Upper Limb Considerations: Difference between revisions
No edit summary |
Anas Mohamed (talk | contribs) No edit summary |
||
| (45 intermediate revisions by 7 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- [[User:Mary-Jane Cole|Mary-Jane Cole]] and [[User:Joy Rendell|Joy Rendell]] as part of the [[World Physiotherapy Network for Amputee Rehabilitation Project]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Amputation of the upper limb (UL) involves the loss of the hand and this can be especially challenging. The effect upon the person can be devastating often with an inability to perform the simplest of functional activities | Amputation of the upper limb (UL) involves the loss of the hand and this can be especially challenging. The effect upon the person can be devastating often with an inability to perform the simplest of functional activities<ref>Atkins, D. J. Prosthetic Training. In: Smith, D, G., Michael, J.W and J. H. Bowker. Editors, 2004, Atlas of Amputations and Limb Deficiencies. 3rd Ed. American Acadamy of Orthopaedic Surgeons</ref> . | ||
This chapter aims to provide some considerations for the physiotherapist in the management of the person with acquired limb loss (versus congenital loss). Traditionally the Occupational Therapist leads prosthetic therapy for the upper limb amputee. However, physiotherapy is indicated in many rehabilitation phases from assessment pre-amputation and post amputation, to pre-prosthetic rehabilitation and the management of problems associated with UL loss e.g. pain, overuse injuries and postural and gait deviations. | This chapter aims to provide some considerations for the physiotherapist in the management of the person with acquired limb loss (versus congenital loss). Traditionally the Occupational Therapist leads prosthetic therapy for the upper limb amputee. However, physiotherapy is indicated in many rehabilitation phases from assessment pre-amputation and post amputation, to pre-prosthetic rehabilitation and the management of problems associated with UL loss e.g. pain, overuse injuries and postural and gait deviations. | ||
| Line 30: | Line 26: | ||
Before considering the specifics of physiotherapy and the UL amputee it is important to remember the anatomy of the UL and to appreciate the purpose and function of the UL. | Before considering the specifics of physiotherapy and the UL amputee it is important to remember the anatomy of the UL and to appreciate the purpose and function of the UL. | ||
== Clinically relevant anatomy == | |||
===Muscles of the Upper Arm and Shoulder Blade=== | |||
===Shoulder girdle– [[Shoulder#Anatomy|shoulder gridle anatomy pages]] === | |||
{{#ev:youtube|5bneylG3w10}} | |||
===Glenohumeral joint- [[Glenohumeral Joint|glenohumeral joint page]] === | |||
{{#ev:youtube|vG1XQkj3Yx0}} | |||
===Elbow – [[Elbow|elbow pages]] === | |||
{{#ev:youtube|S1Jo3Asc68g}} | |||
===Wrist and fingers – [[Wrist and Hand|wrist and hand pages]] === | |||
{{#ev:youtube|uiyqVsSPD1w}} | |||
'''Purpose and function of arm and hand i.e. prehensile and non prehensile activities, expression and culture''' | '''Purpose and function of arm and hand i.e. prehensile and non prehensile activities, expression and culture''' | ||
| Line 75: | Line 82: | ||
==== Culture ==== | ==== Culture ==== | ||
*Hand use and specific gestures take on considerable significance in certain cultures. The most common popular belief about hands, for instance in Hindu, Islam, and some African cultures, is to consider the left hand as “unclean” and reserved solely for “hygienic” reasons, while it is thought culturally imperative to use the right hand for offering, receiving, eating, for pointing at something or when gesticulating | *Hand use and specific gestures take on considerable significance in certain cultures. The most common popular belief about hands, for instance in Hindu, Islam, and some African cultures, is to consider the left hand as “unclean” and reserved solely for “hygienic” reasons, while it is thought culturally imperative to use the right hand for offering, receiving, eating, for pointing at something or when gesticulating <ref name="who2009">World Health Organization. 2009. [http://www.ncbi.nlm.nih.gov/books/NBK143998/ WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care].</ref>. In the Sikh and Hindu cultures, a specific cultural meaning is given to the habit of folding hands together either as a form of greeting, as well as in prayer<ref name="who2009" />. | ||
*Hand washing is also closely connected with religious practice in the Islamic faith in particular. | *Hand washing is also closely connected with religious practice in the Islamic faith in particular. | ||
*Causes of amputation such as punishment for theft, or occurred as a war injury can incur an additional stigma and psychological issues. | *Causes of amputation such as punishment for theft, or occurred as a war injury can incur an additional stigma and psychological issues. | ||
*Products and services are generally designed assuming two-handed and right-handed users. | *Products and services are generally designed assuming two-handed and right-handed users. | ||
==Causes and incidence of upper limb amputation (United Kingdom)<ref name="NASDAB">The Amputee Statistical Database for the United Kingdom 2004/05. Information Services Division | |||
NHS Scotland on behalf of National Amputee Statistical Database (NASDAB)</ref>. == | |||
(NB University of Salford now holds more recent UK statistics but reports available at cost only). | |||
The most common cause of amputation in the UL amputee is trauma. Amputation may happen as part of the trauma itself. In some cases where limb salvage and reconstructive surgery has not achieved a successful outcome, elective amputation may be performed e.g. where trauma is associated with a totally avulsed brachial plexus, amputation may be a choice where the arm remains flail and insensate. | The most common cause of amputation in the UL amputee is trauma. Amputation may happen as part of the trauma itself. In some cases where limb salvage and reconstructive surgery has not achieved a successful outcome, elective amputation may be performed e.g. where trauma is associated with a totally avulsed brachial plexus, amputation may be a choice where the arm remains flail and insensate. | ||
| Line 96: | Line 106: | ||
*<1% No cause provided | *<1% No cause provided | ||
However, in middle and low income countries the incidence of traumatic UL amputation is higher | However, in middle and low income countries the incidence of traumatic UL amputation is higher.<br>The figures below reflect the total numbers recorded of acquired UL loss in the UK in the year 2004-2005 | ||
*Total no. new referrals to UK prosthetic centres = 280 | *Total no. new referrals to UK prosthetic centres = 280 | ||
| Line 105: | Line 115: | ||
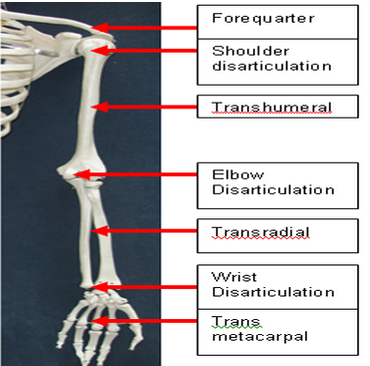
== Levels of amputation == | == Levels of amputation == | ||
