Upper Limb Management in Lower Tetraplegia and Central Cord Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
== Introduction == | == Introduction == | ||
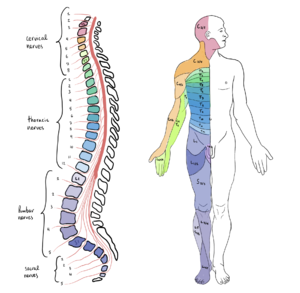
[[File:Spinal Cord Segments and body representation.png|thumb]] | [[File:Spinal Cord Segments and body representation.png|thumb]] | ||
Upper limb function is vital | Upper limb function is vital for individuals with cervical [[Spinal Cord Injury|spinal cord injury]] (SCI) to regain autonomy. There are conservative management options and surgical pathways available. Conservative treatment includes positioning, [[splinting]], passive and active [[Range of Motion|range of motion]], functional training, and training with adaptive equipment to offer the best possible benefit to the individual patient.<ref name=":0">Bersch I, Krebs J, Fridén J. A [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9397669/pdf/fresc-03-889577.pdf Prediction Model for Various Treatment Pathways of Upper Extremity in Tetraplegia.] Front Rehabil Sci. 2022 Jun 30;3:889577. </ref> Prevention must be considered when treatment strategies are selected. [[Claw Hand|Claw hand]], contractures or inadequate closing or opening of the fingers may occur with lower-level cervical spinal cord injury.<ref name=":0" /> The treatment strategy depends on the type of damage present (upper vs lower [[Motor Neurone|motor neuron]]). This article will discuss upper limb function with lower-level cervical spinal cord injury and its impact on an individual's functional abilities. | ||
== C6 [[Tetraplegia]] == | == C6 [[Tetraplegia]] == | ||
# Innervated upper limb muscles | # Innervated upper limb muscles in C6 spinal cord injury | ||
#* [[Deltoid]], [[Biceps Brachii|biceps]], [[Brachialis|brachialis,]] [[brachioradialis]] (C5 level) | #*[[Deltoid]], [[Biceps Brachii|biceps]], [[Brachialis|brachialis,]] [[brachioradialis]] (C5 level) | ||
#* [[Pectoralis major|Pectoralis]] (clavicular head only) | #* [[Pectoralis major|Pectoralis]] (clavicular head only) | ||
#* [[Supinator]] | #* [[Supinator]] | ||
| Line 25: | Line 25: | ||
#* Able to extend the wrist, rotate and adduct the shoulder<ref name=":2">Oelofse W. Upper Limb Management in Lower Tetraplegia - Occupational Therapy Course. Plus 2022</ref> | #* Able to extend the wrist, rotate and adduct the shoulder<ref name=":2">Oelofse W. Upper Limb Management in Lower Tetraplegia - Occupational Therapy Course. Plus 2022</ref> | ||
#* Improved weight bearing through the upper limbs due to the function of [[Latissimus Dorsi Muscle|latissimus dorsi]] and pectoralis | #* Improved weight bearing through the upper limbs due to the function of [[Latissimus Dorsi Muscle|latissimus dorsi]] and pectoralis | ||
Goals for upper limb | Goals for upper limb management: | ||
* To prevent upper limb | * To prevent secondary complications in the upper limb, including the development of contractures and deformities<ref name=":1">Arsh A, Anwar Z, Zeb A, Ilyas SM. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6994917/pdf/PJMS-36-96.pdf Effectiveness of occupational therapy in improving activities of daily living performance in complete cervical tetraplegic patients; A quasi-experimental study.] Pak J Med Sci. 2020 Jan-Feb;36(2):96-99.</ref> | ||
* To assist with function: optimise independence with activities of daily living (ADLs), including eating, dressing, meal | * To assist with function: i.e. optimise independence with activities of daily living (ADLs), including eating, dressing, meal preparation, grooming, bladder and bowel programme<ref name=":3">Yarkony GM, Roth EJ, Heinemann AW, Lovell L. [https://www.nature.com/articles/sc198828.pdf?origin=ppub Rehabilitation outcomes in C6 tetraplegia.] Paraplegia. 1988 Jun;26(3):177-85.</ref> | ||
* To gain community integration | * To gain community integration by learning transfers with assistance and independent [[Wheelchair Biomechanics|wheelchair propulsion]]<ref name=":1" /> | ||
Factors effecting outcomes:<ref name=":3" /> | Factors effecting outcomes:<ref name=":3" /> | ||
| Line 37: | Line 37: | ||
* Complications of spinal cord injury | * Complications of spinal cord injury | ||
=== Prevention of Development of | === Prevention of Development of Upper Limb Deformities === | ||
==== Prevention of Contracture in the Fingers ==== | ==== Prevention of Contracture in the Fingers ==== | ||
''' | '''Boxing glove:'''<ref name=":2" /> | ||
* Maintains range of motion | * Maintains range of motion | ||
* Prevents contractures in the fingers | * Prevents contractures in the fingers | ||
* Encourages correct positioning for | * Encourages correct positioning for a tenodesis grasp | ||
* Has a positive effect on [[Oedema Assessment|oedema]] management | * Has a positive effect on [[Oedema Assessment|oedema]] management | ||
==== Prevention of Contracture in the Elbow ==== | ==== Prevention of Contracture in the Elbow ==== | ||
* Teach the patient to maintain elbow extension while flexing the shoulders during functional tasks | * Teach the patient to maintain elbow extension while flexing the shoulders during functional tasks, such as mat activities and bed mobility | ||
* Teach the patient to contract the anterior deltoid and the upper fibres of the pectoralis major and relax the biceps | * Teach the patient to contract the anterior deltoid and the upper fibres of the pectoralis major and to relax the biceps | ||
* Teach the patient to lock the elbow by externally rotating the shoulders, extending the elbow and the wrist, and supinating the forearm | * Teach the patient to lock the elbow by externally rotating the shoulders, extending the elbow and the wrist, and supinating the forearm | ||
