Vestibular Oculomotor Motor Screening (VOMS) Assessment: Difference between revisions
Kim Jackson (talk | contribs) m (Text replacement - "Category:Course Pages" to "Category:Course Pages Category:Physioplus Content") |
No edit summary |
||
| (8 intermediate revisions by 4 users not shown) | |||
| Line 5: | Line 5: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
The VOMS assessment is a tool designed to identify the signs and symptoms of a concussion. According to the creators of the VOMS assessment: <ref>UPMC Sports Medicine. Vestibular Ocular Motor Screening (VOMS). Available from: https://www.upmc.com/services/sports-medicine/services/concussion/symptoms-diagnosis/voms (accessed 16/11/2022).</ref> | |||
[[Concussion]]<nowiki/>s can directly impair oculomotor function. Ocular issues (poor eye tracking) after concussion are common. Specifically cranial nerves (CN) III, IV and VI which innervate the eye muscles are susceptible to injury anywhere along the route from brainstem to eye muscles, so this needs to be assessed. | * Symptoms which include vision issues, fogginess, and dizziness are often associated with prolonged recovery after concussion | ||
* Assessment of the vestibular ocular system provides the most accurate predictions of long-term outcomes from sports-related concussions | |||
<blockquote> | |||
"Individuals who have suffered a concussion/mild traumatic brain injury (mTBI) frequently report symptoms associated with vestibular and/or oculomotor dysfunction (VOD) like dizziness, nausea, fatigue, brain fog, headache, gait and neurocognitive impairments which are associated with the development of chronic symptoms. The Vestibular/Ocular Motor Screening (VOMS) tool has been established as a reliable and clinically relevant complement to use alongside a battery of post-concussion tests to improve screening and referral for further evaluation and treatment of VOD." | |||
-Kaae C et al 2022.<ref name=":4">Kaae C, Cadigan K, Lai K, Theis J. [https://content.iospress.com/articles/neurorehabilitation/nre228012 Vestibulo-ocular dysfunction in mTBI: Utility of the VOMS for evaluation and management–A review]. NeuroRehabilitation. 2022 Jan 1;50(3):279-96.</ref></blockquote> | |||
Impairments in the vestibulo-ocular system commonly manifest as symptoms of dizziness and visual instability. Nearly 30% of concussed athletes report visual problems during the first week after the injury.<ref name=":0">Kontos AP, Elbin RJ, Schatz P, et al. [https://www.ncbi.nlm.nih.gov/pubmed/22904209 A revised factor structure for the Post-Concussion Symptom Scale: baseline and postconcussion factors]. Am J Sports Med. 2012;40(10):2375-2384.</ref> Oculomotor impairments and symptoms may manifest as blurred vision, diplopia, impaired eye movements, difficulty in reading, dizziness, [[Headaches and Dizziness|headaches]], ocular pain, and poor visual-based concentration.<ref>Ciuffreda KJ, Ludlam D, Thiagarajan P. [https://www.ncbi.nlm.nih.gov/pubmed/21276567 Oculomotor diagnostic protocol for the mTBI population.] Optometry. 2011;82(2):61-63.</ref> Dizziness, which may represent an underlying impairment of the vestibular and/or oculomotor systems, is reported by 50% of concussed athletes<ref name=":0" /> and is associated with a 6.4-times greater risk, relative to any other on-field symptom, in predicting protracted (>21 days) recovery.<ref>Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. [https://journals.sagepub.com/doi/abs/10.1177/0363546511410655 Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players?] Am J Sports Med. 2011;39(11):2311-2318.</ref> | |||
[[Assessment and Management of Concussion|Assessment and management of concussion]]<nowiki/>s can directly impair oculomotor function. Ocular issues (poor eye tracking) after concussion are common. Specifically cranial nerves (CN) III, IV and VI which innervate the eye muscles are susceptible to injury anywhere along the route from brainstem to eye muscles, so this needs to be assessed. | |||
== Objective == | == Objective == | ||