[[Image:Levels-of-amputation-upper-limb.png|Levels of amputation - upper limb]]<br> | |||
== Limb salvage and assessment – considerations == | |||
*[[Assessment of the amputee|Assessment principles]] – pre and post-amputation – will align with those of the LL amputee | |||
*In cases of trauma where there is no amputation as a consequence of the trauma, the MESS<ref name="mess">Mangled extremity severity score (MESS) (Johnson et al 1990) http://www.mdcalc.com/mangled-extremity-severity-score-mess-score/</ref> or TRISS <ref>Trauma Score and the Injury Severity Score (TRISS) (Boyd et al1987) http://www.trauma.org/index.php/main/article/387/</ref> scoring will be applied to assess potential for successful reconstruction of the limb. | |||
**[http://www.mdcalc.com/mangled-extremity-severity-score-mess-score/ Mangled extremity severity score (MESS)] | |||
**[http://www.trauma.org/index.php/main/article/387/ Trauma Score and the Injury Severity Score (TRISS)] | |||
*Where limb salvage and reconstruction is not indicated a thorough pre-amputation assessment should be performed | *Where limb salvage and reconstruction is not indicated a thorough pre-amputation assessment should be performed | ||
*Assessment may take place in cases where limb salvage has not succeeded in restoring a functional extremity and an elective amputation is to be performed; or in the case of a peripheral nerve injury where nerve recovery is insufficient and the arm is insensate and functionless | *Assessment may take place in cases where limb salvage has not succeeded in restoring a functional extremity and an elective amputation is to be performed; or in the case of a peripheral nerve injury where nerve recovery is insufficient and the arm is insensate and functionless | ||
*An MDT approach to decision making and preparation for amputation is recommended as with the LL amputee | *An MDT approach to decision making and preparation for amputation is recommended as with the LL amputee<ref>Broomhead P, Dawes D, Hancock A, Unia P, Blundell A, Davies V. 2006. [http://bacpar.csp.org.uk/publications/clinical-guidelines-pre-post-operativephysiotherapy-management-adults-lower-li Clinical guidelines for the pre and post operative physiotherapy management of adults with lower limb amputation]. Chartered Society of Physiotherapy, London</ref>. | ||
*It can be helpful for the person and the MDT in terms of agreeing goals of treatment if the OT and Physiotherapy can jointly assess | *It can be helpful for the person and the MDT in terms of agreeing goals of treatment if the OT and Physiotherapy can jointly assess | ||
*Associated injuries in relation to cause of amputation or potential amputation must be assessed and may require additional specialist expertise e.g. peripheral nerve injury | *Associated injuries in relation to cause of amputation or potential amputation must be assessed and may require additional specialist expertise e.g. peripheral nerve injury | ||
**Peripheral nerve injury – traumatic injury of the UL can be associated with PNI | **Peripheral nerve injury – traumatic injury of the UL can be associated with PNI | ||
**Assessment will include the use of EMG to identify and classify the extent and type of nerve damage e.g. neurapraxia, axonotmesis, and neurotmesis (in order of increasing severity) | **Assessment will include the use of EMG to identify and classify the extent and type of nerve damage e.g. neurapraxia, axonotmesis, and neurotmesis (in order of increasing severity) | ||
**The extent of damage can influence the decision to avoid amputation, amputate early or defer e.g. in case of brachial plexus injury, amputation surgery may be delayed for up to 2 years to determine full nerve recovery and functional return | **The extent of damage can influence the decision to avoid amputation, amputate early or defer e.g. in case of brachial plexus injury, amputation surgery may be delayed for up to 2 years to determine full nerve recovery and functional return<ref>Shin, A, Y., Bishop, Al T and J. W. Michael. 2004. Brachial Plexus Injuries: Surgical and Prosthetic Management. In: Smith, D, G., Michael, J.W and J. H. Bowker. Editors, Atlas of Amputations and Limb Deficiencies. 3rd Ed. American Acadamy of Orthopaedic Surgeons</ref>. | ||
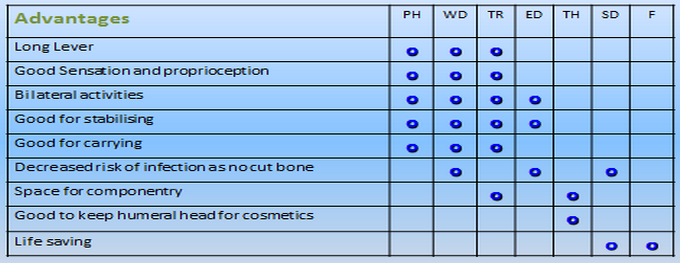
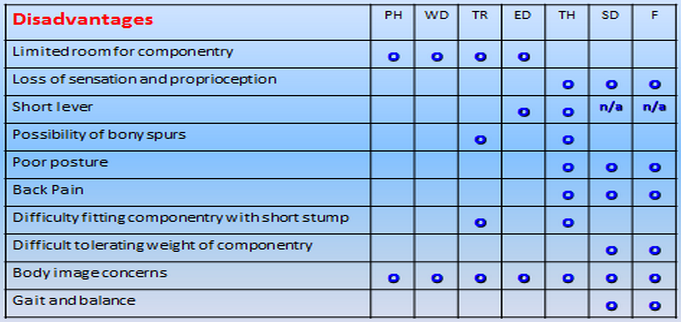
== Advantages and disadvantages of different levels of amputation == | |||
The tables below provide a broad overview of the advantages and disadvantages of the different levels of amputation including partial hand amputation (PH). | The tables below provide a broad overview of the advantages and disadvantages of the different levels of amputation including partial hand amputation (PH). | ||
[[Image:Advantages-upper-limb-amputation-levels.png]] | |||
Table 1 | |||
[[Image:Disadvantages-upper-limb-amputation-levels.png]] | |||
Table 2 | Table 2 | ||
Subjective assessment | == Subjective assessment == | ||
=== History of present condition === | |||
*Nature of injury or pathology and reason for amputation e.g. trauma, tumour, congenital deformity, infection | |||
*Current and past functional ability e.g. self-care, mobility, activities of daily living | |||
*Co-morbidities and concurrent pathologies/ injuries associated e.g. multiple limb loss, PNI | |||
*History of investigations/ surgery prior to amputation | |||
=== Past and relevant medical history === | |||
*Osteoarthritis and Rheumatoid Arthritis– limitations of movement, pain or weakness; remaining hand function will be important for performing PADL and ADL | |||
*THREAD (Thyroid disorders, Heart problems, Rheumatoid arthritis, Epilepsy, Asthma or other respiratory problems, Diabetes) | |||
*Cardiac history / exercise tolerance | |||
*Smoking/ alcohol history | |||
*Vision and hearing | |||
=== Pain === | |||
*Pattern of pain in affected arm | |||
*Pain elsewhere e.g. associated trauma, co-morbidities, remaining arm | |||
*Residual limb pain and/ or phantom limb pain will influence participation in rehab and independence with functional activities and prosthetic use | |||
*A common cause of pain in the remaining arm is through overuse | |||
=== Drug history === | |||
*Pain relief | |||
*Other | |||
=== Psychosocial factors === | |||
*Social support i.e. family members, neighbours, community | |||
*Social participation prior to amputation | |||
*Home e.g. accommodation, flat, house, stairs | |||
*Occupation, school, study | |||
*Interests and hobbies | |||
*Driving and transport | |||
*If the UL loss is associated with an accident, were others injured, RIP? | |||
*Cognition | |||
*Mood/ motivation/ mental health status, presentation e.g. posture, willingness to engage with history taking and assessment process, reaction towards prospective amputation or amputation | |||
