Pneumorrhachis
Introduction[edit | edit source]
Pneumorrhachis also known as Epidural emphysema is a rare condition characterized by intraspinal air or air in the epidural space as a result of traumatic, iatrogenic factors from surgery, anesthesia and diagnostic interventions or as a result of increased intrathoracic pressure associated with forced coughing from conditions such as bronchial asthma.[1][2] Pneumorrhachis can be classified into epidural or subarachnoid depending on the location of the air in the spinal canal.[3]
Aetiology[edit | edit source]
The causes of pneumorrhachasis is classified into iatrogenic, non-traumatic, or traumatic although traumatic cases are rare and traumatic pneumorrhachasis is usually associated with air in the subarachnoid space and is an indicator of severe injury.[3] Cases of Traumatic Pnuemorrhachasis are often associated with neurological deficits and a few cases are as a result of stab injuries to the lower cervical spine.[4]
Pathogenesis[edit | edit source]
The increase in the pressure between the alveoli and interstitial space which occurs during coughing can cause alveolar rupture, followed by air dissection along the bronchoalveolar sheaths and into the mediastinum. Air then passes through the path of least resistance into the mediastinum into the fascial planes of the neck. The lack of fascia barriers between the posterior mediastinum and the epidural space permits air to escape through the neural canal into the epidural space.[5]
Epidermiology[edit | edit source]
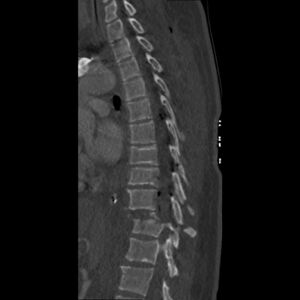
Several cases are reported on the various presentations f the condition as it occurs in children in the case of 2 children having Pneumorrachasis as a result of pnuemomediastinum[7] and also adults. The was a case of a 62 years old patient presenting with degenerative changes in the lumbar spine, including end plates and disc spaces, with intervertebral disc vacuum phenomenon (VP) with the CT showing intraspinal air in the epidural space at L5-S1 levels which compresses on the cauda eqina[8] causing neurological symptoms.[9] Pneumorrhachis was present in 5.8% of patients presenting with pneumomediastinum.[10] This condition is also common in patients with forceful vomiting.[11] [12][13]
Clinical Presentations[edit | edit source]
This condition is often asymptomatic[14], although rarely it presents with symptoms such as pain, discomfort, neurological symptoms such as progressive muscle weakness as air in the spinal canal increases the pressure in the spinal cord and compresses the spinal cord[15] Therefore, traumatic pneumorrhachis could be a possible cause of traumatic spinal cord compression[16]. Some of these patients have co-morbidity such as Bronchial asthma and pnuemothorax[17]. Air injected also can act as a space-occupying lesion and exert pressure on nervous structures within the spinal canal[18]
Differential Diagnosis[edit | edit source]
- Tension pneumothorax
- Thoracic spinal fracture
- Pneumocephalus.[19]
Diagnosis[edit | edit source]
Radiological investigations such as MRI and X-ray are used primarily for the diagnoses as intraspinal air is usually asymptomatic and clinically unspecific.[20] Traumatic PR, especially subarachnoid, is an indicator of severe injury which is usually notable on the CT and therefore, CT scan is highly recommended in the diagnoses of PR.[21]
Management[edit | edit source]
Medical and Surgical Management[edit | edit source]
Pnuemorrhachis which is spontaneous, asymptomatic and usually resolves it self therefore the management is usually conservative for this type of Pnuemorrhachis.[20][22] Pnuemorrhachis is individualized and frequently requires multidisciplinary management, involving head, chest, and/or abdomen interventions depending on the presentations of the patient[23]. Medical treatment approaches include the use of intravenous steroids (dexamethasone), administration of high concentrations of inspired oxygen to promote re-absorption of air, and hyperbaric oxygen therapy.[17] The surgical management of this condition is dependent of the presentation as patients with pneumorrhachis have different presentations depending on the cause of pneunorrhachis. A case of reversible spinal cord and lower cervical root dysfunction caused by air dissection through a bronchopleural-epidural-cutaneous fistula[24]
Physiotherapy Management[edit | edit source]
The role of physiotherapy in the management of pnuemorrhachis is dependent on symptoms and co-morbidity as each case presents with various causes. These include;
- To clear Airways
- Ensure proper breathing patterns
- Improve muscular strength
- Restore the patient to independent function concerning the symptoms presented
- Manage comorbidities and presentations such as Cancer, reduced respiratory function and asthma.
