stage of cancer or tumor should also be determined for each eye depending on the intensity of the cancer spreading outside the eye, which can be predicted using ultrasound or MRI, and noting the tumor-nerve optic nerve relationship. CT examination is however not recommended due to the additional exposure to radiation therapy. [1]
If there is a presence of very large tumor(s) with a possibility of an extraocular disease, it is recommended that bone marrow aspiration and analysis of cerebrospinal fluid can be carried out at diagnosis. This can also be carried out when pathologic examination of the enucleated eye presents optic nerve intrusion with a likelihood for spreading outside the eye. If it spreads outside the eye, the most suitable care would need to be determined. [1]
It is possible that the the retinal tumors can be small and noticed by optical coherent tomography in those with a family history of retinoblastoma, and if the child displays strabismus or poor vision. [1]
Families speaking with health professionals such as a medical geneticist, certified genetic counselor, or certified advanced genetic nurse to gather information on the nature, inheritance, and complications of retinoblastoma, can assist with medical and personal decision making. [1]
Long-term Monitoring of the Cancer-free Patient[edit | edit source]
The patient is generally followed up every 4 weeks, to evaluate the treatment, check for any side effects, and determine future management steps. Generally globe salvage treatment would be continued, with maintaining observation and analysis, but there are also cases where enucleation may be necessary. [1]
Thereafter, the patients should be monitored for life, especially if the condition has occurred through genetic transmission. It is possible that a secondary or second cancer may occur, regardless of the treatment stage of the initial retinoblastoma.
Once tumor control has been maintained, patients are monitored with eye exams on a periodic basis until the age of 7, and then monitored less frequently. It is seen that many patients experience a recurrence around 3 years after treatment, and remain free of recurrences subsequent to that. It is possible that a recurrence can develop 11 years after the primary treatment. Reassessment visits with the pediatric oncologist are recommended every 1-2 years. [1]
Visits to the ophthalmologist need to be centred around assessing for long‑term secondary effects of the cancer treatment (amblyopia, glaucoma, cataract, vitreous hemorrhage, retinal detachment, etc.), maintaining the health of the unaffected eye, and any age related care and visual acuity assessment. [1]
Patients and families should be educated on any genetic effects and how this may effect further family planning and lines of genetic transmission. [1]
Resources[edit | edit source]
Retinoblastoma in Children from the Children's Cancer and Leukemia Group
Stages of Retinoblastoma from the Canadian Cancer Society
Treating Retinoblastoma from the American Cancer Society
Looking at Retinoblastoma Through the Lens of Global Health
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 1.38 1.39 1.40 1.41 1.42 1.43 1.44 1.45 1.46 1.47 1.48 1.49 1.50 1.51 1.52 1.53 1.54 1.55 1.56 1.57 1.58 1.59 1.60 1.61 1.62 1.63 1.64 1.65 1.66 1.67 1.68 1.69 1.70 1.71 1.72 Lohmann D.R, Gallie B.L. Retinoblastoma. GENEReviews. 2023:1-22.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 Ancona-Lezama D, Dalvin LA, Shields CL. Modern treatment of retinoblastoma: A 2020 review. Indian Journal of Ophthalmology. 2020:68:2356-2365.