**The hand is a significant factor in body image, personality, independence and livelihood<ref>Carnegie F. 1999. Upper limb amputation and congenital limb deficiency. In Therapy for Amputees. Engstrom B and Van de Ven C. Churchill</ref> | |||
**The loss of an arm can have considerable psychological consequences | |||
*8The cultural impact of upper limb loss may have a profound effect on a person’s independence, participation and status within a society | |||
*8Children as they become older, will be increasingly aware of their disability and are susceptible to psychological difficulties e.g. body image, participation physically and socially. Parents and families also require support. Establishing links early with family support services and prosthetic services – with the opportunity to meet peers of a similar age with limb loss – is highly recommended | |||
**Sense of loss, bereavement for the limb and life as they knew it before. | |||
**The 5 stages are denial and isolation, anger, bargaining, depression and acceptance | |||
== Objective assessment == | |||
=== Range of movement and muscle strength === | |||
*Cervical and thoracic spine, the shoulder girdle and all joints proximal to amputation level in both arms | |||
**Restricted movement and muscle strength can limit function and predispose to postural and gait deviations | |||
**In the bilateral UL amputee the neck, hips, knees and feet will be used in ADLs and PADLs | |||
*Soft tissue – intact skin cover, sensation, scarring, burns | |||
*ROM, muscle strength of remaining arm | |||
**E.g. manual dexterity of the ‘sound’ is critical as it will become dominant | |||
=== Balance, posture and gait === | |||
*In sitting, standing, walking and turning | |||
*Postural asymmetry e.g. reduced muscle bulk, tone, scapular elevation, retraction | |||
**Restricted balance and proprioception can limit function and predispose to postural and gait deviations; the impact of bilateral UL loss on balance should not be underestimated | |||
**The most common postural deviation observed in the UL amputee is scapular elevation and protraction, internal rotation and adduction of the gleno-humeral joint, restricted cervical rotation and side flexion , kyphotic posture with pocking chin (see figure 2) | |||
**In walking arm swing can be reduced and accompanied by thoracic side flexion to the amputated side | |||
[[Image:Upper-limb-amputee-posture.jpg]] | |||
'''Figure 2''' | |||
Hand dominance, function and testing of ADLs | === Hand dominance, function and testing of ADLs === | ||
*PADL and ADL | |||
**In the case of the single UL amputee the remaining arm will become the dominant arm | |||
**Dexterity and ability of the remaining arm to perform functional tasks and personal activities of daily living | |||
**Ability of the lower limbs to assist in functional activities | |||
== Considerations for pre-operative physiotherapy (where possible) == | |||
*Explore the opportunity to meet with another with the same level to inform, demonstrate and reassure. As with the LL amputee, source local prosthetic centres or national organisations ([http://www.limbless-association.org/ Limbless Association]) | |||
*Where possible, an appointment to be seen and assessed by a specialist prosthetic MDT at a regional rehabilitation centre can provide the opportunity to meet with an other UL amputee/s, to see and gain facts about appropriate prostheses and prosthetic use | |||
*Otherwise, early liaison with prosthetic centre to gain advice. Be cautious with patient expectations of prosthetic use | |||
*Discuss pain relief and potential for pain post operatively, phantom limb sensation (PLS) and phantom limb pain (PLP) | |||
*Plan pre and postoperative physiotherapy intervention through agreeing realistic short term goals | |||
*Situation permitting, maintain and/ or increase proximal joint ROM and muscle strength both arms | |||
*In anticipation of transhumeral prosthetic use incorporate scapular movement e.g. protraction and retraction | |||
*Introduce functional activities in the ‘dominant’ arm and lower limbs | |||
*Advice on posture, teach and correct | |||
*Concurrent treatment | |||
== Post amputation and pre-prosthetic rehabilitation == | |||
Assessment post amputation should include information about the quality of the residual limb/ residuum (stump) as this will have an impact on the prosthetic rehabilitation potential for the patient | |||
*Wound condition | |||
*Oedema | |||
*Residual limb length | |||
*Soft tissue cover | |||
*Cut end of bone (prominent or not) | |||
*Shape | |||
*Sensation | |||
*Position of suture line, adherence | |||
*Pain | |||
The principles of wound care, oedema control, pain management will align to that of the LL. Similarly, emotional support, goal planning. Where possible there should be close working with the OT | |||
*Oedema control | |||
**Elevation e.g. at rest on a pillow with the distal end at a higher level than the shoulder; supported via a drip stand when walking | |||
**Compression via compression shrinker sock or elastic bandage | |||
**Active exercises | |||
*[[Pain Management of the Amputee|Pain management]] | |||
**Encourage residual limb handling & desensitising – this can help adjustment to changed body image | |||
**Note that phantom limb sensation and pain can be more common in the UL; consider the relative representation of the hand on the homunculus and proximity to the face. PLP experienced by the UL amputee can be associated with facial sensations | |||
*Emotional support | |||
**MDT approach, onward referral for specialist support e.g. clinical psychologist, counsellor | |||
*Patient and family /carer – as above | |||
*Discuss lifestyle, employment, hobbies and home situation | |||
*Discuss expectations of prosthesis | |||
*Agree goals for treatment | |||
=== Physiotherapy specific === | |||
*Postural advice in sitting, standing and walking | |||
*Maintain and > proximal joint ROM & strength | |||
**Encourage early active movement of all proximal joints from 1st day post amputation | |||
**Resisted exercise as soon as pain allows | |||
**Active ROM Cx and Tx spine | |||
*GH joint – flex/ ext; abd/ add; ext rot/ int rot | |||
**Scapula – depression/ elevation; protraction/ retraction | |||
***GH and scapula rhythm – NB protraction and flexion principle movement required for a body powered prosthesis | |||
**Elbow – flex/ ext, pron/ sup | |||
*Physiotherapy treatment techniques include | |||
**Mobilisations, stretches (see figure 3), auto resisted exercises, theraband | |||
[[Image:Upper-limb-amputee-fig3.jpg]] | |||
'''Figure 3''' | |||
**Base on normal movement e.g. reach and grasp, PNF (see Figure 4) | |||
[[Image:Upper-limb-amputee-fig4.jpg]]<br> | |||
'''Figure 4''' | |||
*Proprioception for shoulder e.g. stabilisation exercises, 4 point kneeling, wobble cushion, ball | |||
Figure | *Normalisation of residual limb sensation e.g. handling, exercises, loading (see Figure 5) | ||
[[Image:Upper-limb-amputee-fig5.jpg|Figure 5]]<br> | |||
'''Figure 5''' | |||
*Pilates & core stability | |||
*Exercise leaflets e.g. core stability | |||