The Vestibular/Ocular Motor Screening (VOMS) Assessment is | The Vestibular/Ocular Motor Screening (VOMS) Assessment is a brief 5-10 minute concussion screening tool. It has been proposed that it may serve as a single component of a comprehensive approach to the assessment of concussions.<ref name=":1">Mucha A, Collins MW, Elbin RJ, Furman JM, Troutman-Enseki C, DeWolf RM, Marchetti G, Kontos AP. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4209316/ A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions: preliminary finding]s. The American journal of sports medicine. 2014 Oct;42(10):2479-86.</ref><ref>Yorke AM, Smith L, Babcock M, Alsalaheen B. Validity and Reliability of the Vestibular/Ocular Motor Screening and Associations With Common Concussion Screening Tools. Sports Health. 2017;9(2):174-80. </ref> More recent evidence is suggesting that the VOMS, when used in a combination with other assessment tools, can aide in outcome prediction for individuals following a concussion or mild traumatic brain injury (mTBI).<ref>Knell G, Caze T, Burkhart SO. [https://scholar.google.com/scholar?output=instlink&q=info:66FLAaJTdnUJ:scholar.google.com/&hl=en&as_sdt=0,44&as_ylo=2021&scillfp=3377324037247749458&oi=lle Evaluation of the vestibular and ocular motor screening (VOMS) as a prognostic tool for protracted recovery following paediatric sports-related concussion]. BMJ Open Sport & Exercise Medicine. 2021 Mar 1;7(1):e000970.</ref><ref name=":3">Kaae C, Cadigan K, Lai K, Theis J. [https://content.iospress.com/articles/neurorehabilitation/nre228012 Vestibulo-ocular dysfunction in mTBI: Utility of the VOMS for evaluation and management]. A review. NeuroRehabilitation. 2022 Jan 1(Preprint):1-8.</ref><ref>Parrington L, King LA, Hoppes CW, Klaiman MJ, Michielutti P, Fino PC, Dibble LE, Lester ME, Weightman MM. [https://journals.lww.com/headtraumarehab/Fulltext/2022/09000/Exploring_Vestibular_Ocular_Motor_Screening_in.13.aspx Exploring vestibular ocular motor screening in adults with persistent complaints after mild traumatic brain injury]. Journal of head trauma rehabilitation. 2022 Sep 23;37(5):E346-54.</ref><blockquote>"Eye movement abnormalities can be an objective biomarker for assessing concussion, as eye movement control relates to neurological functional integrity. Over the past few years, numerous government and medical organizations have released consensus recommendations that include performing vestibulo-oculomotor testing when diagnosing concussion." | ||
-Kaae C et al 2022.<ref name=":4" /></blockquote>The VOMS assessment is established as a reliable and clinically relevant assessment tool, that when used appropriately can improve screening and referral for further evaluation and treatment of vestibular and/or oculomotor dysfunction following a mTBI.<ref name=":3" /> | |||
== Intended population == | == Intended population == | ||
| Line 25: | Line 37: | ||
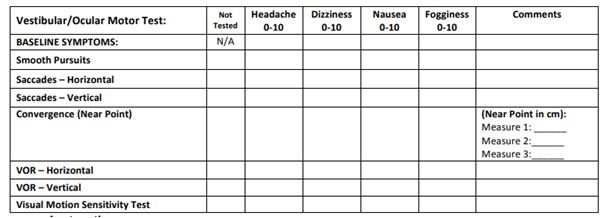
Prior to performing the 5 domains of the VOMS screen, it is important to establish the patient's baseline symptoms. On a scale of 0-10, ask the patient to score their symptoms at rest for headache, dizziness, nausea & fogginess. | Prior to performing the 5 domains of the VOMS screen, it is important to establish the patient's baseline symptoms. On a scale of 0-10, ask the patient to score their symptoms at rest for headache, dizziness, nausea & fogginess. | ||
For each Domain, symptom provocation should be considered a positive result.<ref>Crampton A, Schneider KJ, Grilli L, Chevignard M, Katz-Leurer M, Beauchamp MH, Debert C, Gagnon IJ. [https://www.sciencedirect.com/science/article/pii/S2590109522000453 Determining the Agreement Between Common Measures Related to Vestibulo-ocular Reflex Function After a Mild Traumatic Brain Injury in Children and Adolescents]. Archives of Rehabilitation Research and Clinical Translation. 2022 Sep 1;4(3):100217.</ref> Symptoms provocation can include, but not limited to: headache, dizziness, nausea and mental fogginess. | |||
=== Domain 1: Smooth Pursuit === | === Domain 1: Smooth Pursuit === | ||
[[File:Vertical_Saccades.JPG| | <blockquote>"'''Smooth pursuit''' eye movements are a type of conjugate eye movement that primarily allows both eyes to simultaneously follow a slow-moving target and maintain that image on the retina as the target moves. Smooth pursuits also work with the VOR to help maintain fixation on a target when the head and body is in motion. When smooth pursuits are impaired, the eyes will lose track of the moving object and use a saccadic eye-movement to recover or “catch up” to the target, making abnormal smooth pursuits look jerky on clinical examination." -Kaae C et al 2022.<ref name=":4" /> </blockquote>[[File:Vertical_Saccades.JPG|thumb|Smooth Pursuit Test]] | ||
