The Pelvic Girdle Musculoskeletal Method - Introduction: Difference between revisions
(added content, still to be formatted and referenced) |
No edit summary |
||
| (30 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox"> '''Original Editor '''- [https://members.physio-pedia.com/course_tutor/deborah-riczo/ Deborah Riczo], [[User:Wanda van Niekerk|Wanda van Niekerk]]<br> | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
</ | |||
< | == Overview of the Pelvic Girdle Musculoskeletal Method<sup>sm</sup> == | ||
The Pelvic Girdle Musculoskeletal Method<sup>sm</sup> (PGM Method<sup>sm</sup>) has been developed by Deborah Riczo, a physiotherapist and leading expert in the field of pelvic girdle pain. She has been teaching this method to physiotherapists and physiotherapy assistants since 2011.<ref name=":0">Riczo, D. Introduction to the Pelvic Girdle Musculoskeletal Method Course. Plus , 2021.</ref> | |||
== Components of the PGM Method<sup>sm</sup> == | |||
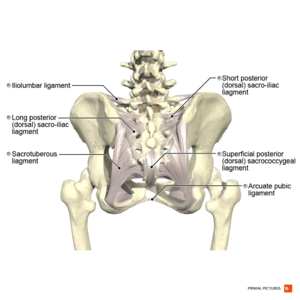
</ | [[File:Ligaments of the pelvis posterior aspect Primal.png|thumb]] | ||
The PGM<sup>sm</sup> method is a holistic approach to pelvic girdle pain and includes the following components<ref name=":0" />: | |||
* Clinical history/pain location | |||
** [[Recognising Pelvic Girdle Pain]] | |||
* Special tests | |||
** Tools to use to identify [[Pelvic Girdle Dysfunction: Literature Review|pelvic girdle pain]] | |||
** [[Pelvic Girdle Dysfunction: Literature Review]] | |||
* Pelvic sacral balancing exercises | |||
** Interventions used to correct issues of innominate and sacral positional strain. These include: | |||
*** Targeted strengthening exercises | |||
*** Targeted stretching exercises | |||
* Core strengthening | |||
* Patient education | |||
* Consideration of sacroiliac belt | |||
== PGM<sup>sm</sup> Method Special Tests == | |||
This method includes two sets of special tests to assess dysfunction. For the purpose of this page and the Plus course, Introduction to the PGM method, dysfunction refers to a tendency for a positional strain caused by muscles that are overstrained versus a positional change. The two sets of special tests are:<ref name=":0" /> | |||
# Innominate dysfunction cluster of special tests | |||
# Sacral dysfunction special tests | |||
'''''In the PGM method, it is important to screen the innominate first.''''' | |||
=== Innominate Imbalance Special Tests === | |||
These are a cluster of 4 special tests and 3 out of 4 of these tests must be positive.<ref name=":0" /> The tests are:<ref name=":0" /> | |||
# Asymmetrical hip internal rotation (IR) range of motion (>10 degrees between sides) | |||
# Asymmetry/ tenderness of the symphysis pubis | |||
# Unilateral tenderness of ASIS and/or the Iliac Crest | |||
# Unilateral tenderness of PSIS and/or long dorsal sacroiliac ligament | |||
==== 1. Special Test: Asymmetrical Hip Rotation Range of Motion (ROM) ==== | |||
* Comparison of hip internal and external range of motion between sides | |||
** Optimal assessment position is prone | |||
** Can be assessed in other positions | |||
* Use an inclinometer or smartphone application to measure the range of motion | |||
* A difference of more than 10° between left and right internal hip rotation is regarded as a positive test result | |||
* Important to assess: | |||
** "Perceived" tightness unilaterally | |||
** Reproduction of symptoms unilaterally during the assessment | |||
===== Evidence for the Relationship of Hip Range of Motion and Low Back Pain and Pelvic Girdle Dysfunction ===== | |||
Ellison et al. (1990)<ref name=":1">Barbee Ellison J, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Physical therapy. 1990 Sep 1;70(9):537-41.</ref> reported differences in hip rotation in patients with low back pain compared to patients without low back pain (controls). The researchers reported that the total hip external rotation was greater than the total hip internal rotation in patients with low back pain. A significant result was a difference of more than 10°.<ref name=":1" /> | |||