References[edit | edit source]
- ↑ Kirkham J, Schiers KA. Pneumorrhachis. J Am Osteopath Assoc. 2016 Feb;116(2):119. doi: 10.7556/jaoa.2016.027. PMID: 26830529.
- ↑ Manden PK, Siddiqui AH. Pneumorrhachis, pneumomediastinum, pneumopericardium and subcutaneous emphysema as complications of bronchial asthma. Ann Thorac Med. 2009 Jul;4(3):143-5. doi: 10.4103/1817-1737.53352. PMID: 19641647; PMCID: PMC2714570.
- ↑ 3.0 3.1 Gelalis ID, Karageorgos A, Arnaoutoglou C, Gartzonikas D, Politis A, Georgakopoulos N, Petsanas AP, Matzaroglou C, Xenakis T. Traumatic pneumorrhachis: etiology, pathomechanism, diagnosis, and treatment. Spine J. 2011 Feb;11(2):153-7. doi: 10.1016/j.spinee.2010.12.010. PMID: 21296300.https://pubmed.ncbi.nlm.nih.gov/21296300/
- ↑ Traumatic pneumorrhachis: 2 cases and review of the literature Hasan Kara, Murat Akinci et al. The American Journal of Emergency Medicine, 33, 6, 6 2015. https://www.sciencedirect.com/science/article/abs/pii/S0735675714009425
- ↑ Pathophysiology of epidural pneumorrhachis. | Download Scientific Diagram https://www.researchgate.net/figure/Pathophysiology-of-epidural-pneumorrhachis_fig3_263208566.
- ↑ Case courtesy of Liz Silverstone, <a href="https://radiopaedia.org/?lang=us">Radiopaedia.org</a>. From the case <a href="https://radiopaedia.org/cases/91306?lang=us">rID: 91306</a> https://radiopaedia.org/articles/pneumorrhachis
- ↑ Yaginuma K, Watanabe M, Saito Y, Takahashi N, Ohara Y, Kobayashi S, Mochizuki K, Suyama K, Sato M, Sano H, Hashimoto K, Kikuta A, Hosoya M. Pneumorrhachis in children: A report of two cases and review of the literature. Radiol Case Rep. 2019 Sep 5;14(11):1325-1329. doi: 10.1016/j.radcr.2019.08.010. PMID: 31516647; PMCID: PMC6732755. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6732755/
- ↑ Cauda Equina. (2022, April 29). Physiopedia, . Retrieved 22:23, April 25, 2023 from https://www.physio-pedia.com/index.php?title=Cauda_Equina&oldid=303384.
- ↑ Pneumorrhachis causing cauda equina syndrome: a case report and literature review Areez Shafqat, Hamzah M.F. Magableh et al. Egyptian Journal of Radiology and Nuclear Medicine, 51, 1, 12 2020
- ↑ Behr G, Mema E, Costa K, Garg A. Proportion and Clinical Relevance of Intraspinal Air in Patients With Pneumomediastinum. AJR Am J Roentgenol. 2018 Aug;211(2):321-326. doi: 10.2214/AJR.17.19256. Epub 2018 May 29. PMID: 29812979; PMCID: PMC7956126.