This tests the ability to follow a slowly moving target. The patient and the examiner are seated. The examiner holds a fingertip at a distance of 3 ft. from the patient. The patient is instructed to maintain focus on the target as the examiner moves the target smoothly in the horizontal direction 1.5 ft. to the right and 1.5 ft. to the left of midline. One repetition is complete when the target moves back and forth to the starting position, and 2 repetitions are performed. The target should be moved at a rate requiring approximately 2 seconds to go fully from left to right and 2 seconds to go fully from right to left. The test is repeated with the examiner moving the target smoothly and slowly in the vertical direction 1.5 ft. above and 1.5 ft. below midline for 2 complete repetitions up and down. Again, the target should be moved at a rate requiring approximately 2 seconds to move the eyes fully upward and 2 seconds to move fully downward. | This tests the ability to follow a slowly moving target. The patient and the examiner are seated. The examiner holds a fingertip at a distance of 3 ft. from the patient. The patient is instructed to maintain focus on the target as the examiner moves the target smoothly in the horizontal direction 1.5 ft. to the right and 1.5 ft. to the left of midline. One repetition is complete when the target moves back and forth to the starting position, and 2 repetitions are performed. The target should be moved at a rate requiring approximately 2 seconds to go fully from left to right and 2 seconds to go fully from right to left. The test is repeated with the examiner moving the target smoothly and slowly in the vertical direction 1.5 ft. above and 1.5 ft. below midline for 2 complete repetitions up and down. Again, the target should be moved at a rate requiring approximately 2 seconds to move the eyes fully upward and 2 seconds to move fully downward. | ||
| Line 33: | Line 45: | ||
=== Domain 2: Saccades === | === Domain 2: Saccades === | ||
<blockquote>"'''Saccadic''' eye movements are a conjugate eye movement that allow both eyes to move quickly in the same direction, rapidly shifting the eyes from one object of visual interest to another. Saccades can be made voluntarily or reflexively to visual, auditory, memory, and tactile stimuli. Clinically, when saccades are inaccurate in mTBI, they have been characterized as hypometric (undershoot the target) or hypermetric (overshoot the target), have slower velocities/increased latency, and smaller peak accelerations." -Kaae C et al 2022.<ref name=":4" /> </blockquote> | |||
This tests the ability of the eyes to move quickly between targets. The patient and the examiner are seated. [[File:Horizontal_Saccades.JPG|thumb|Saccaddes Test]] | |||
* '''Horizontal Saccades''': The examiner holds two single points (fingertips) horizontally at a distance of 3 ft. from the patient, and 1.5 ft. to the right and 1.5 ft. to the left of midline so that the patient must gaze 30 degrees to left and 30 degrees to the right. Instruct the patient to move their eyes as quickly as possible from point to point. One repetition is complete when the eyes move back and forth to the starting position, and 10 repetitions are performed. | * '''Horizontal Saccades''': The examiner holds two single points (fingertips) horizontally at a distance of 3 ft. from the patient, and 1.5 ft. to the right and 1.5 ft. to the left of midline so that the patient must gaze 30 degrees to left and 30 degrees to the right. Instruct the patient to move their eyes as quickly as possible from point to point. One repetition is complete when the eyes move back and forth to the starting position, and 10 repetitions are performed. | ||
''Record: Headache, Dizziness, Nausea & Fogginess ratings after the test.'' | ''Record: Headache, Dizziness, Nausea & Fogginess ratings after the test.'' | ||
| Line 43: | Line 55: | ||
=== Domain 3: Convergence === | === Domain 3: Convergence === | ||
[[File:Convergence.JPG| | <blockquote>"Vergence eye movements are a disconjugate eye movement used to track an object moving closer or further away as well as look at objects that are located at different distances away. When looking at objects further away, both eyes move outwards, termed divergence. When looking at objects approaching closer, both eyes move inwards towards the nose, termed '''convergence'''. Both eyes need to make these movements at the same speed and magnitude in order for the brain to interpret a single and fused image perception (binocular vision). If the eyes do not move together in sync, the brain will either perceive two distinct images (ie double vision) due to the mismatched input from each eye, or the brain will perceive an overlap of images, which may be perceived as blurry vision or shadowing." -Kaae C et al 2022.<ref name=":4" /></blockquote>[[File:Convergence.JPG|thumb|Convergence Test]] | ||