Cibulka et al. (2002)<ref name=":2">Cibulka MT. Understanding sacroiliac joint movement as a guide to the management of a patient with unilateral low back pain. Manual Therapy. 2002 Nov 1;7(4):215-21.</ref> indicated that the presence of asymmetrical hip rotation range of motion may be an indication of [[Sacroiliac Joint Syndrome|sacroiliac region pain]].<ref name=":2" /> | |||
Prather et al. (2017)<ref name=":3">Prather H, Cheng A, Steger-May K, Maheshwari V, Van Dillen L. Hip and lumbar spine physical examination findings in people presenting with low back pain, with or without lower extremity pain. journal of orthopaedic & sports physical therapy. 2017 Mar;47(3):163-72.</ref> indicated an association between reduced hip internal rotation and low back pain.<ref name=":3" /> | |||
Hartigan et al. (2020)<ref name=":4">Hartigan E, McAuley JA, Lawrence M, Brucker W, King A, Tryon B, DeSilva M. Hip Angles, Joint Moments, and Muscle Activity During Gait in Women With and Without Self-reported Stress Urinary Incontinence. Journal of Women’s Health Physical Therapy. 2020 Jul 1;44(3):107-16.</ref> investigated hip angles, joint moments and muscle activity during gait in women with self-reported stress urinary incontinence and found the following in this population<ref name=":4" />: | |||
* Weakness, poor endurance and timing of the pelvic floor muscles | |||
* Decreased ability of hip position control in the non-dominant leg | |||
* Decreased strength of the hip abductors and hip external rotators | |||
* Increased gluteus maximus activity of the non-dominant leg | |||
* Women with stress urinary incontinence present with altered hip biomechanics during the stance phase of gait. Although women with stress urinary incontinence seem to be using greater hip abduction and external rotation forces, motor control strategies seem to be lacking and unable to avoid greater hip adduction and internal rotation positions.<ref name=":4" /> | |||
===== Test Reliability ===== | |||
Inter- and intra-rater reliability have been established for the measurement of hip internal and external rotation in prone.<ref name=":1" /> Measurement of hip internal and external rotation in prone with a goniometer is performed as follows: | |||
Hip internal rotation (IR) and external rotation (ER) are measured with the subject in prone, with the hip in a neutral position and the knees flexed to 90°. The goniometer is centred at the joint line, with the movement arm of the goniometer aligned along the midline of the tibia and the stationary arm aligned perpendicular to the floor.<ref name=":5">Charlton PC, Mentiplay BF, Pua YH, Clark RA. Reliability and concurrent validity of a Smartphone, bubble inclinometer and motion analysis system for measurement of hip joint range of motion. Journal of Science and Medicine in Sport. 2015 May 1;18(3):262-7.</ref> The patient is asked to move the hip into internal rotation while keeping the hips stationary on the table. The patient is then asked to move the hip into external rotation while keeping the hips stationary on the table. Measures are assessed on the contralateral hip as well. | |||
Measurement of hip rotation in prone with a smartphone application (there are various applications available, the method described here is for the Clinometer app) may be done as follows:<ref name=":6">Miley E, May J, Albertin E, Takahashi E, Goodman C, Pettaway A. Reliability and Validity for Measuring Active Hip Rotation with the Clinometer Smartphone Application™. Journal of Rehabilitation Sciences & Research. 2019 Dec 1;6(4):193-9.</ref> | |||