- ↑ Gill I, Edhi AI, Cappell MS. Proposed characterization of the syndrome of epidural pneumatosis (pneumorrhachis) in patients with forceful vomiting from diabetic ketoacidosis as a clinico-radiologic pentad based on systematic literature review & an illustrative case report. Medicine (Baltimore). 2020 Aug 28;99(35):e21001. doi: 10.1097/MD.0000000000021001. PMID: 32871860; PMCID: PMC7458230. https://pubmed.ncbi.nlm.nih.gov/32871860/
- ↑ Hudson JS, Jeong S, Zhang X, Abel TJ. Spontaneous epidural pneumorrhachis in 14 years old. Surg Neurol Int. 2021 Jul 6;12:329. doi: 10.25259/SNI_414_2021. Erratum in: Surg Neurol Int. 2021 Aug 14;12:404. PMID: 34345470; PMCID: PMC8326144. https://pubmed.ncbi.nlm.nih.gov/34345470/
- ↑ Houston R, Fiani B, Musch B, Tayag E. Holocord spontaneous pneumorrhachis in the setting of refractory emesis. Surg Neurol Int. 2021 Dec 8;12:602. doi: 10.25259/SNI_1046_2021. PMID: 34992919; PMCID: PMC8720439. https://pubmed.ncbi.nlm.nih.gov/34992919/
- ↑ Kim SW, Seo HJ. Symptomatic epidural pneumorrhachis : a rare entity. J Korean Neurosurg Soc. 2013 Jul;54(1):65-7. doi: 10.3340/jkns.2013.54.1.65. Epub 2013 Jul 31. PMID: 24044086; PMCID: PMC3772292. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3772292/
- ↑ Uemura K, Behr R, Roosen K. Symptomatic intraspinal air entrapment. Br J Neurosurg. 2000 Apr;14(2):154-6. doi: 10.1080/02688690050004642. PMID: 10889894. https://pubmed.ncbi.nlm.nih.gov/10889894/
- ↑ Pneumorachis: A possible source of traumatic cord compression. M. Ould-Slimane, M. A. Ettori et al. Orthopaedics & Traumatology: Surgery & Research, 96, 7, 11 2010
- ↑ 17.0 17.1 The Spine. Fred Nelson, Carolyn Blauvelt. A Manual of Orthopaedic Terminology, 2022. https://www.sciencedirect.com/topics/medicine-and-dentistry/pneumorachis
- ↑ Boezaart AP, Levendig BJ. Epidural air-filled bubbles and unblocked segments. Can J Anaesth. 1989 Sep;36(5):603-4. doi: 10.1007/BF03005401. PMID: 2791185. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1602196/#CR29
- ↑ Ghafarzad A, Tagizadieh A, Moharamzadeh P, Shahsavari Nia K, Majidi G. Thoracic Pneumorrhachis in Patient with Lumbar Fractures; a Case Report. Emerg (Tehran). 2014 Spring;2(2):98-100. PMID: 26495356; PMCID: PMC4614588. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4614588/
- ↑ 20.0 20.1 Oertel MF, Korinth MC, Reinges MH, Krings T, Terbeck S, Gilsbach JM. Pathogenesis, diagnosis and management of pneumorrhachis. Eur Spine J. 2006 Oct;15 Suppl 5(Suppl 5):636-43. doi: 10.1007/s00586-006-0160-6. Epub 2006 Jul 12. PMID: 16835735; PMCID: PMC1602196. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1602196/
- ↑ Traumatic pneumorrhachis: etiology, pathomechanism, diagnosis, and treatment. Ioannis D. Gelalis, Athanasios Karageorgos et al.The Spine Journal, 11, 2, 2 2011. https://sci-hub.se/https://doi.org/10.1016/j.spinee.2010.12.010
- ↑ Gelalis ID, Karageorgos A, Arnaoutoglou C, Gartzonikas D, Politis A, Georgakopoulos N, Petsanas AP, Matzaroglou C, Xenakis T. Traumatic pneumorrhachis: etiology, pathomechanism, diagnosis, and treatment. Spine J. 2011 Feb;11(2):153-7. doi: 10.1016/j.spinee.2010.12.010. PMID: 21296300.
- ↑ Gelalis ID, Karageorgos A, Arnaoutoglou C, Gartzonikas D, Politis A, Georgakopoulos N, Petsanas AP, Matzaroglou C, Xenakis T. Traumatic pneumorrhachis: etiology, pathomechanism, diagnosis, and treatment. Spine J. 2011 Feb;11(2):153-7. doi: 10.1016/j.spinee.2010.12.010. PMID: 21296300. https://pubmed.ncbi.nlm.nih.gov/21296300/
- ↑ Gonzales GR, Payne R, Portenoy RK, Foley KM. Epidural air from a bronchopleural-epidural-cutaneous fistula producing reversible myelopathy and radiculopathy symptoms. Neurology. 1994 Dec;44(12):2409-10. doi: 10.1212/wnl.44.12.2409. PMID: 7991142. https://pubmed.ncbi.nlm.nih.gov/7991142/