Convergence is assessed by both symptom report and objective measurement of the near point of convergence (NPC).The NPC values are averaged across 3 trials, and normal NPC values are within 5 cm.<ref>Scheiman M, Gallaway M, Frantz KA, et al. [http://hope.vision/wp-content/uploads/nearpoint_of_convergence__test_procedure_target-11.pdf Nearpoint of convergence: test procedure, target selection, and normative data.] Optom Vis Sci80(3) 2003:214-225</ref> | Convergence is assessed by both symptom report and objective measurement of the near point of convergence (NPC).The NPC values are averaged across 3 trials, and normal NPC values are within 5 cm.<ref>Scheiman M, Gallaway M, Frantz KA, et al. [http://hope.vision/wp-content/uploads/nearpoint_of_convergence__test_procedure_target-11.pdf Nearpoint of convergence: test procedure, target selection, and normative data.] Optom Vis Sci80(3) 2003:214-225</ref> | ||
| Line 51: | Line 63: | ||
=== Domain 4: Vestibular-Ocular Reflex (VOR) Test === | === Domain 4: Vestibular-Ocular Reflex (VOR) Test === | ||
[[File:Vertical_VOR_Test.JPG| | [[File:Vertical_VOR_Test.JPG|thumb|Vestibular-Ocular Reflex (VOR) Test]] | ||
Assess the ability to stabilise vision as the head moves. The patient and the examiner are seated. The examiner holds a target of approximately 14 point font size in front of the patient in the midline at a distance of 3 ft. | Assess the ability to stabilise vision as the head moves. The patient and the examiner are seated. The examiner holds a target of approximately 14 point font size in front of the patient in the midline at a distance of 3 ft. | ||
| Line 63: | Line 75: | ||
=== Domain 5: Visual Motion Sensitivity (VMS) Test === | === Domain 5: Visual Motion Sensitivity (VMS) Test === | ||
[[File:Visual_Motion_Sensitivity_(VMS)_Test.JPG| | Also known as VOR cancellation test.[[File:Visual_Motion_Sensitivity_(VMS)_Test.JPG|thumb|Visual Motional Sensitivity (VMS) Test]] | ||
Assess visual motion sensitivity and the ability to inhibit vestibular-induced eye movements using vision. | Assess visual motion sensitivity and the ability to inhibit vestibular-induced eye movements using vision. | ||
| Line 81: | Line 93: | ||
Anzalon et al<ref>Anzalone AJ, Blueitt D, Case T, McGuffin T, Pollard K, Garrison JC, Jones MT, Pavur R, Turner S, Oliver JM. [https://www.ncbi.nlm.nih.gov/pubmed/27789472 A positive vestibular/ocular motor screening (VOMS) is associated with increased recovery time after sports-related concussion in youth and adolescent athletes. The American journal of sports medicine.] 2017 Feb;45(2):474-9.</ref> suggest that the VOMS can serve as a predictor of recovery time in patients with sports-related concussion. | Anzalon et al<ref>Anzalone AJ, Blueitt D, Case T, McGuffin T, Pollard K, Garrison JC, Jones MT, Pavur R, Turner S, Oliver JM. [https://www.ncbi.nlm.nih.gov/pubmed/27789472 A positive vestibular/ocular motor screening (VOMS) is associated with increased recovery time after sports-related concussion in youth and adolescent athletes. The American journal of sports medicine.] 2017 Feb;45(2):474-9.</ref> suggest that the VOMS can serve as a predictor of recovery time in patients with sports-related concussion. | ||
Worts et al<ref>Worts PR, Schatz P, Burkhart SO. Test Performance and Test-Retest Reliability of the Vestibular/Ocular Motor Screening and King-Devick Test in Adolescent Athletes During a Competitive Sport Season. Am J Sports Med. 2018;46(8):2004-10. </ref> found that the VOMS may be more stable than other screening measures and is less likely to result in false-positives than the King-Devick test in adolescent athletes. {{#ev:youtube|IsixgD-2LQE}} | Worts et al<ref>Worts PR, Schatz P, Burkhart SO. Test Performance and Test-Retest Reliability of the Vestibular/Ocular Motor Screening and King-Devick Test in Adolescent Athletes During a Competitive Sport Season. Am J Sports Med. 2018;46(8):2004-10. </ref> found that the VOMS may be more stable than other screening measures and is less likely to result in false-positives than the King-Devick test in adolescent athletes. | ||
Please view the following six-minute video for a quick demonstration of the VOMS. Please note how this professional discusses the importance of using this examination as part of a concussion assessment.{{#ev:youtube|IsixgD-2LQE}} | |||
== References == | == References == | ||