==== Prevention of Development of | ==== Prevention of Development of Upper Limb Pain ==== | ||
Risk factors: | Risk factors: | ||
* Females more often than males<ref name=":4">Barbetta DC, Lopes AC, Chagas FN, Soares PT, Casaro FM, Poletto MF, de Carvalho Paiva Ribeiro YH, Ogashawara TO. [https://www.nature.com/articles/sc2015126 Predictors of musculoskeletal pain in the upper extremities of individuals with spinal cord injury.] Spinal Cord. 2016 Feb;54(2):145-9.</ref> | * Females are affected more often than males<ref name=":4">Barbetta DC, Lopes AC, Chagas FN, Soares PT, Casaro FM, Poletto MF, de Carvalho Paiva Ribeiro YH, Ogashawara TO. [https://www.nature.com/articles/sc2015126 Predictors of musculoskeletal pain in the upper extremities of individuals with spinal cord injury.] Spinal Cord. 2016 Feb;54(2):145-9.</ref> | ||
* Age over 40<ref name=":4" /> | * Age over 40 years<ref name=":4" /> | ||
* Less than 1 year since the spinal cord injury<ref name=":4" /> | * Less than 1 year since the spinal cord injury<ref name=":4" /> | ||
* Higher [[Body Mass Index|body mass index]] (BMI)<ref>Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, Part I: Epidemiology, aetiology, and pathomechanics. J Spinal Cord Med. 2004;27(1):4-17. </ref> | * Higher [[Body Mass Index|body mass index]] (BMI)<ref>Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, Part I: Epidemiology, aetiology, and pathomechanics. J Spinal Cord Med. 2004;27(1):4-17. </ref> | ||
* | * Using a manual wheelchair | ||
* Risks associated with a spinal cord injury at the cervical level: | * Risks associated with a spinal cord injury at the cervical level: | ||
** | ** Upper extremity immobilisation | ||
** | ** Upper extremity reduction in the range of motion in the acute phase | ||
** | ** Muscle shortening and shoulder capsule tightness | ||
** | ** Impaired muscle strength from weakness | ||
** [[ | ** [[Spasticity]] | ||
"Pain in the upper extremities of SCI patients is an incapacitating condition."<ref name=":4" /> It interferes with all patient | "Pain in the upper extremities of SCI patients is an incapacitating condition."<ref name=":4" /> It interferes with all patient activities, including transfer skills, pressure relief and wheelchair mobility. Prevention and early management of upper limb pain in persons with tetraplegia should be addressed at every stage of rehabilitation. | ||
The following are examples of therapeutic interventions | The following are examples of therapeutic interventions that aim to reduce upper limb pain:<ref name=":4" /> | ||
* Increasing patient | * Increasing patient / caregiver knowledge of upper limb biomechanics | ||
* Implementing appropriate daily | * Implementing appropriate daily life activity techniques, including wheelchair propulsion | ||
* Avoiding overuse and weight-bearing through the upper limbs | * Avoiding overuse and weight-bearing through the upper limbs | ||
* Designing a balanced muscle fitness | * Designing a balanced muscle fitness programme for the upper extremity | ||
* Establishing a nutritional orientation with a weight control focus | * Establishing a nutritional orientation with a weight control focus | ||
* Postural optimisation in the appropriate wheelchair | * Postural optimisation in the appropriate wheelchair | ||
* Evaluating | * Evaluating indications for adaptive devices and environmental changes | ||
=== Assisting with Function === | === Assisting with Function === | ||
[[File:Tenodesis grasp.jpeg|thumb|<small><nowiki>https://commons.wikimedia.org/wiki/File:Wrist_related_tenodesis_effect,_second_step.JPG</nowiki></small>|alt=]] | [[File:Tenodesis grasp.jpeg|thumb|<small>Tenodesis grasp. <nowiki>https://commons.wikimedia.org/wiki/File:Wrist_related_tenodesis_effect,_second_step.JPG</nowiki></small>|alt=]] | ||
==== [[Tenodesis Function in Spinal Cord Injury|Tenodesis Grasp]] <ref>Harvey LA, Herbert RD. [https://www.nature.com/articles/3101241 Muscle stretching for treatment and prevention of contracture in people with spinal cord injury.] Spinal Cord. 2002 Jan;40(1):1-9. </ref> ==== | ==== [[Tenodesis Function in Spinal Cord Injury|Tenodesis Grasp]]<ref>Harvey LA, Herbert RD. [https://www.nature.com/articles/3101241 Muscle stretching for treatment and prevention of contracture in people with spinal cord injury.] Spinal Cord. 2002 Jan;40(1):1-9. </ref> ==== | ||
* | * Requires contracture in flexor pollicis longus and the extrinsic finger flexor muscles | ||
* Active wrist extension passively pulls the fingers and thumb into flexion | * Active wrist extension passively pulls the fingers and thumb into flexion | ||
* Objects can be passively held between the thumb and index finger or in the palm | * Objects can be passively held between the thumb and index finger or in the palm | ||
'''Methods to encourage/develop a good tenodesis grasp''' <ref name=":2" /> | '''Methods to encourage/develop a good tenodesis grasp'''<ref name=":2" /> | ||
* Perform passive range of motion (PROM) | * Perform passive range of motion (PROM) exercises daily | ||
* Proper sequence of PROM includes the wrist down (flexed) when fingers are opened (extended) | * Proper sequence of PROM includes the wrist down (flexed) when fingers are opened (extended); fingers closed (flexed) when wrist comes up (extends) | ||
* Reach and preserve mild tension in the long finger flexors without overstretching or shortening the flexors | * Reach and preserve mild tension in the long finger flexors without overstretching or shortening the flexors | ||
* Maintain the webspace | * Maintain the webspace | ||