The top of the smartphone is placed 3cm below the tibial tuberosity and the base of the smartphone is positioned towards the midline of the medial and lateral malleoli.<ref name=":5" /> The patient is asked to move the hip into internal rotation (IR) and then into external rotation (ER). The clinician provides verbal cues to ensure that no compensatory movements occur during the motion.<ref>Cheatham S, Hanney WJ, Kolber MJ. Hip range of motion in recreational weight training participants: a descriptive report. International Journal of Sports Physical Therapy. 2017 Oct;12(5):764.</ref> Measures are also assessed on the contralateral limb. | |||
Recent research demonstrated moderate to excellent intra-rater reliability for the measurement of active hip IR and ER when using the goniometer and a smartphone application (Clinometer).<ref name=":6" /> Good to excellent interrater reliability was also reported with the measurement of active hip IR and ER with both goniometer and smartphone application. Additionally, it is suggested that the smartphone application may be a valid alternative to hand-held goniometry when measuring active hip IR and ER in clinical practice.<ref name=":6" /> | |||
Hip rotation range of motion can also be assessed in sitting as well as in supine in the PGM method.<ref name=":0" /> | |||
* [[Goniometry: Hip External Rotation]] | |||
* [[Goniometry: Hip Internal Rotation]] | |||
<div class="row"> | |||
<div class="col-md-4"> {{#ev:vimeo|399220225|250}} <div class="text-right"><ref>ATX Physical Therapy. Prone hip external and internal rotation assessment. Available from https://vimeo.com/399220225 (last accessed 3 January 2021)</ref></div></div> | |||
<div class="col-md-4"> {{#ev:youtube|watch?v=jFBD1wZvXIc|250}} <div class="text-right"><ref>MCCCPTAP. Hip IR and ER ROM with a goniometer. Available from https://www.youtube.com/watch?v=jFBD1wZvXIc (last accessed 3 January 2021)</ref></div></div> | |||
<div class="col-md-4"> {{#ev:youtube|watch?v=0MQ01JbJOGs|250}} <div class="text-right"><ref>FITT. 19 Medial Hip Rotation Goni. Available from https://www.youtube.com/watch?v=0MQ01JbJOGs (last accessed 3 January 2021)</ref></div></div> | |||
</div> | |||
==== 2. Special Test: Asymmetry/ Tenderness of the Symphysis Pubis ==== | |||
2. | |||
===== Palpation of the Symphysis Pubis ===== | |||
The presence of unilateral tenderness with palpation of the symphysis pubis is considered a positive result in the PGM method.<ref name=":0" /> The sensitivity (66%) and specificity (99%) of palpation of the anterior surface of the symphysis pubis with the person in supine have been established. The examiner uses palpation to elicit pain that persists for more than 5 seconds after removal of the examiner’s hand.<ref>Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. European Spine Journal. 2000 Apr 1;9(2):161-6.</ref> | |||
Anteroposterior or superoinferior displacement of the upper border of the pubic symphysis or pubic tubercle can also be felt with palpation.<ref>Jain S, Eedarapalli P, Jamjute P, Sawdy R. Symphysis pubis dysfunction: a practical approach to management. The Obstetrician & Gynaecologist. 2006 Jul;8(3):153-8.</ref> This may sometimes be more difficult, for example, in the third trimester of pregnancy.<ref name=":0" /> | |||
A painful unilateral response on the side that the patient is complaining of the pain is a positive result in the PGM method.<ref name=":0" /> | |||
{{#ev:youtube|watch?v=JKuBjqbzpc8}}<ref>Orthopedic Physical Examination Tests. Pubic symphysis palpation. Available from https://www.youtube.com/watch?v=JKuBjqbzpc8. (last accessed 3 January 2021) </ref> | |||
===== Range of Motion at the Symphysis Pubis ===== | |||
Garras et al. (2008)<ref name=":7">Garras DN, Carothers JT, Olson SA. Single-leg-stance (flamingo) radiographs to assess pelvic instability: how much motion is normal?. JBJS. 2008 Oct 1;90(10):2114-8.</ref> investigated the range of movement at the symphysis pubis by using single-leg stance radiographs. Multiparous women had a significantly increased physiologic range of pubic translation compared to men and nulliparous women. Up to 5 mm of physiologic motion can occur at the pubic symphysis in asymptomatic individuals.<ref name=":7" /> | |||