| Line 91: | Line 105: | ||
[[Category:Head - Assessment and Examination]] | [[Category:Head - Assessment and Examination]] | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category: | [[Category:Plus Content]] | ||
[[Category:Outcome Measures]] | [[Category:Outcome Measures]] | ||
Latest revision as of 04:28, 31 October 2023
Original Editor - Megyn Robertson
Top Contributors - Simisola Ajeyalemi, Kim Jackson, Rachael Lowe, Shaimaa Eldib, Mandy Roscher, Stacy Schiurring, Megyn Robertson, Samuel Adedigba, Jess Bell, Olajumoke Ogunleye and Nupur Smit Shah
Introduction[edit | edit source]
The VOMS assessment is a tool designed to identify the signs and symptoms of a concussion. According to the creators of the VOMS assessment: [1]
- Symptoms which include vision issues, fogginess, and dizziness are often associated with prolonged recovery after concussion
- Assessment of the vestibular ocular system provides the most accurate predictions of long-term outcomes from sports-related concussions
"Individuals who have suffered a concussion/mild traumatic brain injury (mTBI) frequently report symptoms associated with vestibular and/or oculomotor dysfunction (VOD) like dizziness, nausea, fatigue, brain fog, headache, gait and neurocognitive impairments which are associated with the development of chronic symptoms. The Vestibular/Ocular Motor Screening (VOMS) tool has been established as a reliable and clinically relevant complement to use alongside a battery of post-concussion tests to improve screening and referral for further evaluation and treatment of VOD."-Kaae C et al 2022.[2]
Impairments in the vestibulo-ocular system commonly manifest as symptoms of dizziness and visual instability. Nearly 30% of concussed athletes report visual problems during the first week after the injury.[3] Oculomotor impairments and symptoms may manifest as blurred vision, diplopia, impaired eye movements, difficulty in reading, dizziness, headaches, ocular pain, and poor visual-based concentration.[4] Dizziness, which may represent an underlying impairment of the vestibular and/or oculomotor systems, is reported by 50% of concussed athletes[3] and is associated with a 6.4-times greater risk, relative to any other on-field symptom, in predicting protracted (>21 days) recovery.[5]
Assessment and management of concussions can directly impair oculomotor function. Ocular issues (poor eye tracking) after concussion are common. Specifically cranial nerves (CN) III, IV and VI which innervate the eye muscles are susceptible to injury anywhere along the route from brainstem to eye muscles, so this needs to be assessed.
Objective[edit | edit source]
The Vestibular/Ocular Motor Screening (VOMS) Assessment is a brief 5-10 minute concussion screening tool. It has been proposed that it may serve as a single component of a comprehensive approach to the assessment of concussions.[6][7] More recent evidence is suggesting that the VOMS, when used in a combination with other assessment tools, can aide in outcome prediction for individuals following a concussion or mild traumatic brain injury (mTBI).[8][9][10]
"Eye movement abnormalities can be an objective biomarker for assessing concussion, as eye movement control relates to neurological functional integrity. Over the past few years, numerous government and medical organizations have released consensus recommendations that include performing vestibulo-oculomotor testing when diagnosing concussion." -Kaae C et al 2022.[2]
The VOMS assessment is established as a reliable and clinically relevant assessment tool, that when used appropriately can improve screening and referral for further evaluation and treatment of vestibular and/or oculomotor dysfunction following a mTBI.[9]
Intended population[edit | edit source]
The test is designed for use with subjects ages 9-40, when used with patients outside this age range, interpretation may vary.
Method of Use[edit | edit source]
For this test you will need: a tape measure (cm), target with a 14 point font print and a metronome.
The test assesses vestibular and ocular motor impairments via patient-reported symptom provocation after each assessment[6]. The assessment includes a baseline measurement and 5 domains which are recorded in the table provided (see below). Patients verbally rate changes in headache, dizziness, nausea, and fogginess symptoms compared with their immediate pre-assessment state on a scale of 0 (none) to 10 (severe) after each VOMS assessment to determine if each assessment provokes symptoms.