* A thumb opponens splint may be prescribed to increase tenodesis grasp | * A thumb opponens splint (see below) may be prescribed to increase tenodesis grasp as it helps to maintain proper thumb position | ||
| Line 103: | Line 103: | ||
{{#ev:youtube|v=T_cFWDum3KU|300}}<ref>AmputeeOT: What is a tenodesis splint?Available from: https://www.youtube.com/watch?v=T_cFWDum3KU [last accessed 28/11/2022]</ref> | {{#ev:youtube|v=T_cFWDum3KU|300}}<ref>AmputeeOT: What is a tenodesis splint?Available from: https://www.youtube.com/watch?v=T_cFWDum3KU [last accessed 28/11/2022]</ref> | ||
=== C7 | === C7 Tetraplegia === | ||
# Innervated upper limb muscles | # Innervated upper limb muscles in C7 spinal cord injury | ||
#* All muscles at the C6 level | #* All muscles at the C6 level | ||
#* Pectoralis (sternal head) | #* Pectoralis (sternal head) | ||
| Line 113: | Line 113: | ||
#* [[Extensor Digitorum Communis|Extensor digitorum communis]] (finger extensor) | #* [[Extensor Digitorum Communis|Extensor digitorum communis]] (finger extensor) | ||
# Weak fingers and/or thumb extension may be present | # Weak fingers and/or thumb extension may be present | ||
# No | # No finger or thumb flexion | ||
# Functional impact | # Functional impact | ||
#* Able to lift arms above shoulder level | #* Able to lift arms above shoulder level | ||
| Line 121: | Line 121: | ||
Goals for upper limb | Goals for upper limb management: | ||
* To prevent upper limb | * To prevent secondary complications of the upper limb, including the development of contractures and deformities.<ref name=":1" /> | ||
* To assist with function: optimise independence with | * To assist with function: e.g. optimise independence with ADLs, including eating, dressing, meal preparation, grooming, bladder and bowel programme<ref name=":3" /> | ||
* To gain community integration through '''independent [[Transfer Boards|transfers]] without sliding board''' <ref name=":6">Rodríguez-Mendoza B, Santiago-Tovar PA, Guerrero-Godinez MA, García-Vences E. Rehabilitation Therapies in Spinal Cord Injury Patients. Paraplegia. 2020 Jun 17.</ref> and independent wheelchair propulsion<ref name=":1" /> | * To gain community integration through '''independent [[Transfer Boards|transfers]] without a sliding board'''<ref name=":6">Rodríguez-Mendoza B, Santiago-Tovar PA, Guerrero-Godinez MA, García-Vences E. Rehabilitation Therapies in Spinal Cord Injury Patients. Paraplegia. 2020 Jun 17.</ref> and independent wheelchair propulsion<ref name=":1" /> | ||
== C8 | == C8 Tetraplegia == | ||
# Innervated upper limb muscles | # Innervated upper limb muscles in C8 spinal cord injury | ||
## All muscles at the C7 level | ## All muscles at the C7 level | ||
## Ulnar wrist extensor | ## Ulnar wrist extensor | ||
| Line 135: | Line 135: | ||
# No intrinsics | # No intrinsics | ||
# No thumb abduction | # No thumb abduction | ||
# Functional impact | # Functional impact: | ||
## Limited grip function | ## Limited grip function - an active hand is achievable if there is flexor force of at least 3-4/5<ref name=":7">Suszek-Corradetti M. [http://apgr.wssp.edu.pl/wp-content/uploads/2021/02/APGR-24-2-5.pdf Rehabilitation path for patients with spinal cord injury from critical condition to optimal independence in everyday life on the example of the activities of the Montecatone Rehabilitation Institute in Italy.] Archives of Physiotherapy & Global Researches. 2020 Jul 1;24(2).</ref> | ||
## Use of enlarged, thick and soft grasps for daily activities <ref name=":7" /> | ## Use of enlarged, thick and soft grasps for daily activities<ref name=":7" /> | ||
## No fine motor control | ## No fine motor control | ||
## Deformities of the hand may develop due to hand muscle imbalance ( | ## Deformities of the hand may develop due to hand muscle imbalance (claw hand) | ||
Goals for | Goals for upper limb management: | ||
* To prevent upper limb | * To prevent secondary complications of the upper limb, including the development of contractures and deformities.<ref name=":1" /> | ||
* To assist with function: optimise independence with | * To assist with function: optimise independence with ADLs, including eating, dressing, meal preparation, grooming, bladder and bowel programme.<ref name=":3" /> | ||
* To gain community integration through independent transfers without sliding board | * To gain community integration through independent transfers without a sliding board, '''advanced wheelchair skills''', and '''driving with adaptations'''.<ref name=":6" /> | ||
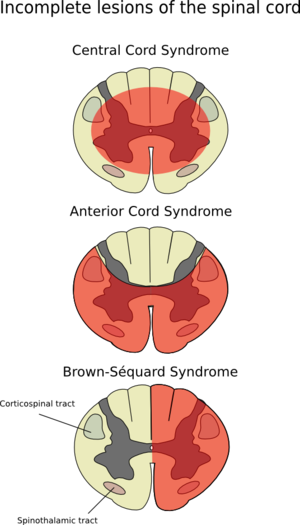
[[File:Spinal Cord Lesions and Syndromes.jpeg|thumb|Incomplete Spinal Cord Injuries]] | [[File:Spinal Cord Lesions and Syndromes.jpeg|thumb|Incomplete Spinal Cord Injuries]] | ||
== Incomplete Spinal Cord Injury == | == Incomplete Spinal Cord Injury == | ||
The term incomplete spinal cord injury " is used when there is | The term "incomplete spinal cord injury" is used when there is "preservation of any sensory and/or motor function below the neurological level that includes the lowest sacral segments S4–5 (i.e., presence of “sacral sparing”)."<ref name=":9">Rupp R, Biering-Sørensen F, Burns SP, Graves DE, Guest J, Jones L, Read MS, Rodriguez GM, Schuld C, Tansey-Md KE, Walden K. [https://meridian.allenpress.com/tscir/article/27/2/1/465525/International-Standards-for-Neurological International standards for neurological classification of spinal cord injury: revised 2019.] Topics in spinal cord injury rehabilitation. 2021;27(2):1-22.</ref> | ||
'''Goals for | '''Goals for upper limb management''' | ||
* Prevent complications | * Prevent complications | ||
* Improve function | * Improve function | ||
'''General Guidelines for | '''General Guidelines for upper limb management in incomplete spinal cord injury'''<ref name=":2" /> | ||
