Urinary Incontinence
Original Editor - Kirsten Ryan
Lead Editors - Your name will be added here if you are a lead editor on this page. Read more.
Clinically Relevant Anatomy
[edit | edit source]
add text here relating to clinically relevant anatomy of the condition
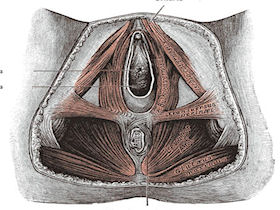
Pelvic Floor[edit | edit source]
The pelvic floor is made up of the muscles, ligaments, and fascial structures that act together to support the pelvic organs and to provide compressive forces to the urethra during increased intra-abdominal pressure.
The pelvic floor muscles refers to the muscular layer of the pelvic floor. It includes the levator ani, striated urogenital sphincter, external anal sphincter, ischiocavernosus, and bulbospongiosus.[1]
The urethra, vagina, and rectum pass through the pelvic floor and are surrounded by the pelvic floor muscles. During increased intra-abdominal pressure, the pelvic floor muscles must contract to provide support. When the pelvic floor muscles contract the urethra, anus, and vagina close. The contraction is important in preventing involuntary loss of urine or rectal contents. The pelvic floor muscles must also relax in order to void.[1]
Mechanism of Injury / Pathological Process
[edit | edit source]
Definitions: [edit | edit source]
- Urinary incontinence (symptom): Complaint of involuntary loss of urine.
- Stress (urinary) incontinence: Complaint of involuntary loss of urine on effort or physical exertion (e.g. sporting activities), or on sneezing or coughing.
- Urgency (urinary) incontinence: Complaint of involuntary loss of urine associated with urgency.
- Mixed (urinary) incontinence: Complaint of involuntary loss of urine associated with urgency and also effort or physical exertion or on sneezing or coughing.
- Urgency: Complaint of a sudden, compelling desire to pass urine which is difficult to defer.
- Overactive bladder (OAB, Urgency) syndrome: Urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology.[3]
Clinical Presentation[edit | edit source]
Urinary Leaking
Frequency
Urgency
Nocturia
Prolapse
Diagnostic Procedures[edit | edit source]
A large portion of women with urinary stress incontinence can be diagnosed from clinical history alone. In this systematic review, little evidence was found on the performance of urinary diaries, and pad-tests although they are common diagnostic assessments used in physical therapy.[4]
Clinical history[edit | edit source]
Clinical history taking compared with multi-channel urodynamics was found to have 0.92 sensitivity and 0.56 specificity for the diagnosis of urinary stress incontinence based on the presence of stress incontinence symptoms.[4]
Pelvic Floor Muscle Function and Strength[edit | edit source]
Pelvic Floor Muscle Function and Strength
Pelvic Floor Muscle Strength
Modified Oxford grading system: [edit | edit source]
0 - no contraction
1 - flicker
2 - weak squeeze, no lift
3 - fair squeeze, definite lift
4 - good squeeze with lift
5 - strong squeeze with a lift
Palpation of the pelvic floor muscles per the vagina in females and per the rectum in male patients.[5]
PERFECT mnemonic assessment, described by Jo Laycock:[edit | edit source]
P - power, may use the Modified Oxford grading scale
E - endurance, the time (in seconds) that a maximum contraction can be sustained
R - repetition, the number of repetitions of a maximum voluntary contraction
F - fast contractions, the number of fast (one second) maximum contractions
ECT - every contraction timed, reminds the therapist to continually overload the muscle activity for strengthening[5]
Pad Test[edit | edit source]
The 1 hour pad test was found to have 0.94 sensitivity and 0.44 specificity for diagnosing any leakage compared with multi-channel urodynamics.