Baseline Measurement[edit | edit source]
Prior to performing the 5 domains of the VOMS screen, it is important to establish the patient's baseline symptoms. On a scale of 0-10, ask the patient to score their symptoms at rest for headache, dizziness, nausea & fogginess.
For each Domain, symptom provocation should be considered a positive result.[11] Symptoms provocation can include, but not limited to: headache, dizziness, nausea and mental fogginess.
Domain 1: Smooth Pursuit[edit | edit source]
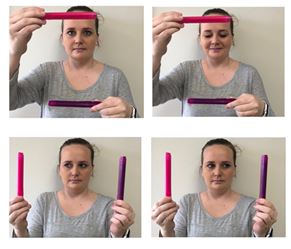
"Smooth pursuit eye movements are a type of conjugate eye movement that primarily allows both eyes to simultaneously follow a slow-moving target and maintain that image on the retina as the target moves. Smooth pursuits also work with the VOR to help maintain fixation on a target when the head and body is in motion. When smooth pursuits are impaired, the eyes will lose track of the moving object and use a saccadic eye-movement to recover or “catch up” to the target, making abnormal smooth pursuits look jerky on clinical examination." -Kaae C et al 2022.[2]
This tests the ability to follow a slowly moving target. The patient and the examiner are seated. The examiner holds a fingertip at a distance of 3 ft. from the patient. The patient is instructed to maintain focus on the target as the examiner moves the target smoothly in the horizontal direction 1.5 ft. to the right and 1.5 ft. to the left of midline. One repetition is complete when the target moves back and forth to the starting position, and 2 repetitions are performed. The target should be moved at a rate requiring approximately 2 seconds to go fully from left to right and 2 seconds to go fully from right to left. The test is repeated with the examiner moving the target smoothly and slowly in the vertical direction 1.5 ft. above and 1.5 ft. below midline for 2 complete repetitions up and down. Again, the target should be moved at a rate requiring approximately 2 seconds to move the eyes fully upward and 2 seconds to move fully downward.
Record: Headache, Dizziness, Nausea & Fogginess ratings after the test.
Domain 2: Saccades[edit | edit source]
"Saccadic eye movements are a conjugate eye movement that allow both eyes to move quickly in the same direction, rapidly shifting the eyes from one object of visual interest to another. Saccades can be made voluntarily or reflexively to visual, auditory, memory, and tactile stimuli. Clinically, when saccades are inaccurate in mTBI, they have been characterized as hypometric (undershoot the target) or hypermetric (overshoot the target), have slower velocities/increased latency, and smaller peak accelerations." -Kaae C et al 2022.[2]
This tests the ability of the eyes to move quickly between targets. The patient and the examiner are seated.
- Horizontal Saccades: The examiner holds two single points (fingertips) horizontally at a distance of 3 ft. from the patient, and 1.5 ft. to the right and 1.5 ft. to the left of midline so that the patient must gaze 30 degrees to left and 30 degrees to the right. Instruct the patient to move their eyes as quickly as possible from point to point. One repetition is complete when the eyes move back and forth to the starting position, and 10 repetitions are performed.
Record: Headache, Dizziness, Nausea & Fogginess ratings after the test.
- Vertical Saccades: Repeat the test with 2 points held vertically at a distance of 3 ft. from the patient, and 1.5 feet above and 1.5 feet below midline so that the patient must gaze 30 degrees upward and 30 degrees downward. Instruct the patient to move their eyes as quickly as possible from point to point. One repetition is complete when the eyes move up and down to the starting position, and 10 repetitions are performed.
Record: Headache, Dizziness, Nausea & Fogginess ratings after the test.