* Complete a comprehensive baseline assessment | * Complete a comprehensive baseline assessment | ||
| Line 161: | Line 161: | ||
* Continuously assess and reassess to align treatment aims with strategies | * Continuously assess and reassess to align treatment aims with strategies | ||
'''Treatment strategies for | '''Treatment strategies for upper limb management'''<ref name=":2" /> | ||
* | * Upper limb positioning | ||
* Early out-of-bed mobilisation | * Early out-of-bed mobilisation | ||
* Activities in | * Activities in an upright position using a tilt table or standing frame | ||
* Stimulation | * Stimulation a more normal movement pattern: therapist-directed activities, hand-over-hand guidance | ||
[[File:Incomplete Spinal Cord Injury.png|thumb|Central Cord Syndrome, Anterior Cord Syndrome, Brown-Sequard Syndrome]] | [[File:Incomplete Spinal Cord Injury.png|thumb|Central Cord Syndrome, Anterior Cord Syndrome, Brown-Sequard Syndrome]] | ||
==[[Central Cord Syndrome]] == | ==[[Central Cord Syndrome]] == | ||
"Central cord syndrome is the most common clinical syndromes, often seen in individuals with underlying cervical spondylosis who sustain a hyperextension injury (most commonly from a fall), and may occur with or without fracture and dislocations."<ref name=":9" /> | "Central cord syndrome is the most common of the clinical syndromes, often seen in individuals with underlying cervical spondylosis who sustain a hyperextension injury (most commonly from a fall), and may occur with or without fracture and dislocations. This clinically will present as an incomplete injury with greater weakness in the upper limbs than in the lower limbs."<ref name=":9" /> | ||
'''Pathophysiology''' | '''Pathophysiology''' | ||
| Line 190: | Line 190: | ||
* Shoulder pain and/or shoulder subluxation <ref name=":2" /> | * Shoulder pain and/or shoulder subluxation <ref name=":2" /> | ||
* Hand oedema <ref name=":2" /> | * Hand oedema <ref name=":2" /> | ||
* Joint contractures of the upper limbs <ref name=":2" /> | * Joint contractures of the upper limbs<ref name=":2" /> | ||
'''Treatment strategies for | '''Treatment strategies for upper limb management'''<ref name=":2" /> | ||
* | * Varies based on the level of injury - e.g., with central cord syndrome at the level of C5, poor proximal stability at the shoulder and the elbow must be addressed | ||
* Spasticity management | * Spasticity management | ||
* | * Upper limb pain management | ||
* | * Upper limb positioning strategies in sitting, standing and during ambulation | ||
== Upper Limb [[Splinting]] == | == Upper Limb [[Splinting]] == | ||
| Line 202: | Line 202: | ||
* Almost exclusively custom-made | * Almost exclusively custom-made | ||
* Facilitates tenodesis by opposing the thumb and preventing thumb overstretching during functional tasks | * Facilitates tenodesis by opposing the thumb and preventing thumb overstretching during functional tasks | ||
* Worn as needed to increase function | * Worn as needed to increase function | ||
* Facilitates tenodesis for individuals with wrist extension 3-5/5 and | * Facilitates tenodesis for individuals with wrist extension 3-5/5 and digits 0-2/5 | ||
* Recommended for individuals with C6, C7-8 SCI | * Recommended for individuals with C6, C7-8 SCI | ||
| Line 212: | Line 212: | ||
* Prefabricated wrist splints are preferred | * Prefabricated wrist splints are preferred | ||
* Worn during the day to increase functional activity participation | * Worn during the day to increase functional activity participation | ||
* Dorsal varieties and a U-Cuff are | * Dorsal varieties and a U-Cuff are preferred options | ||
* The primary wrist splint | * The primary goal of a wrist splint is to prevent overstretching of the wrist extensors; adding a universal cuff provides a stable base for ADLs | ||
* '''Clinical Practice Guidelines''': for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5 | * '''Clinical Practice Guidelines''': for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5 | ||
* Most commonly used in a C5 SCI (73% of patients) and C4 (40% of patients) | * Most commonly used in a C5 SCI (73% of patients) and C4 (40% of patients) | ||
''' | '''Metacarpophalangeal''' ('''MCP) blocking splint''' | ||
* Custom-made splint | * Custom-made splint | ||
* Prevents hyperextension deformity of the MCP joints | * Prevents hyperextension deformity of the MCP joints | ||
* | * Prevents MCP hyperextension during functional hand tasks | ||
* Recommended for patients with C7 | * Recommended for patients with C7, C8 spinal cord injury if intrinsic hand weakness is present | ||
More information on | More information on upper limb splinting in tetraplegia is available [https://www.physio-pedia.com/Upper_Limb_Management_in_C4_and_C5_SCI#Upper_Limb_Splinting here.] | ||
== Exercise Therapy == | == Exercise Therapy == | ||
=== Strengthening Exercises === | === Strengthening Exercises === | ||
According to the literature,<ref name=":5" /><ref>Atkins MS, Baumgarten JM, Yasuda YL, Adkins R, Waters RL, Leung P, Requejo P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2582429/pdf/i1079-0268-31-4-388.pdf Mobile arm supports: evidence-based benefits and criteria for use]. J Spinal Cord Med. 2008;31(4):388-93.</ref> <ref>DiCarlo SE. Effect of arm ergometry training on wheelchair propulsion endurance of individuals with quadriplegia. Phys Ther. 1988 Jan;68(1):40-4.</ref> strengthening exercises | According to the literature,<ref name=":5" /><ref>Atkins MS, Baumgarten JM, Yasuda YL, Adkins R, Waters RL, Leung P, Requejo P. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2582429/pdf/i1079-0268-31-4-388.pdf Mobile arm supports: evidence-based benefits and criteria for use]. J Spinal Cord Med. 2008;31(4):388-93.</ref> <ref>DiCarlo SE. Effect of arm ergometry training on wheelchair propulsion endurance of individuals with quadriplegia. Phys Ther. 1988 Jan;68(1):40-4.</ref> strengthening exercises such as arm ergometry, resistance training, the use of mobile arm supports, or virtual reality improves the overall performance of functional daily activities in individuals with a spinal cord injury. Exercise therapy effectively improves functional outcomes in patients with tetraplegia when conducted according to the following three training principles. | ||