*Incorporate prosthetic use into functional exercises at later stage based on normal movement (see figure 6) | |||
[[Image:Upper-limb-amputee-fig6.jpg]]<br> | |||
'''Figure 6''' | |||
*Apply ergonomics e.g. car, work station, sleep posture (see figure 7) | |||
[[Image:Upper-limb-amputee-fig7.jpg]]<br> | |||
'''Figure 7''' | |||
*Encourage to use residual limb as much as possible with PADLs and ADLs | |||
*Use simple gauntlet to hold utensils, comb, toothbrush (see figure 8) | |||
<br> | [[Image:Upper-limb-amputee-fig8.jpg]]<br> | ||
'''Figure 8''' | |||
*Encourage symmetry of movement | |||
**Avoid one handedness i.e. of remaining arm | |||
*Balance, gait and posture | |||
**Walk, run, turn | |||
**Encourage arm swing and trunk rotation | |||
*Education and advice on prevention of problems e.g. of not moving or overuse | |||
**Stiff, shoulder pain, Cx & Tx pain, tenosynovitis. See below | |||
**Functional limitations e.g. unable to wash axilla/ apply deodorant | |||
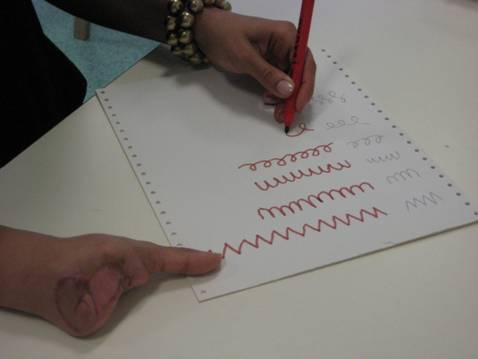
*Exercises for the dominant hand | |||
**Hand mobility | |||
**Writing (see figure 9) | |||
**Dressing | |||
[[Image:Upper-limb-amputee-fig9.jpg]]<br> | |||
'''Figure 9''' | |||
*Mobility, balance and functional activities for the bilateral UL amputee (see figures 10, 11) | |||
[[Image:Upper-limb-amputee-fig10.jpg]]<br> | |||
'''Figure 10''' | |||
[[Image:Upper-limb-amputee-fig11.png]]<br> | |||
'''Figure 11''' | |||
== Considerations for prosthetic rehabilitation == | |||
Motivation is essential if patients are planning to use a prosthesis. Amputees with lower limb loss often choose to wear prostheses but those with UL loss often don’t use prosthetic arms, especially children. Developing skills with a prosthesis is a bit like learning to ride a bike, once learnt it is easy to use later. <br>It is advisable to encourage amputees to learn to use a prosthesis early and put in the time practise time required to be proficient. Once patients have found a way to do something and have adjusted to being without a hand there is less tendency to adapt to using a prosthesis. <br>Early prosthetic use is recommended; amputees are more likely to adapt with the risks of becoming one handed and with less motivation to use a prosthesis. <br>Early referral for prosthesis and rehabilitation is advised. | |||
*Seek out what the patient’s goal is | |||
*Identify the potential of the prosthesis that the client is due to receive, or is available, as it is and what could be added | |||
*Enabling the patient to put on and take off the prosthesis at will | |||
*Making sure that the fit of the prosthesis is not going to create harm by chaffing or pressing on hypersensitive locations. Check the skin before and after each session and teach the patient to know what to look for | |||
*That they can put clothes over the prosthesis easily. The prosthesis may not assist with putting on undergarments, but can assist with larger garments | |||
*Enable the patient to know how far they can reach, when wearing the prosthesis and still operate it. That they know where the prosthesis ends For example to enable patient to move around a crowded environment without knocking things in error | |||
*To be able to grasp and release a variety of objects at will, and with confidence | |||
*To be able to maintain a grasp while doing other activities eg walking around or talking. This sustained grip is ideally relaxed posture rather than global tension | |||
*Where there is a change in hand dominance it is necessary to do repetitive practice to develop ease of movement | |||
*Ultimately the prosthesis assumes the role of a tool and they are able to focus on the task and expression that they are engaged in. They are able to relate to other people on the basis of chosen activities and not that the prosthesis dominates their awareness | |||
=== Common physical problems associated with UL loss – considerations and potential management strategies === | |||
#Injury, repetitive strain/ overuse in the remaining arm e.g. shoulder impingement, tenosynovitis, epicondylitis, Carpal Tunnel Syndrome<br> | |||
#*Increased risk in certain non amputee populations e.g. typists | |||
#*Altered biomechanics and posture due to amputation | |||
#*Favour and stress intact arm | |||
#*Minimal research evidence of overuse/ repetitive strain injuries in UL amputees<ref name="Jones">Jones, L,E and J,H Davidson. 1999. Save that arm: a study of problems in the remaining arm of unilateral upper limb amputees. Prosthetics and Orthotics International. 23:55-58</ref><ref name="Gambrell">Gambrell, C. 2008. Overuse Syndrome and the Unilateral Upper Limb Amputee: Consequences and Prevention. Journal of Prosthetics & Orthotics. 20:126-132</ref><ref name="Biden">Biden, E., L. Manor., G. Bush and W.L Hill. 2015. Repetitive Strain Injury Risk Factors in Upper Limb Amputees. ISPO World Congress Lyon, France. 2015</ref> | |||
#*Problems more prevalent in proximal amputations | |||
#*Prosthetic use or lack of employment not protective of remaining arm<ref name="Jones" /> | |||
#*No unilateral UL amputee is immune to developing overuse injury | |||
#*Risk factors include | |||
#**Repetition e.g. texting | |||
#**High force<br> | |||
#**Awkward joint posture | |||
#**Prolonged constrained posture | |||
#**Direct pressure | |||
#**Vibration | |||
#**Greater risk factors for wrist and hand with acquired amputation versus congenital | |||
#**Increased BMI | |||
#*Apply knowledge from other patient populations<ref name="Gambrell" /> to manage; utilise musculoskeletal and pain assessment approach | |||
#**Education on prevention of joint overuse, pacing, consider influence of posture on movement, encourage early use of residual limb to minimize one handedness with associated greater risk of overuse injury in remaining arm | |||
#**Recognise 3 stages of overuse syndrome<br>Stage 1 – Increased aching and tiredness during an activity that subsides with overnight rest – a warning symptom<br>Stage 2 – Discomfort into the next day with earlier fatigue – suggests injury is developing (reduce strain on affected tissues by minimising aggravating activities and prescribe frequent rests and/ or splinting e.g. carpal tunnel, thumb spica)<br>Stage 3 – Chronic fatigue, pain and weakness that persists despite rest – onset of fibrosis (complete rest via splinting, medical management e.g. steroid injection) | |||
#Neck & thoracic back pain (e.g. asymmetry of posture due to reduced weight on one side of body) | |||
#Tight anterior shoulder capsule, tight pectoral & anterior deltoid muscles e.g. established amputees/ persons with congenital loss with long term habits, protective and postural changes | |||
#Reduced glenohumeral range of movement | |||
#Poor glenohumeral / scapula rhythm | |||
#Weak rotator cuff i.e. subscapularis, infraspinatus, teres major & minor (inherently weaker > 60 years of age) | |||
#[[Phantom limb pain|Phantom pain]]. | |||
=== Prevention and management of common physical problems associated with UL loss includes === | |||
