The Role of Rehabilitation Within Low Resource Settings
Top Contributors - Robin Tacchetti, Robin Leigh Tacchetti, Wanda van Niekerk, Tarina van der Stockt, Kim Jackson, Jess Bell and Stacy Schiurring
Introduction[edit | edit source]
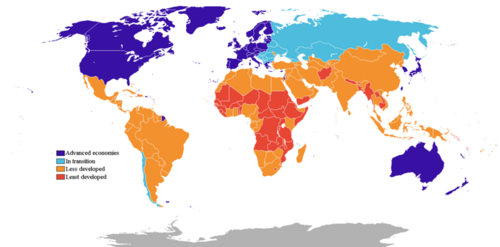
Recent estimates by the World Health Organization state that over 2.4 billion people[1] in the world need rehabilitation services. 80% of these individuals are from low- and middle-income countries. Poverty breeds disability and disability breeds poverty as they are inherently linked.[2] Compounding poverty in these settings is malnutrition, non-potable water, unsanitary conditions and inadequate shelter.[3] Attaining healthcare services in these poor areas is particularly challenging as many of these areas are also grappling with political uncertainty, corruption, volatile security, lack of professional healthcare training, dysfunctional and/or overwhelmed health systems and insufficient roads to access services.[4]
Health Inequalities in Low Resource Settings[edit | edit source]
Poor people living in low-income settings tend to be the least healthy and benefit the most from healthcare. Social determinants of health such as education, income level, gender, ethnicity, place of residence and employment status have a direct correlation on the rate of illness. with lower income-countries bearing a higher burden of disease or illness.[5]
Access to Care[edit | edit source]
Accessibility of healthcare services is a crucial problem. When discussing access to care, one needs to consider if the services are available, affordable and well accepted.[6]
Availability[edit | edit source]
If healthcare services are provided within these settings, it is often found to be of poor quality. Substandard care or non-effective care tends to lead to mistrust in healthcare and a decrease in demand for these services. This in turn impacts whether or not individuals seek future care and breeds mistrust in providers.[6]
Affordability[edit | edit source]
When healthcare services are obtainable, are they affordable?[6]
Acceptability[edit | edit source]
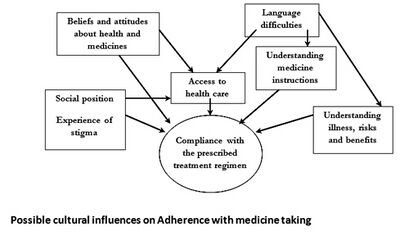
People living in low-resource settings may have educational and cultural differences that may prevent them from pursuing healthcare services and/or they may not appreciate the potential health benefits of available services.[6]
Rehabilitation Specific[edit | edit source]
Within low resource settings, the need for rehabilitation services are high and increasing.[7] [8] However, there are low resources and low supply (meaning both quantity and quality). These countries have less than ten skilled rehabilitation providers per 1 million population.[7]
The demand for rehabilitation services is continuing to increase as the world manages global warming, droughts, floods, natural disasters, war and conflict, epidemics and migration and displacement.[9] [10] This video by the World Health Organization explains why rehabilitation services are so important in low-income countries.
Future Course for Rehabilitation Professionals[edit | edit source]
Knowledge[edit | edit source]
When working in low-income settings, rehabilitation professionals must investigate the local political, economic, cultural and social circumstances within the region. High-income country interventions should be adapted to the cultural norms of local settings. Additionally, when donating equipment and medication, it is necessary to consider the needs of the location to which they are being sent.[12] Learning about the culture will prevent a misuse of donations as in the real-life examples below:
- Hip prosthesis provisions distributed to a country where people were used to squatting[12]
- Dispensing of lice shampoo to people who cannot read and who view shampoo as a luxury that should be shared with others[12]
Advocate[edit | edit source]
In low resource settings, there is minimal recognition of rehabilitation services. This prevents the rehabilitation sector from gaining an equal footing in local health systems. Advocating for rehabilitation services to become a division within the Ministries of Health would allow rehabilitation professionals to access education models, health resources and research funding. Rehabilitation professionals should promote their services to health policymakers, local health authorities and to the people living within these areas.[9]
Listen[edit | edit source]
Utilising high-income country interventions, even evidence-based research, may not be applicable in low-resource settings. Provided services need to be determined by the people living in the region and reflect the situation of these diverse settings. The most effective way to initiate care is to listen to experts on the ground. These experts can identify resources that are available within that particular setting and any cultural beliefs that need to be considered.[9]
Partnerships[edit | edit source]
Rehabilitation professionals from higher-resource settings can assist low-resource healthcare professionals via education and professional development. Non-governmental organisations should move from short-term to long-term partnerships with local authorities to improve health care over time.[12]
Resources[edit | edit source]
- https://www.who.int/initiatives/rehabilitation-2030
- https://www.who.int/disabilities/care/Need-to-scale-up-rehab-July2018.pdf
- Role of Physiotherapists in Global Health
- Global Health
- Determinants of Health
- Rehabilitation Contexts
- Introduction to Rehabilitation
References[edit | edit source]
- ↑ World Health Organization. 2019. Available from: https://www.who.int/teams/noncommunicable-diseases/sensory-functions-disability-and-rehabilitation/global-estimates-of-the-need-for-rehabilitation#:~:text=According%20to%20this%20landmark%20global,billion%20to%202.41%20billion%20people.
- ↑ Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low-and middle-income countries. International journal of environmental research and public health. 2018 Oct;15(10):2165.
- ↑ Orach D, Garimoi C. Health equity: challenges in low income countries. African health sciences. 2009 Oct 1;9(s2):S49-51.
- ↑ Barth CA. Meeting the needs of people with physical disabilities in crisis settings. Bulletin of the World Health Organization. 2019 Dec 1;97(12):790.
- ↑ WHO. Health inequities and their causes. Available from https://www.who.int/news-room/facts-in-pictures/detail/health-inequities-and-their-causes (accessed 15/11/2021)
- ↑ 6.0 6.1 6.2 6.3 Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur Rahman M. Poverty and access to health care in developing countries. Annals of the new York Academy of Sciences. 2008 Jun;1136(1):161-71.
- ↑ 7.0 7.1 Bright T, Wallace S, Kuper H. A systematic review of access to rehabilitation for people with disabilities in low-and middle-income countries. International journal of environmental research and public health. 2018 Oct;15(10):2165.
- ↑ Heine M, Derman W, Hanekom S. Towards a framework for the scale-up of rehabilitation for patients with non-communicable disease in low-resource settings. medRxiv. 2022 Jan 1.
- ↑ 9.0 9.1 9.2 Barth, C. The Role of Rehabiliation in Low Resource Settings. Course. Plus. 2021
- ↑ Jesus TS, Landry MD, Hoenig H. Global need for physical rehabilitation: systematic analysis from the Global Burden of Disease Study 2017. International journal of environmental research and public health. 2019 Jan;16(6):980.
- ↑ WHO: Rehabilitation: Key for health in the 21st century. Available from https://www.youtube.com/watch?v=a8uaRziXruc (last accessed 15 November 2021)
- ↑ 12.0 12.1 12.2 12.3 Bauer I. More harm than good? The questionable ethics of medical volunteering and international student placements. Tropical diseases, travel medicine and vaccines. 2017 Dec;3(1):1-2.