==== 3. Special Test: Unilateral Tenderness of ASIS and/or the Iliac Crest ==== | |||
As part of the PGM Method, only unilateral tenderness of the iliac crest and/or the anterior superior iliac spine (ASIS) is assessed and not asymmetry.<ref name=":0" /> The standing ASIS asymmetry test has poor reliability and has no value during the examination.<ref>Cook C, Hegedus E. ''Orthopedic Physical Examination Tests: An Evidence-Based Approach''. 2nd ed. Prentice Hall; 2012</ref> | |||
===== Test Reliability ===== | |||
Research has shown a good discriminative ability and inter-rater reliability when two criteria (localised tenderness and pain recognition) were combined.<ref>Njoo KH, Van der Does E. The occurrence and inter-rater reliability of myofascial trigger points in the quadratus lumborum and gluteus medius: a prospective study in non-specific low back pain patients and controls in general practice. Pain. 1994 Jan 1;58(3):317-23.</ref> Good interobserver agreement was reported for “localised tenderness” and “typical pain” criteria on iliac crest pain syndrome in patients with non-specific low back pain.<ref>Njoo KH, Van der Does E, Stam HJ. Interobserver agreement on iliac crest pain syndrome in general practice. The Journal of rheumatology. 1995 Aug 1;22(8):1532-5.</ref> McCombe et al. (1989)<ref name=":8">McCombe PF, Fairbank JC, Cockersole BC, Pynsent PB. 1989 Volvo Award in clinical sciences. Reproducibility of physical signs in low-back pain. Spine. 1989 Sep 1;14(9):908-18.</ref> reported that palpation tests for bony tenderness were more reliable than palpation tests for soft tissue tenderness.<ref name=":8" /> | |||
{{#ev:youtube|watch?v=dCzuLb3Cng8&t=125s}}<ref>SapiensMove_PT_Videos. Anterior and Lateral Hip & Pelvis Palpation. Available from https://www.youtube.com/watch?v=dCzuLb3Cng8&t=125s (last accessed 3 January 2021)</ref> | |||
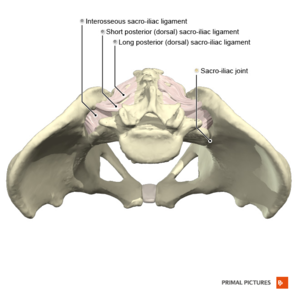
==== 4. Special Test: Unilateral Tenderness of PSIS and/or Long Dorsal Sacroiliac Ligament ==== | |||
[[File:Sacro-iliac joint Primal.png|thumb]] | |||
In the PGM Method, tenderness with palpation of the posterior superior iliac spine (PSIS) and/or the long dorsal sacroiliac ligament on the symptomatic side is considered a positive test result.<ref name=":0" /> | |||
===== Palpation of the Long Dorsal Sacroiliac Ligament ===== | |||
The long dorsal sacroiliac ligament is known as a major pain generator for pelvic pain.<ref>Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, Stoeckart R, Snijders CJ, Mens JM. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996 Mar 1;21(5):556-62.</ref><ref>Vleeming A, De Vries HJ, Mens JM, Wingerden JP. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta obstetricia et gynecologica Scandinavica. 2002 Jan 1;81(5):430-6.</ref> Tenderness with palpation of this ligament does seem to indicate sacroiliac joint pain versus a low back problem. The sensitivity of this palpation test increases when it is combined with the active straight leg raise test and the thrust test.<ref>Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.</ref> | |||
{{#ev:youtube|watch?v=ers5kA9vK_o}}<ref>SapiensMoves_PT_Videos. Posterior Pelvis & Lumbar Palpation. Available from https://www.youtube.com/watch?v=ers5kA9vK_o (last accessed 3 January 2021)</ref> | |||
=== Sacral Imbalance Special Tests === | |||
There are two reasons/indications for performing the sacral tests in the PGM Method:<ref name=":0" /> | |||
* A negative cluster of PGM signs for the innominate (less than 3 out of 4 positive tests), but the patient has clinical history and symptoms consistent with sacroiliac pelvic girdle pain | |||
* After having completed the interventions for the innominate dysfunction to address the positional strain, the patient’s improve, innominate tests are negative, but the patient is still displaying some clinical signs and complaints of sacroiliac pain or pelvic girdle dysfunction | |||