*Patient information and education as early as possible | |||
*Preventative measures e.g. avoid excessive loading and repetitive movements, manage posture | |||
*Adaptations to encourage function, bilateral arm use and symmetry of movement | |||
*Postural advice including ergonomics e.g. height of work stations | |||
*Mobilising, stretching and strengthening exercises including core | |||
*Facilitation of normal rhythmical movement | |||
*‘Pacing’ and appropriate goal setting | |||
*Self management of early symptoms e.g. rest | |||
*Thermal modalities | |||
*Ultrasound | |||
*Immobilisation via splinting e.g. carpal tunnel, thumb spica | |||
*NSAIDs | |||
*Steroid injections | |||
*Friction massage | |||
*Nerve blocks | |||
*Surgery e.g. carpal tunnel decompression, tendon repair | |||
*MDT responsibility – beware of focus on prosthetic rehab and forgetting reliance on remaining arm | |||
*Functioning prosthesis versus cosmetic prosthesis or no prosthesis may limit common physical problems<ref name="Sato">Sato et al. 1999. Carpal tunnel syndrome involving unaffected limbs of stroke patients. Stroke. 30:414-418</ref><ref name="Gambrell" /><br> | |||
=== Considerations for the child with UL amputation === | |||
Refer to the [http://www.reach.org.uk/ Association for Children with Upper Limb Deficiency] | |||
*Children with an UL amputation may experience additional problems and challenge in relation to the cause of amputation and/ or as they grow older e.g. musculoskeletal pathologies | |||
*Regular review is essential to assess and treat symptomatically<br> | |||
== Standards of practice == | |||
Refer to [http://www.irpag.org/PIRPAG PIRPAG (Physiotherapy Interregional Prosthetic Audit Group) recommendations] <br> | |||
{{pdf|RecommnedationsforPHYSIOTHERAPYUpperLimbAmputeeRoehampton2009.doc.pdf|Recommendations for practice from Roehampton Rehabilitation Centre}} | |||
<br> | <br> | ||
== References | == References == | ||
<references /> | <references /> | ||
[[Category:Amputees]] [[Category: | [[Category:Amputees]] | ||
[[Category:World Physiotherapy Amputee Project]] | |||
[[Category:Occupational Health]] | |||
Latest revision as of 13:17, 29 August 2020
Original Editor - Mary-Jane Cole and Joy Rendell as part of the World Physiotherapy Network for Amputee Rehabilitation Project
Top Contributors - Tony Lowe, Admin, Kim Jackson, Sheik Abdul Khadir, Amrita Patro, Anas Mohamed, Rachael Lowe and Joao Costa
Introduction[edit | edit source]
Amputation of the upper limb (UL) involves the loss of the hand and this can be especially challenging. The effect upon the person can be devastating often with an inability to perform the simplest of functional activities[1] .
This chapter aims to provide some considerations for the physiotherapist in the management of the person with acquired limb loss (versus congenital loss). Traditionally the Occupational Therapist leads prosthetic therapy for the upper limb amputee. However, physiotherapy is indicated in many rehabilitation phases from assessment pre-amputation and post amputation, to pre-prosthetic rehabilitation and the management of problems associated with UL loss e.g. pain, overuse injuries and postural and gait deviations.
Please note that prosthetic rehabilitation is normally beyond the scope of the physiotherapist’s role and this phase is not included.
Learning outcomes ….[edit | edit source]
- Anatomical knowledge of the upper limb
- Understand the functional purpose of the arm and hand
- Know the causes and levels of acquired UL amputation
- Be able to perform a subjective and objective assessment pre and post-amputation
- Be able to prepare a person for UL amputation
- Be able to treat an UL amputee post operatively and pre-prosthetically
- Appreciate the psychosocial needs of the UL amputee
- Appreciate the needs of the child with upper limb amputation
- Understand the physiotherapist’s role within the MDT and the roles of others
Before considering the specifics of physiotherapy and the UL amputee it is important to remember the anatomy of the UL and to appreciate the purpose and function of the UL.
Clinically relevant anatomy[edit | edit source]
Muscles of the Upper Arm and Shoulder Blade[edit | edit source]
Shoulder girdle– shoulder gridle anatomy pages[edit | edit source]
Glenohumeral joint- glenohumeral joint page[edit | edit source]
Elbow – elbow pages[edit | edit source]
Wrist and fingers – wrist and hand pages[edit | edit source]
Purpose and function of arm and hand i.e. prehensile and non prehensile activities, expression and culture
Our hands are unique and versatile and our arms are there to support and place them wherever they need to be. Hands are used to
- Stabilise
- Manipulate
- Discover (stereognosis)
- Express
Stabilise[edit | edit source]
- Hands are used in open or closed position to push objects away and to protect e.g. opening a door or pushing branches aside
- As a lever to lean on to stabilise ourselves for a task
- To arrange objects in our environment such as pushing and pulling objects around on a desk
- With our fingers to press switches and manage our electronic media. The length or our arm is significant here
Manipulate[edit | edit source]
- When manipulating objects bimanually one hand is static and the other is the active manipulator for example holding a box in one hand and opening the catch and the lid with the other
- The range of grasps we have within the hand utilise the different positions of the thumb
- there is the pinch and tripod grips for fine tasks
- key grip for thin flat objects
- power grip for grasping handle
- spherical grip for round objects. There are also combination of grips within the one hand e.g. using a computer mouse. Then there is the fluid movement of the hand through all these positions and the interweaving of both hands within the same activity
Discover (stereognosis)[edit | edit source]
- Discovery and exploration is to be able to know what is in the hand by grasping and releasing again and again, or by running a finger over the surface. E.g. putting you hand in a pocket and pulling out only the desired object
Expression[edit | edit source]
- Our arms and hands are an extension of our thoughts and feelings - to gesture as you speak, or rather not speak and merely gesture. To touch another is a gesture of concern or love
Culture[edit | edit source]
- Hand use and specific gestures take on considerable significance in certain cultures. The most common popular belief about hands, for instance in Hindu, Islam, and some African cultures, is to consider the left hand as “unclean” and reserved solely for “hygienic” reasons, while it is thought culturally imperative to use the right hand for offering, receiving, eating, for pointing at something or when gesticulating [2]. In the Sikh and Hindu cultures, a specific cultural meaning is given to the habit of folding hands together either as a form of greeting, as well as in prayer[2].