The 48 hour pad-test was found to have 0.92 sensitivity and 0.72 specificity for the diagnosis of urinary stress incontinence.[4]
Urinary (Voiding) Diary[edit | edit source]
One study found a scale derived from a 7 day diary was 0.88 sensitive and 0.83 specific for the diagnosis of detrusor overactivity in women.[4]
Outcome Measures[edit | edit source]
- Incontinence Quality of Life Instrument (I-QOL)
- Male Urogenital Distress Inventory (MUDI)
- Male Urinary Symptom Impact Questionnaire (MUSIQ)
- Patient Global Impression of Improvement (PGI-I)
- Patient Global Impression of Severity (PGI-S)
- Pelvic Floor Distress Inventory - 20 (PFDI - 20)
- Pelvic Floor Impact Questionnaire - 7 (PFIQ - 7)
Management / Interventions
[edit | edit source]
The Knack maneuver:[edit | edit source]
The Knack maneuver essentially is a voluntary contraction performed in response to a specific situation. Teach a voluntary contraction of the pelvic floor muscles with appropriate timing, for example, just prior to a cough or sneeze. It is a useful strategy in patients with stress urinary incontinence.[6]
Pelvic Floor Muscle Training[edit | edit source]
Behavioral Therapy[edit | edit source]
The focus of behavioral therapy is on lifestyle changes such as fluid or diet management, weight control, and bowel regulation. Education about bladder irritants, like caffeine, is an important consideration. Also, discussing bowel habits to determine if constipation is an issue. It is important to educate the patient about avoiding straining.[7]
Bladder Training[edit | edit source]
The information gathered from the bladder diary is used to guide decision making for bladder re-training, including a voiding schedule if necessary to increase the capacity of the bladder for people with frequency issues. Bladder training attempts to break the cycle by teaching patients to void on a schedule, rather than in response to urgency. Urge suppression techniques are taught, for example, distraction and relaxation. It is also important to teach the patient to contract the pelvic floor to induce detrusor inhibition.[8]
Differential Diagnosis
[edit | edit source]
Multi-channel urodynamics testing is the gold standard for making a condition-specific diagnosis. This testing is typically done in secondary care, not in primary care or physical therapy.[4]
Key Evidence[edit | edit source]
add text here relating to key evidence with regards to any of the above headings
A systematic review published in the Annals of Internal Medicine in 2008 found good evidence that pelvic floor muscle training and bladder training resolved urinary incontinence in women. However, the effects of electrostimulation, medical devices, injectable bulking agents, and local estrogen therapy were inconsistent.[9]
Resources
[edit | edit source]
add appropriate resources here
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1HU7eBGY7ASJd2ThtMkTHAX8SCSlU38pI5yF_Tn2LBY8SrtQVJ|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Messelink B, Benson T, Berghmans B, Bo K, Corcos J, Fowler C, Laycck J, Huat-Chye Lim P, van Lunsen R, Lycklama a Nijeholt G, Pemberton J, Wang A, Watier A, Van Kerrebrocck P. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourol Urodyn 2005;24:374-380.
- ↑ Natural Childbirth. Childbirth and your pelvic floor. http://childbirth.amuchbetterway.com/childbirth-and-your-pelvic-floor/ (accessed 15 March 2011).
- ↑ Abrams P, Cardozo L, Fall M, et al. The standardization of terminology in lower urinary tract function: report from the standardization sub-committee of the International Continence Society. Urology 2003;61:37-49.
- ↑ 4.0 4.1 4.2 4.3 4.4 Martin JL, Williams KS, Sutton AJ, Abrams KR, Assassa RP. Systematic review and meta-analysis of methods of diagnostic assessment for urinary incontinence. Neurourol Dynam 2006;25:674-683.
- ↑ 5.0 5.1 Laycock J. Pelvic muscle exercises: physiotherapy for the pelvic floor. Urologic Nursing 1994;14:136-40.
- ↑ Miller JM, Sampselle C, Ashton-Miller J, Son Hong G-R, De Lancey JOL. Clarification and confirmation of the Knack maneuver: the effect of volitional pelvic floor muscle contraction to preempt expected stress incontinence. Int Urogynecol J 2008;19:773-782.
- ↑ Burgio KL. Current perspectives on management of urgency using bladder and behavioral training. J Am Academy Nurse Pract 2004;16:4-7.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedburgio - ↑ Shamliyan TA, Kane RL, Wyman J, Wilt TJ. Systematic review: randomized, controlled trials of nonsurgical treatments for urinary incontinence in women. Ann Intern Med 2008;148:459-474.