'''Three principles of training''':<ref name=":5">Kloosterman MG, Snoek GJ, Jannink MJ. [https://www.nature.com/articles/sc2008113 Systematic review of the effects of exercise therapy on the upper extremity of patients with spinal cord injury]. Spinal Cord. 2009 Mar;47(3):196-203.</ref> | '''Three principles of training''':<ref name=":5">Kloosterman MG, Snoek GJ, Jannink MJ. [https://www.nature.com/articles/sc2008113 Systematic review of the effects of exercise therapy on the upper extremity of patients with spinal cord injury]. Spinal Cord. 2009 Mar;47(3):196-203.</ref> | ||
| Line 235: | Line 235: | ||
* Overload (the most important) | * Overload (the most important) | ||
** System or tissue must be challenged with the intensity, duration and frequency of exercise | ** System or tissue must be challenged with the intensity, duration and frequency of exercise | ||
** The outcome depends on the patient's motivation and feedback received (augmented feedback <ref>van Dijk H, Jannink MJ, Hermens HJ. [https://www.medicaljournals.se/jrm/content/abstract/10.1080/16501970510030165 Effect of augmented feedback on motor function of the affected upper extremity in rehabilitation patients: a systematic review of randomized controlled trials]. J Rehabil Med. 2005 Jul;37(4):202-11.</ref>), and structure of practice (task specificity and goal-orientated practice) | ** The outcome depends on the patient's motivation and feedback received (augmented feedback<ref>van Dijk H, Jannink MJ, Hermens HJ. [https://www.medicaljournals.se/jrm/content/abstract/10.1080/16501970510030165 Effect of augmented feedback on motor function of the affected upper extremity in rehabilitation patients: a systematic review of randomized controlled trials]. J Rehabil Med. 2005 Jul;37(4):202-11.</ref>), and structure of practice (task specificity and goal-orientated practice) | ||
* Specificity | * Specificity | ||
** The training effect is limited to the system and tissues involved in the activity | ** The training effect is limited to the system and tissues involved in the activity | ||
| Line 241: | Line 241: | ||
** Gains are quickly lost when the overload is removed | ** Gains are quickly lost when the overload is removed | ||
'''Examples of exercise therapy applied in therapy | '''Examples of exercise therapy applied in therapy programmes for patients with tetraplegia''':<ref name=":5" /> | ||
* | * Virtual Reality: offers repetitive practice, feedback about performance and motivation<ref>Palaniappan SM, Suresh S, Haddad JM, Duerstock BS. Adaptive Virtual Reality Exergame for Individualized Rehabilitation for Persons with Spinal Cord Injury. In European Conference on Computer Vision 2020 Aug 23 (pp. 518-535). Springer, Cham.</ref> | ||
* Use of robotics to increase therapy intensity | * Use of robotics to increase therapy intensity | ||
=== Functional Passive Range of Motion (FPROM) === | === Functional Passive Range of Motion (FPROM) === | ||
Patients with lower tetraplegia present with <ref name=":8">Frye SK, Geigle PR, York HS, Sweatman WM. Functional passive range of motion of individuals with chronic cervical spinal cord injury. The Journal of Spinal Cord Medicine. 2020 Mar 3;43(2):257-63.</ref> | Patients with lower tetraplegia present with:<ref name=":8">Frye SK, Geigle PR, York HS, Sweatman WM. Functional passive range of motion of individuals with chronic cervical spinal cord injury. The Journal of Spinal Cord Medicine. 2020 Mar 3;43(2):257-63.</ref> | ||
* Limitations in forearm pronation | * Limitations in forearm pronation | ||
* Limitations in elbow extension or elbow hyperextension | * Limitations in elbow extension or elbow hyperextension - elbow hyperextension was present in one-third of patients participating in the study<ref name=":8" /> | ||
* Increased shoulder extension | * Increased shoulder extension | ||
* Increased wrist extension | * Increased wrist extension | ||
According to research <ref name=":8" /> | According to research,<ref name=":8" /> shoulder horizontal adduction and elbow extension were associated with functional performance. | ||
The goal | The goal of FPROM: | ||
# To develop long-term plans for passive range of motion exercises to optimise functional abilities | # To develop long-term plans for passive range of motion exercises to optimise functional abilities | ||
== Resources == | == Resources == | ||
*Web-based teaching and educational resource for medical and paramedical professionals involved in SCI Management https://www.elearnsci.org/pages.aspx?id=16&page=Who_are_we | *Web-based teaching and educational resource for medical and paramedical professionals involved in SCI Management: https://www.elearnsci.org/pages.aspx?id=16&page=Who_are_we | ||
*[https://meridian.allenpress.com/tscir/article/27/2/1/465525/International-Standards-for-Neurological International Standards for Neurological Classification of Spinal Cord Injury: Revised 2019] | *[https://meridian.allenpress.com/tscir/article/27/2/1/465525/International-Standards-for-Neurological International Standards for Neurological Classification of Spinal Cord Injury: Revised 2019] | ||