- Hand washing is also closely connected with religious practice in the Islamic faith in particular.
- Causes of amputation such as punishment for theft, or occurred as a war injury can incur an additional stigma and psychological issues.
- Products and services are generally designed assuming two-handed and right-handed users.
Causes and incidence of upper limb amputation (United Kingdom)[3].[edit | edit source]
(NB University of Salford now holds more recent UK statistics but reports available at cost only).
The most common cause of amputation in the UL amputee is trauma. Amputation may happen as part of the trauma itself. In some cases where limb salvage and reconstructive surgery has not achieved a successful outcome, elective amputation may be performed e.g. where trauma is associated with a totally avulsed brachial plexus, amputation may be a choice where the arm remains flail and insensate.
Persons with amputations as a result of infection (e.g. meningococcal septicaemia) may have multiple amputations involving the UL and LL.
In the UK, persons with UL amputation account for approximately 5% of the total UK amputee population. Unlike LL amputees, most UL amputees are in the younger age group reflecting the aetiology of the condition.
- 54% Trauma
- 14% Neoplasia
- 12% Dysvascularity
- 6% Infection
- 2% Neurological disorder
- 12% Other
- <1% No cause provided
However, in middle and low income countries the incidence of traumatic UL amputation is higher.
The figures below reflect the total numbers recorded of acquired UL loss in the UK in the year 2004-2005
- Total no. new referrals to UK prosthetic centres = 280
- Male (184):Female (95) (unspecified 1)
- 49 amputees >65 years were referred
- Bilateral UL amputees: 9
Levels of amputation[edit | edit source]
Limb salvage and assessment – considerations[edit | edit source]
- Assessment principles – pre and post-amputation – will align with those of the LL amputee
- In cases of trauma where there is no amputation as a consequence of the trauma, the MESS[4] or TRISS [5] scoring will be applied to assess potential for successful reconstruction of the limb.
- Where limb salvage and reconstruction is not indicated a thorough pre-amputation assessment should be performed
- Assessment may take place in cases where limb salvage has not succeeded in restoring a functional extremity and an elective amputation is to be performed; or in the case of a peripheral nerve injury where nerve recovery is insufficient and the arm is insensate and functionless
- An MDT approach to decision making and preparation for amputation is recommended as with the LL amputee[6].
- It can be helpful for the person and the MDT in terms of agreeing goals of treatment if the OT and Physiotherapy can jointly assess
- Associated injuries in relation to cause of amputation or potential amputation must be assessed and may require additional specialist expertise e.g. peripheral nerve injury
- Peripheral nerve injury – traumatic injury of the UL can be associated with PNI
- Assessment will include the use of EMG to identify and classify the extent and type of nerve damage e.g. neurapraxia, axonotmesis, and neurotmesis (in order of increasing severity)
- The extent of damage can influence the decision to avoid amputation, amputate early or defer e.g. in case of brachial plexus injury, amputation surgery may be delayed for up to 2 years to determine full nerve recovery and functional return[7].
Advantages and disadvantages of different levels of amputation[edit | edit source]
The tables below provide a broad overview of the advantages and disadvantages of the different levels of amputation including partial hand amputation (PH).
Table 1
Table 2
Subjective assessment[edit | edit source]
History of present condition[edit | edit source]
- Nature of injury or pathology and reason for amputation e.g. trauma, tumour, congenital deformity, infection
- Current and past functional ability e.g. self-care, mobility, activities of daily living
- Co-morbidities and concurrent pathologies/ injuries associated e.g. multiple limb loss, PNI
- History of investigations/ surgery prior to amputation
Past and relevant medical history[edit | edit source]
- Osteoarthritis and Rheumatoid Arthritis– limitations of movement, pain or weakness; remaining hand function will be important for performing PADL and ADL
- THREAD (Thyroid disorders, Heart problems, Rheumatoid arthritis, Epilepsy, Asthma or other respiratory problems, Diabetes)
- Cardiac history / exercise tolerance
- Smoking/ alcohol history
- Vision and hearing
Pain[edit | edit source]
- Pattern of pain in affected arm
- Pain elsewhere e.g. associated trauma, co-morbidities, remaining arm
- Residual limb pain and/ or phantom limb pain will influence participation in rehab and independence with functional activities and prosthetic use
- A common cause of pain in the remaining arm is through overuse
Drug history[edit | edit source]
- Pain relief
- Other
Psychosocial factors[edit | edit source]
- Social support i.e. family members, neighbours, community
- Social participation prior to amputation
- Home e.g. accommodation, flat, house, stairs
- Occupation, school, study
- Interests and hobbies
- Driving and transport
- If the UL loss is associated with an accident, were others injured, RIP?
- Cognition
- Mood/ motivation/ mental health status, presentation e.g. posture, willingness to engage with history taking and assessment process, reaction towards prospective amputation or amputation
- The hand is a significant factor in body image, personality, independence and livelihood[8]
- The loss of an arm can have considerable psychological consequences
- 8The cultural impact of upper limb loss may have a profound effect on a person’s independence, participation and status within a society
- 8Children as they become older, will be increasingly aware of their disability and are susceptible to psychological difficulties e.g. body image, participation physically and socially. Parents and families also require support. Establishing links early with family support services and prosthetic services – with the opportunity to meet peers of a similar age with limb loss – is highly recommended
- Sense of loss, bereavement for the limb and life as they knew it before.