Domain 3: Convergence[edit | edit source]
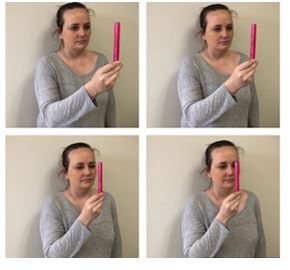
"Vergence eye movements are a disconjugate eye movement used to track an object moving closer or further away as well as look at objects that are located at different distances away. When looking at objects further away, both eyes move outwards, termed divergence. When looking at objects approaching closer, both eyes move inwards towards the nose, termed convergence. Both eyes need to make these movements at the same speed and magnitude in order for the brain to interpret a single and fused image perception (binocular vision). If the eyes do not move together in sync, the brain will either perceive two distinct images (ie double vision) due to the mismatched input from each eye, or the brain will perceive an overlap of images, which may be perceived as blurry vision or shadowing." -Kaae C et al 2022.[2]
Convergence is assessed by both symptom report and objective measurement of the near point of convergence (NPC).The NPC values are averaged across 3 trials, and normal NPC values are within 5 cm.[12]
Measure the ability to view a near target without double vision. The patient is seated and wearing corrective lenses (if needed). The examiner is seated in front of the patient and observes their eye movement during this test. The patient focuses on a small target (approximately 14 point font size) at arm’s length and slowly brings it toward the tip of their nose. The patient is instructed to stop moving the target when they see two distinct images (double vision) or when the examiner observes an outward deviation of one eye. Blurring of the image is ignored. The distance in centimetres between where the target is stopped, and the tip of nose, is measured and recorded using a tape measure. This is repeated a total of 3 times with measures recorded each time.
Record: Headache, Dizziness, Nausea & Fogginess ratings after the test. Abnormal: Near Point of convergence ≥ 6 cm from the tip of the nose.
Domain 4: Vestibular-Ocular Reflex (VOR) Test[edit | edit source]
Assess the ability to stabilise vision as the head moves. The patient and the examiner are seated. The examiner holds a target of approximately 14 point font size in front of the patient in the midline at a distance of 3 ft.
• Horizontal VOR Test: The patient is asked to rotate their head horizontally while maintaining focus on the target. Using a metronome set at 180 beats per minute (bpm), the head is moved at an amplitude of 20 degrees to each side with the beat. One repetition is complete when the head moves back and forth to the starting position, and 10 repetitions are performed.
Record: Headache, Dizziness, Nausea and Fogginess ratings after the test.
• Vertical VOR Test: The test is repeated with the patient moving their head vertically while maintaining focus on the target. Using a metronome set at 180 bpm, the head is moved in an amplitude of 20 degrees up and 20 degrees down with the beat. One repetition is complete when the head moves up and down to the starting position, and 10 repetitions are performed.
Record: Headache, Dizziness, Nausea and Fogginess ratings after the test.
Domain 5: Visual Motion Sensitivity (VMS) Test[edit | edit source]
Also known as VOR cancellation test.
Assess visual motion sensitivity and the ability to inhibit vestibular-induced eye movements using vision.
The patient stands with feet shoulder width apart, facing a busy area of the clinic. The examiner stands next to and slightly behind the patient, so that the patient is guarded but the movement can be performed freely. The patient holds arm outstretched and focuses on their thumb. Set the metronome to 50 bpm. Maintaining focus on their thumb, the patient rotates, together as a unit, their head, eyes and trunk at an amplitude of 80 degrees to the right and 80 degrees to the left, to the beat of the metronome. One repetition is complete when the trunk rotates back and forth to the starting position, and 5 repetitions are performed.
Record: Headache, Dizziness, Nausea & Fogginess ratings after a 10 second pause to allow for latent symptoms after the test[13].
Evidence[edit | edit source]
The VOMS has demonstrated internal consistency as well as sensitivity in identifying patients with concussions[6][14][15].
Mucha et al[6] found that the test demonstrates internal consistency and basic validity compared with the Post-Concussion Symptom Scale (PCSS). They also suggest that it may "provide preliminary evidence for the use of the VOMS to identify patients with sport-related concussions from healthy controls".
Moran et al[14] supported the implementation of the VOMS baseline assessment into clinical practice, due to a high internal consistency, strong relationships between VOMS items, and a low false-positive rate at baseline in youth athletes.
Anzalon et al[16] suggest that the VOMS can serve as a predictor of recovery time in patients with sports-related concussion.
Worts et al[17] found that the VOMS may be more stable than other screening measures and is less likely to result in false-positives than the King-Devick test in adolescent athletes.
Please view the following six-minute video for a quick demonstration of the VOMS. Please note how this professional discusses the importance of using this examination as part of a concussion assessment.
References[edit | edit source]
- ↑ UPMC Sports Medicine. Vestibular Ocular Motor Screening (VOMS). Available from: https://www.upmc.com/services/sports-medicine/services/concussion/symptoms-diagnosis/voms (accessed 16/11/2022).