==== 1. Special Test: Sacral Springing Test ==== | |||
This test is similar to the [[Sacral Thrust Test|sacral thrust test]] and involves gross springing of the sacrum. The patient is in prone, the therapist uses the pisiform of their hand and applies a gentle springing of the sacrum. If this relieves the symptoms of the patient, this can be used as a treatment technique. The test is positive if pain is elicited. If no pain is elicited with this test, but pelvic girdle dysfunction is still suspected, move on to assessing each individual pole of the sacrum.<ref name=":0" /> | |||
{{#ev:youtube|watch?v=zySIMEn3u7w}}<ref>Thomasz Grass. Sacral Spring Test. Available from https://www.youtube.com/watch?v=zySIMEn3u7w (last accessed 3 January 2021)</ref> | |||
==== 2. Special Test: Springing of Four Poles of Sacrum ==== | |||
This test involves the individual springing of the four poles of the sacrum in a similar way that the sacral springing test is performed and is considered positive if pain is present.<ref name=":0" /> The four poles of the sacrum are: | |||
* The right and left base of the sacrum | |||
* The right and left inferior lower angles of the sacrum (ILA) | |||
If the patient's symptoms are relieved with the individual springing on a specific pole, this can be used as a treatment technique. | |||
When performing the individual springing on the four different poles it is important to take note of the pain provocation patterns.<ref name=":0" /> | |||
===== Pain Provocation Patterns ===== | |||
* Diagonal | |||
** For example, painful with the springing of the right superior pole and the left inferior lateral angle (ILA) of the sacrum - this may indicate a torsion dysfunction<ref name=":0" /> | |||
* Vertical | |||
** For example, pain provocation with the springing of the right superior pole and right inferior lateral angle of the sacrum - this may indicate the presence of an "up slip" or a "down slip." This is often best treated with postural type education and manual myofascial releases<ref name=":0" /> | |||
* Horizontal | |||
** Pain provocation on both superior poles or inferior lateral angles of the sacrum (ILA) - this is not a torsion or "up slip/down slip" dysfunction and would more likely indicate a positional postural type dysfunction<ref name=":0" /> | |||
== Virtual Assessment of Pelvic Girdle Dysfunction == | |||
The [[Coronavirus Disease (COVID-19)|COVID-19]] [[Endemics, Epidemics and Pandemics|pandemic]] has brought [[Introduction to Telehealth|telehealth]] and [[Telehealth Evaluation|virtual patient assessments]] to the forefront in physiotherapy.<ref>Bennell KL, Lawford BJ, Metcalf B, Mackenzie D, Russell T, van den Berg M, et al. [https://www.sciencedirect.com/science/article/pii/S1836955321000527 Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study]. J Physiother. 2021 Jul;67(3):201-9. </ref><ref>Brigo E, Rintala A, Kossi O, Verwaest F, Vanhoof O, Feys P, Bonnechère B. [https://www.mdpi.com/1660-4601/19/16/10325 Using telehealth to guarantee the continuity of rehabilitation during the COVID-19 pandemic: a systematic review]. Int J Environ Res Public Health. 2022 Aug 19;19(16):10325. </ref><ref>Haines KJ, Sawyer A, McKinnon C, Donovan A, Michael C, Cimoli C, et al. [https://www.sciencedirect.com/science/article/pii/S0031940622000943 Barriers and enablers to telehealth use by physiotherapists during the COVID-19 pandemic]. Physiotherapy. 2022 Sep 7;118:12-9. </ref> For more info on telehealth and rehabilitation, have a look at these pages: | |||
* [[Introduction to Telehealth]] | |||
* [[Fundamentals of Telehealth Technology]] | |||
* [[Telehealth Evaluation]] | |||
* [[Practical Considerations in Telehealth]] | |||
* [[The Basics of Telehealth Assessment and Treatment|The basics of Telehealth Assessment and Treatment]] | |||