- The 5 stages are denial and isolation, anger, bargaining, depression and acceptance
Objective assessment[edit | edit source]
Range of movement and muscle strength[edit | edit source]
- Cervical and thoracic spine, the shoulder girdle and all joints proximal to amputation level in both arms
- Restricted movement and muscle strength can limit function and predispose to postural and gait deviations
- In the bilateral UL amputee the neck, hips, knees and feet will be used in ADLs and PADLs
- Soft tissue – intact skin cover, sensation, scarring, burns
- ROM, muscle strength of remaining arm
- E.g. manual dexterity of the ‘sound’ is critical as it will become dominant
Balance, posture and gait[edit | edit source]
- In sitting, standing, walking and turning
- Postural asymmetry e.g. reduced muscle bulk, tone, scapular elevation, retraction
- Restricted balance and proprioception can limit function and predispose to postural and gait deviations; the impact of bilateral UL loss on balance should not be underestimated
- The most common postural deviation observed in the UL amputee is scapular elevation and protraction, internal rotation and adduction of the gleno-humeral joint, restricted cervical rotation and side flexion , kyphotic posture with pocking chin (see figure 2)
- In walking arm swing can be reduced and accompanied by thoracic side flexion to the amputated side
Figure 2
Hand dominance, function and testing of ADLs[edit | edit source]
- PADL and ADL
- In the case of the single UL amputee the remaining arm will become the dominant arm
- Dexterity and ability of the remaining arm to perform functional tasks and personal activities of daily living
- Ability of the lower limbs to assist in functional activities
Considerations for pre-operative physiotherapy (where possible)[edit | edit source]
- Explore the opportunity to meet with another with the same level to inform, demonstrate and reassure. As with the LL amputee, source local prosthetic centres or national organisations (Limbless Association)
- Where possible, an appointment to be seen and assessed by a specialist prosthetic MDT at a regional rehabilitation centre can provide the opportunity to meet with an other UL amputee/s, to see and gain facts about appropriate prostheses and prosthetic use
- Otherwise, early liaison with prosthetic centre to gain advice. Be cautious with patient expectations of prosthetic use
- Discuss pain relief and potential for pain post operatively, phantom limb sensation (PLS) and phantom limb pain (PLP)
- Plan pre and postoperative physiotherapy intervention through agreeing realistic short term goals
- Situation permitting, maintain and/ or increase proximal joint ROM and muscle strength both arms
- In anticipation of transhumeral prosthetic use incorporate scapular movement e.g. protraction and retraction
- Introduce functional activities in the ‘dominant’ arm and lower limbs
- Advice on posture, teach and correct
- Concurrent treatment
Post amputation and pre-prosthetic rehabilitation[edit | edit source]
Assessment post amputation should include information about the quality of the residual limb/ residuum (stump) as this will have an impact on the prosthetic rehabilitation potential for the patient
- Wound condition
- Oedema
- Residual limb length
- Soft tissue cover
- Cut end of bone (prominent or not)
- Shape
- Sensation
- Position of suture line, adherence
- Pain
The principles of wound care, oedema control, pain management will align to that of the LL. Similarly, emotional support, goal planning. Where possible there should be close working with the OT
- Oedema control
- Elevation e.g. at rest on a pillow with the distal end at a higher level than the shoulder; supported via a drip stand when walking
- Compression via compression shrinker sock or elastic bandage
- Active exercises
- Pain management
- Encourage residual limb handling & desensitising – this can help adjustment to changed body image
- Note that phantom limb sensation and pain can be more common in the UL; consider the relative representation of the hand on the homunculus and proximity to the face. PLP experienced by the UL amputee can be associated with facial sensations
- Emotional support
- MDT approach, onward referral for specialist support e.g. clinical psychologist, counsellor
- Patient and family /carer – as above
- Discuss lifestyle, employment, hobbies and home situation
- Discuss expectations of prosthesis
- Agree goals for treatment
Physiotherapy specific[edit | edit source]
- Postural advice in sitting, standing and walking
- Maintain and > proximal joint ROM & strength
- Encourage early active movement of all proximal joints from 1st day post amputation
- Resisted exercise as soon as pain allows
- Active ROM Cx and Tx spine
- GH joint – flex/ ext; abd/ add; ext rot/ int rot
- Scapula – depression/ elevation; protraction/ retraction
- GH and scapula rhythm – NB protraction and flexion principle movement required for a body powered prosthesis
- Elbow – flex/ ext, pron/ sup
- Scapula – depression/ elevation; protraction/ retraction
- Physiotherapy treatment techniques include
- Mobilisations, stretches (see figure 3), auto resisted exercises, theraband
Figure 3
- Base on normal movement e.g. reach and grasp, PNF (see Figure 4)
Figure 4
- Proprioception for shoulder e.g. stabilisation exercises, 4 point kneeling, wobble cushion, ball
- Normalisation of residual limb sensation e.g. handling, exercises, loading (see Figure 5)
Figure 5
- Pilates & core stability
- Exercise leaflets e.g. core stability
- Incorporate prosthetic use into functional exercises at later stage based on normal movement (see figure 6)
Figure 6
- Apply ergonomics e.g. car, work station, sleep posture (see figure 7)
Figure 7
- Encourage to use residual limb as much as possible with PADLs and ADLs
- Use simple gauntlet to hold utensils, comb, toothbrush (see figure 8)
Figure 8
- Encourage symmetry of movement
- Avoid one handedness i.e. of remaining arm
- Balance, gait and posture
- Walk, run, turn
- Encourage arm swing and trunk rotation
- Education and advice on prevention of problems e.g. of not moving or overuse
- Stiff, shoulder pain, Cx & Tx pain, tenosynovitis. See below
- Functional limitations e.g. unable to wash axilla/ apply deodorant
- Exercises for the dominant hand
- Hand mobility
- Writing (see figure 9)
- Dressing
Figure 9
- Mobility, balance and functional activities for the bilateral UL amputee (see figures 10, 11)
Figure 10
Figure 11
Considerations for prosthetic rehabilitation[edit | edit source]
Motivation is essential if patients are planning to use a prosthesis. Amputees with lower limb loss often choose to wear prostheses but those with UL loss often don’t use prosthetic arms, especially children. Developing skills with a prosthesis is a bit like learning to ride a bike, once learnt it is easy to use later.
It is advisable to encourage amputees to learn to use a prosthesis early and put in the time practise time required to be proficient. Once patients have found a way to do something and have adjusted to being without a hand there is less tendency to adapt to using a prosthesis.
Early prosthetic use is recommended; amputees are more likely to adapt with the risks of becoming one handed and with less motivation to use a prosthesis.
Early referral for prosthesis and rehabilitation is advised.