- ↑ 2.0 2.1 2.2 2.3 2.4 Kaae C, Cadigan K, Lai K, Theis J. Vestibulo-ocular dysfunction in mTBI: Utility of the VOMS for evaluation and management–A review. NeuroRehabilitation. 2022 Jan 1;50(3):279-96.
- ↑ 3.0 3.1 Kontos AP, Elbin RJ, Schatz P, et al. A revised factor structure for the Post-Concussion Symptom Scale: baseline and postconcussion factors. Am J Sports Med. 2012;40(10):2375-2384.
- ↑ Ciuffreda KJ, Ludlam D, Thiagarajan P. Oculomotor diagnostic protocol for the mTBI population. Optometry. 2011;82(2):61-63.
- ↑ Lau BC, Kontos AP, Collins MW, Mucha A, Lovell MR. Which on-field signs/symptoms predict protracted recovery from sport-related concussion among high school football players? Am J Sports Med. 2011;39(11):2311-2318.
- ↑ 6.0 6.1 6.2 6.3 Mucha A, Collins MW, Elbin RJ, Furman JM, Troutman-Enseki C, DeWolf RM, Marchetti G, Kontos AP. A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions: preliminary findings. The American journal of sports medicine. 2014 Oct;42(10):2479-86.
- ↑ Yorke AM, Smith L, Babcock M, Alsalaheen B. Validity and Reliability of the Vestibular/Ocular Motor Screening and Associations With Common Concussion Screening Tools. Sports Health. 2017;9(2):174-80.
- ↑ Knell G, Caze T, Burkhart SO. Evaluation of the vestibular and ocular motor screening (VOMS) as a prognostic tool for protracted recovery following paediatric sports-related concussion. BMJ Open Sport & Exercise Medicine. 2021 Mar 1;7(1):e000970.
- ↑ 9.0 9.1 Kaae C, Cadigan K, Lai K, Theis J. Vestibulo-ocular dysfunction in mTBI: Utility of the VOMS for evaluation and management. A review. NeuroRehabilitation. 2022 Jan 1(Preprint):1-8.
- ↑ Parrington L, King LA, Hoppes CW, Klaiman MJ, Michielutti P, Fino PC, Dibble LE, Lester ME, Weightman MM. Exploring vestibular ocular motor screening in adults with persistent complaints after mild traumatic brain injury. Journal of head trauma rehabilitation. 2022 Sep 23;37(5):E346-54.
- ↑ Crampton A, Schneider KJ, Grilli L, Chevignard M, Katz-Leurer M, Beauchamp MH, Debert C, Gagnon IJ. Determining the Agreement Between Common Measures Related to Vestibulo-ocular Reflex Function After a Mild Traumatic Brain Injury in Children and Adolescents. Archives of Rehabilitation Research and Clinical Translation. 2022 Sep 1;4(3):100217.
- ↑ Scheiman M, Gallaway M, Frantz KA, et al. Nearpoint of convergence: test procedure, target selection, and normative data. Optom Vis Sci80(3) 2003:214-225
- ↑ Mucha A, Collins MW, Elbin RJ, Furman JM, Troutman-Enseki C, DeWolf RM, Marchetti G, Kontos AP. A brief vestibular/ocular motor screening (VOMS) assessment to evaluate concussions: preliminary findings. The American journal of sports medicine. 2014 Oct;42(10):2479-86.
- ↑ 14.0 14.1 Moran RN, Covassin T, Elbin RJ, Gould D, Nogle S. Reliability and normative reference values for the Vestibular/Ocular Motor Screening (VOMS) tool in youth athletes. The American journal of sports medicine. 2018 May;46(6):1475-80.
- ↑ Moran RN, Covassin T, Elbin RJ. Sex Differences on Vestibular and Ocular Motor Assessment in Youth Athletes. Journal of athletic training. 2019 Apr;54(4):445-8.
- ↑ Anzalone AJ, Blueitt D, Case T, McGuffin T, Pollard K, Garrison JC, Jones MT, Pavur R, Turner S, Oliver JM. A positive vestibular/ocular motor screening (VOMS) is associated with increased recovery time after sports-related concussion in youth and adolescent athletes. The American journal of sports medicine. 2017 Feb;45(2):474-9.
- ↑ Worts PR, Schatz P, Burkhart SO. Test Performance and Test-Retest Reliability of the Vestibular/Ocular Motor Screening and King-Devick Test in Adolescent Athletes During a Competitive Sport Season. Am J Sports Med. 2018;46(8):2004-10.