== References == | == References == | ||
Revision as of 03:06, 9 December 2022
Original Editor - Ewa Jaraczewska based on the course by Wendy Oelofse
Top Contributors - Ewa Jaraczewska, Jess Bell and Tarina van der Stockt
Introduction[edit | edit source]
Upper limb function is vital for individuals with cervical spinal cord injury (SCI) to regain autonomy. There are conservative management options and surgical pathways available. Conservative treatment includes positioning, splinting, passive and active range of motion, functional training, and training with adaptive equipment to offer the best possible benefit to the individual patient.[1] Prevention must be considered when treatment strategies are selected. Claw hand, contractures or inadequate closing or opening of the fingers may occur with lower-level cervical spinal cord injury.[1] The treatment strategy depends on the type of damage present (upper vs lower motor neuron). This article will discuss upper limb function with lower-level cervical spinal cord injury and its impact on an individual's functional abilities.
C6 Tetraplegia[edit | edit source]
- Innervated upper limb muscles in C6 spinal cord injury
- Deltoid, biceps, brachialis, brachioradialis (C5 level)
- Pectoralis (clavicular head only)
- Supinator
- Radial wrist extensors (extensor carpi radialis longus and/or brevis)
- No elbow extension
- No active movements of fingers or thumbs
- Functional impact
- Unable to raise arms above shoulder level without external rotation
- Potential for tenodesis grip
- Able to extend the wrist, rotate and adduct the shoulder[2]
- Improved weight bearing through the upper limbs due to the function of latissimus dorsi and pectoralis
Goals for upper limb management:
- To prevent secondary complications in the upper limb, including the development of contractures and deformities[3]
- To assist with function: i.e. optimise independence with activities of daily living (ADLs), including eating, dressing, meal preparation, grooming, bladder and bowel programme[4]
- To gain community integration by learning transfers with assistance and independent wheelchair propulsion[3]
Factors effecting outcomes:[4]
- Patient's motivation
- Patient's physique
- Patient's psychosocial status
- Complications of spinal cord injury
Prevention of Development of Upper Limb Deformities[edit | edit source]
Prevention of Contracture in the Fingers[edit | edit source]
Boxing glove:[2]
- Maintains range of motion
- Prevents contractures in the fingers
- Encourages correct positioning for a tenodesis grasp
- Has a positive effect on oedema management
Prevention of Contracture in the Elbow[edit | edit source]
- Teach the patient to maintain elbow extension while flexing the shoulders during functional tasks, such as mat activities and bed mobility
- Teach the patient to contract the anterior deltoid and the upper fibres of the pectoralis major and to relax the biceps
- Teach the patient to lock the elbow by externally rotating the shoulders, extending the elbow and the wrist, and supinating the forearm
Prevention of Development of Upper Limb Pain[edit | edit source]
Risk factors:
- Females are affected more often than males[5]
- Age over 40 years[5]
- Less than 1 year since the spinal cord injury[5]
- Higher body mass index (BMI)[6]
- Using a manual wheelchair
- Risks associated with a spinal cord injury at the cervical level:
- Upper extremity immobilisation
- Upper extremity reduction in the range of motion in the acute phase
- Muscle shortening and shoulder capsule tightness
- Impaired muscle strength from weakness
- Spasticity
"Pain in the upper extremities of SCI patients is an incapacitating condition."[5] It interferes with all patient activities, including transfer skills, pressure relief and wheelchair mobility. Prevention and early management of upper limb pain in persons with tetraplegia should be addressed at every stage of rehabilitation.
The following are examples of therapeutic interventions that aim to reduce upper limb pain:[5]
- Increasing patient / caregiver knowledge of upper limb biomechanics
- Implementing appropriate daily life activity techniques, including wheelchair propulsion
- Avoiding overuse and weight-bearing through the upper limbs
- Designing a balanced muscle fitness programme for the upper extremity
- Establishing a nutritional orientation with a weight control focus
- Postural optimisation in the appropriate wheelchair
- Evaluating indications for adaptive devices and environmental changes
Assisting with Function[edit | edit source]
Tenodesis Grasp[7][edit | edit source]
- Requires contracture in flexor pollicis longus and the extrinsic finger flexor muscles
- Active wrist extension passively pulls the fingers and thumb into flexion
- Objects can be passively held between the thumb and index finger or in the palm
Methods to encourage/develop a good tenodesis grasp[2]
- Perform passive range of motion (PROM) exercises daily
- Proper sequence of PROM includes the wrist down (flexed) when fingers are opened (extended); fingers closed (flexed) when wrist comes up (extends)
- Reach and preserve mild tension in the long finger flexors without overstretching or shortening the flexors
- Maintain the webspace
- A thumb opponens splint (see below) may be prescribed to increase tenodesis grasp as it helps to maintain proper thumb position
Tenodesis splint: an orthotic device that spinal cord injury patients can wear over their hand and forearm. It helps guide grasp and release movements, providing the extra support individuals may need to perform tasks independently.