- Seek out what the patient’s goal is
- Identify the potential of the prosthesis that the client is due to receive, or is available, as it is and what could be added
- Enabling the patient to put on and take off the prosthesis at will
- Making sure that the fit of the prosthesis is not going to create harm by chaffing or pressing on hypersensitive locations. Check the skin before and after each session and teach the patient to know what to look for
- That they can put clothes over the prosthesis easily. The prosthesis may not assist with putting on undergarments, but can assist with larger garments
- Enable the patient to know how far they can reach, when wearing the prosthesis and still operate it. That they know where the prosthesis ends For example to enable patient to move around a crowded environment without knocking things in error
- To be able to grasp and release a variety of objects at will, and with confidence
- To be able to maintain a grasp while doing other activities eg walking around or talking. This sustained grip is ideally relaxed posture rather than global tension
- Where there is a change in hand dominance it is necessary to do repetitive practice to develop ease of movement
- Ultimately the prosthesis assumes the role of a tool and they are able to focus on the task and expression that they are engaged in. They are able to relate to other people on the basis of chosen activities and not that the prosthesis dominates their awareness
Common physical problems associated with UL loss – considerations and potential management strategies[edit | edit source]
- Injury, repetitive strain/ overuse in the remaining arm e.g. shoulder impingement, tenosynovitis, epicondylitis, Carpal Tunnel Syndrome
- Increased risk in certain non amputee populations e.g. typists
- Altered biomechanics and posture due to amputation
- Favour and stress intact arm
- Minimal research evidence of overuse/ repetitive strain injuries in UL amputees[9][10][11]
- Problems more prevalent in proximal amputations
- Prosthetic use or lack of employment not protective of remaining arm[9]
- No unilateral UL amputee is immune to developing overuse injury
- Risk factors include
- Repetition e.g. texting
- High force
- Awkward joint posture
- Prolonged constrained posture
- Direct pressure
- Vibration
- Greater risk factors for wrist and hand with acquired amputation versus congenital
- Increased BMI
- Apply knowledge from other patient populations[10] to manage; utilise musculoskeletal and pain assessment approach
- Education on prevention of joint overuse, pacing, consider influence of posture on movement, encourage early use of residual limb to minimize one handedness with associated greater risk of overuse injury in remaining arm
- Recognise 3 stages of overuse syndrome
Stage 1 – Increased aching and tiredness during an activity that subsides with overnight rest – a warning symptom
Stage 2 – Discomfort into the next day with earlier fatigue – suggests injury is developing (reduce strain on affected tissues by minimising aggravating activities and prescribe frequent rests and/ or splinting e.g. carpal tunnel, thumb spica)
Stage 3 – Chronic fatigue, pain and weakness that persists despite rest – onset of fibrosis (complete rest via splinting, medical management e.g. steroid injection)
- Neck & thoracic back pain (e.g. asymmetry of posture due to reduced weight on one side of body)
- Tight anterior shoulder capsule, tight pectoral & anterior deltoid muscles e.g. established amputees/ persons with congenital loss with long term habits, protective and postural changes
- Reduced glenohumeral range of movement
- Poor glenohumeral / scapula rhythm
- Weak rotator cuff i.e. subscapularis, infraspinatus, teres major & minor (inherently weaker > 60 years of age)
- Phantom pain.
Prevention and management of common physical problems associated with UL loss includes[edit | edit source]
- Patient information and education as early as possible
- Preventative measures e.g. avoid excessive loading and repetitive movements, manage posture
- Adaptations to encourage function, bilateral arm use and symmetry of movement
- Postural advice including ergonomics e.g. height of work stations
- Mobilising, stretching and strengthening exercises including core
- Facilitation of normal rhythmical movement
- ‘Pacing’ and appropriate goal setting
- Self management of early symptoms e.g. rest
- Thermal modalities
- Ultrasound
- Immobilisation via splinting e.g. carpal tunnel, thumb spica
- NSAIDs
- Steroid injections
- Friction massage
- Nerve blocks
- Surgery e.g. carpal tunnel decompression, tendon repair
- MDT responsibility – beware of focus on prosthetic rehab and forgetting reliance on remaining arm
- Functioning prosthesis versus cosmetic prosthesis or no prosthesis may limit common physical problems[12][10]
Considerations for the child with UL amputation[edit | edit source]
Refer to the Association for Children with Upper Limb Deficiency
- Children with an UL amputation may experience additional problems and challenge in relation to the cause of amputation and/ or as they grow older e.g. musculoskeletal pathologies
- Regular review is essential to assess and treat symptomatically
Standards of practice[edit | edit source]
Refer to PIRPAG (Physiotherapy Interregional Prosthetic Audit Group) recommendations
Recommendations for practice from Roehampton Rehabilitation Centre
References[edit | edit source]
- ↑ Atkins, D. J. Prosthetic Training. In: Smith, D, G., Michael, J.W and J. H. Bowker. Editors, 2004, Atlas of Amputations and Limb Deficiencies. 3rd Ed. American Acadamy of Orthopaedic Surgeons
- ↑ 2.0 2.1 World Health Organization. 2009. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care.
- ↑ The Amputee Statistical Database for the United Kingdom 2004/05. Information Services Division NHS Scotland on behalf of National Amputee Statistical Database (NASDAB)
- ↑ Mangled extremity severity score (MESS) (Johnson et al 1990) http://www.mdcalc.com/mangled-extremity-severity-score-mess-score/
- ↑ Trauma Score and the Injury Severity Score (TRISS) (Boyd et al1987) http://www.trauma.org/index.php/main/article/387/
- ↑ Broomhead P, Dawes D, Hancock A, Unia P, Blundell A, Davies V. 2006. Clinical guidelines for the pre and post operative physiotherapy management of adults with lower limb amputation. Chartered Society of Physiotherapy, London
- ↑ Shin, A, Y., Bishop, Al T and J. W. Michael. 2004. Brachial Plexus Injuries: Surgical and Prosthetic Management. In: Smith, D, G., Michael, J.W and J. H. Bowker. Editors, Atlas of Amputations and Limb Deficiencies. 3rd Ed. American Acadamy of Orthopaedic Surgeons
- ↑ Carnegie F. 1999. Upper limb amputation and congenital limb deficiency. In Therapy for Amputees. Engstrom B and Van de Ven C. Churchill
- ↑ 9.0 9.1 Jones, L,E and J,H Davidson. 1999. Save that arm: a study of problems in the remaining arm of unilateral upper limb amputees. Prosthetics and Orthotics International. 23:55-58
- ↑ 10.0 10.1 10.2 Gambrell, C. 2008. Overuse Syndrome and the Unilateral Upper Limb Amputee: Consequences and Prevention. Journal of Prosthetics & Orthotics. 20:126-132
- ↑ Biden, E., L. Manor., G. Bush and W.L Hill. 2015. Repetitive Strain Injury Risk Factors in Upper Limb Amputees. ISPO World Congress Lyon, France. 2015
- ↑ Sato et al. 1999. Carpal tunnel syndrome involving unaffected limbs of stroke patients. Stroke. 30:414-418