C7 Tetraplegia[edit | edit source]
- Innervated upper limb muscles in C7 spinal cord injury
- All muscles at the C6 level
- Pectoralis (sternal head)
- Triceps
- Pronator teres
- Flexor carpi radialis (wrist flexor)
- Extensor digitorum communis (finger extensor)
- Weak fingers and/or thumb extension may be present
- No finger or thumb flexion
- Functional impact
Goals for upper limb management:
- To prevent secondary complications of the upper limb, including the development of contractures and deformities.[3]
- To assist with function: e.g. optimise independence with ADLs, including eating, dressing, meal preparation, grooming, bladder and bowel programme[4]
- To gain community integration through independent transfers without a sliding board[9] and independent wheelchair propulsion[3]
C8 Tetraplegia[edit | edit source]
- Innervated upper limb muscles in C8 spinal cord injury
- All muscles at the C7 level
- Ulnar wrist extensor
- Finger flexors
- Thumb flexors
- May have finger and/or thumb flexors
- No intrinsics
- No thumb abduction
- Functional impact:
Goals for upper limb management:
- To prevent secondary complications of the upper limb, including the development of contractures and deformities.[3]
- To assist with function: optimise independence with ADLs, including eating, dressing, meal preparation, grooming, bladder and bowel programme.[4]
- To gain community integration through independent transfers without a sliding board, advanced wheelchair skills, and driving with adaptations.[9]
Incomplete Spinal Cord Injury[edit | edit source]
The term "incomplete spinal cord injury" is used when there is "preservation of any sensory and/or motor function below the neurological level that includes the lowest sacral segments S4–5 (i.e., presence of “sacral sparing”)."[11]
Goals for upper limb management
- Prevent complications
- Improve function
General Guidelines for upper limb management in incomplete spinal cord injury[2]
- Complete a comprehensive baseline assessment
- Individual muscle testing
- Movement analysis for detection of compensatory strategies
- Continuously assess and reassess to align treatment aims with strategies
Treatment strategies for upper limb management[2]
- Upper limb positioning
- Early out-of-bed mobilisation
- Activities in an upright position using a tilt table or standing frame
- Stimulation a more normal movement pattern: therapist-directed activities, hand-over-hand guidance
Central Cord Syndrome[edit | edit source]
"Central cord syndrome is the most common of the clinical syndromes, often seen in individuals with underlying cervical spondylosis who sustain a hyperextension injury (most commonly from a fall), and may occur with or without fracture and dislocations. This clinically will present as an incomplete injury with greater weakness in the upper limbs than in the lower limbs."[11]
Pathophysiology
- Forward fall with striking the chin and the neck extending backwards
- High velocity of trauma
- Cervical spine subluxation
- Cervical spine fracture
Symptoms [12]
- Significant strength impairments in the upper and lower extremities, the upper greater than the lower
- Sensory deficits below the level of injury (frequent, but not always)
- Pain and temperature sensations are typically affected
- Light touch sensation impaired
- "Cape-like" sensory impairment across the upper back and down the posterior upper extremities
- Neck pain at the site of spinal cord impingement
- Upper and lower limbs increased muscle tone, and spasticity[2]
- Shoulder pain and/or shoulder subluxation [2]
- Hand oedema [2]
- Joint contractures of the upper limbs[2]
Treatment strategies for upper limb management[2]
- Varies based on the level of injury - e.g., with central cord syndrome at the level of C5, poor proximal stability at the shoulder and the elbow must be addressed
- Spasticity management
- Upper limb pain management
- Upper limb positioning strategies in sitting, standing and during ambulation
Upper Limb Splinting[edit | edit source]
Short opponens
- Almost exclusively custom-made
- Facilitates tenodesis by opposing the thumb and preventing thumb overstretching during functional tasks
- Worn as needed to increase function
- Facilitates tenodesis for individuals with wrist extension 3-5/5 and digits 0-2/5
- Recommended for individuals with C6, C7-8 SCI
Wrist splint (Futuro splint):
- Prefabricated wrist splints are preferred
- Worn during the day to increase functional activity participation
- Dorsal varieties and a U-Cuff are preferred options
- The primary goal of a wrist splint is to prevent overstretching of the wrist extensors; adding a universal cuff provides a stable base for ADLs
- Clinical Practice Guidelines: for daytime use for individuals with elbow flexion 3-5/5, and wrist and hand 0-3/5
- Most commonly used in a C5 SCI (73% of patients) and C4 (40% of patients)
Metacarpophalangeal (MCP) blocking splint
- Custom-made splint
- Prevents hyperextension deformity of the MCP joints
- Prevents MCP hyperextension during functional hand tasks
- Recommended for patients with C7, C8 spinal cord injury if intrinsic hand weakness is present
More information on upper limb splinting in tetraplegia is available here.
Exercise Therapy[edit | edit source]
Strengthening Exercises[edit | edit source]
According to the literature,[13][14] [15] strengthening exercises such as arm ergometry, resistance training, the use of mobile arm supports, or virtual reality improves the overall performance of functional daily activities in individuals with a spinal cord injury. Exercise therapy effectively improves functional outcomes in patients with tetraplegia when conducted according to the following three training principles.
Three principles of training:[13]
- Overload (the most important)
- System or tissue must be challenged with the intensity, duration and frequency of exercise
- The outcome depends on the patient's motivation and feedback received (augmented feedback[16]), and structure of practice (task specificity and goal-orientated practice)
- Specificity
- The training effect is limited to the system and tissues involved in the activity
- Reversibility
- Gains are quickly lost when the overload is removed
Examples of exercise therapy applied in therapy programmes for patients with tetraplegia:[13]
- Virtual Reality: offers repetitive practice, feedback about performance and motivation[17]
- Use of robotics to increase therapy intensity
Functional Passive Range of Motion (FPROM)[edit | edit source]
Patients with lower tetraplegia present with:[18]
- Limitations in forearm pronation
- Limitations in elbow extension or elbow hyperextension - elbow hyperextension was present in one-third of patients participating in the study[18]
- Increased shoulder extension
- Increased wrist extension
According to research,[18] shoulder horizontal adduction and elbow extension were associated with functional performance.
The goal of FPROM:
- To develop long-term plans for passive range of motion exercises to optimise functional abilities
Resources[edit | edit source]
- Web-based teaching and educational resource for medical and paramedical professionals involved in SCI Management: https://www.elearnsci.org/pages.aspx?id=16&page=Who_are_we
- International Standards for Neurological Classification of Spinal Cord Injury: Revised 2019
References[edit | edit source]
- ↑ 1.0 1.1 Bersch I, Krebs J, Fridén J. A Prediction Model for Various Treatment Pathways of Upper Extremity in Tetraplegia. Front Rehabil Sci. 2022 Jun 30;3:889577.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Oelofse W. Upper Limb Management in Lower Tetraplegia - Occupational Therapy Course. Plus 2022
- ↑ 3.0 3.1 3.2 3.3 3.4 Arsh A, Anwar Z, Zeb A, Ilyas SM. Effectiveness of occupational therapy in improving activities of daily living performance in complete cervical tetraplegic patients; A quasi-experimental study. Pak J Med Sci. 2020 Jan-Feb;36(2):96-99.
- ↑ 4.0 4.1 4.2 4.3 Yarkony GM, Roth EJ, Heinemann AW, Lovell L. Rehabilitation outcomes in C6 tetraplegia. Paraplegia. 1988 Jun;26(3):177-85.
- ↑ 5.0 5.1 5.2 5.3 5.4 Barbetta DC, Lopes AC, Chagas FN, Soares PT, Casaro FM, Poletto MF, de Carvalho Paiva Ribeiro YH, Ogashawara TO. Predictors of musculoskeletal pain in the upper extremities of individuals with spinal cord injury. Spinal Cord. 2016 Feb;54(2):145-9.
- ↑ Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, Part I: Epidemiology, aetiology, and pathomechanics. J Spinal Cord Med. 2004;27(1):4-17.
- ↑ Harvey LA, Herbert RD. Muscle stretching for treatment and prevention of contracture in people with spinal cord injury. Spinal Cord. 2002 Jan;40(1):1-9.
- ↑ AmputeeOT: What is a tenodesis splint?Available from: https://www.youtube.com/watch?v=T_cFWDum3KU [last accessed 28/11/2022]
- ↑ 9.0 9.1 Rodríguez-Mendoza B, Santiago-Tovar PA, Guerrero-Godinez MA, García-Vences E. Rehabilitation Therapies in Spinal Cord Injury Patients. Paraplegia. 2020 Jun 17.
- ↑ 10.0 10.1 Suszek-Corradetti M. Rehabilitation path for patients with spinal cord injury from critical condition to optimal independence in everyday life on the example of the activities of the Montecatone Rehabilitation Institute in Italy. Archives of Physiotherapy & Global Researches. 2020 Jul 1;24(2).
- ↑ 11.0 11.1 Rupp R, Biering-Sørensen F, Burns SP, Graves DE, Guest J, Jones L, Read MS, Rodriguez GM, Schuld C, Tansey-Md KE, Walden K. International standards for neurological classification of spinal cord injury: revised 2019. Topics in spinal cord injury rehabilitation. 2021;27(2):1-22.
- ↑ Ameer MA, Tessler J, Munakomi S, Gillis C. Central cord syndrome. StatPearls. 2022 Nov 16.
- ↑ 13.0 13.1 13.2 Kloosterman MG, Snoek GJ, Jannink MJ. Systematic review of the effects of exercise therapy on the upper extremity of patients with spinal cord injury. Spinal Cord. 2009 Mar;47(3):196-203.
- ↑ Atkins MS, Baumgarten JM, Yasuda YL, Adkins R, Waters RL, Leung P, Requejo P. Mobile arm supports: evidence-based benefits and criteria for use. J Spinal Cord Med. 2008;31(4):388-93.
- ↑ DiCarlo SE. Effect of arm ergometry training on wheelchair propulsion endurance of individuals with quadriplegia. Phys Ther. 1988 Jan;68(1):40-4.
- ↑ van Dijk H, Jannink MJ, Hermens HJ. Effect of augmented feedback on motor function of the affected upper extremity in rehabilitation patients: a systematic review of randomized controlled trials. J Rehabil Med. 2005 Jul;37(4):202-11.
- ↑ Palaniappan SM, Suresh S, Haddad JM, Duerstock BS. Adaptive Virtual Reality Exergame for Individualized Rehabilitation for Persons with Spinal Cord Injury. In European Conference on Computer Vision 2020 Aug 23 (pp. 518-535). Springer, Cham.
- ↑ 18.0 18.1 18.2 Frye SK, Geigle PR, York HS, Sweatman WM. Functional passive range of motion of individuals with chronic cervical spinal cord injury. The Journal of Spinal Cord Medicine. 2020 Mar 3;43(2):257-63.