* [[Ethical and Professional Considerations with Telehealth]] | |||
== | === Recommendations for Virtual Consultation === | ||
[[File:Telehealth image.jpg|thumb]] | |||
Here are some recommendations on what and how to assess pelvic girdle dysfunction virtually:<ref name=":0" /> | |||
<u>Initial screening</u> | |||
Rule out centralisation with the McKenzie approach (repeated back extensions or prone press-ups). If the patient's symptoms centralise, initial treatment should be focused on the lumbar spine before further assessment using the PGM Method. | |||
or | |||
<u>PGM Method screening</u> | |||
* Patient in standing (Special Tests 2-4): | |||
** Assess unilateral tenderness or pain with palpation of ASIS/iliac crest | |||
** Assess unilateral tenderness or pain with palpation of symphysis pubis | |||
** Assess unilateral tenderness or pain of the PSIS/long dorsal sacroiliac ligament | |||
* Patient in sitting (Special Test 1): | |||
** Asymmetrical hip rotation range of motion (ROM) | |||
**[[File:Hip external rotation seated. Rehab my patient.png|thumb]]The patient can place the lateral malleoli of the ankle on the contralateral knee (figure of 4 - examining external rotation of the hip) | |||
** From the previous position, the patient can bring the leg across the body and assess pain with this movement (moving hip into internal rotation) | |||
** Knee to chest | |||
Transitional movements should be assessed when the patient moves from sitting to supine | |||
* Patient in supine: | |||
** Asymmetrical Hip Rotation Range of Motion (ROM) | |||
** Figure of 4 (placing lateral malleoli of the ankle on the contralateral knee) | |||
** Piriformis stretch, knee pulled across body | |||
** Looking for pain, perceived tightness between sides | |||
** The patient can also palpate the anterior bony landmarks of the pelvis in supine | |||
** Other assessments as indicated (self palpation of muscles, other flexibility) | |||
== References == | == References == | ||
<references /> | |||
[[Category:Pelvis]] | |||
[[Category:Pelvis - Assessment and Examination]] | |||
[[Category:Pelvic Health]] | |||
[[Category:Course Pages]] | |||
[[Category:Plus Content]] | |||
Latest revision as of 09:44, 27 December 2022
Top Contributors - Wanda van Niekerk, Tarina van der Stockt, Kim Jackson, Jess Bell and Vidya Acharya
Overview of the Pelvic Girdle Musculoskeletal Methodsm[edit | edit source]
The Pelvic Girdle Musculoskeletal Methodsm (PGM Methodsm) has been developed by Deborah Riczo, a physiotherapist and leading expert in the field of pelvic girdle pain. She has been teaching this method to physiotherapists and physiotherapy assistants since 2011.[1]
Components of the PGM Methodsm[edit | edit source]
The PGMsm method is a holistic approach to pelvic girdle pain and includes the following components[1]:
- Clinical history/pain location
- Special tests
- Tools to use to identify pelvic girdle pain
- Pelvic Girdle Dysfunction: Literature Review
- Pelvic sacral balancing exercises
- Interventions used to correct issues of innominate and sacral positional strain. These include:
- Targeted strengthening exercises
- Targeted stretching exercises
- Interventions used to correct issues of innominate and sacral positional strain. These include:
- Core strengthening
- Patient education
- Consideration of sacroiliac belt
PGMsm Method Special Tests[edit | edit source]
This method includes two sets of special tests to assess dysfunction. For the purpose of this page and the Plus course, Introduction to the PGM method, dysfunction refers to a tendency for a positional strain caused by muscles that are overstrained versus a positional change. The two sets of special tests are:[1]
- Innominate dysfunction cluster of special tests
- Sacral dysfunction special tests
In the PGM method, it is important to screen the innominate first.
Innominate Imbalance Special Tests[edit | edit source]
These are a cluster of 4 special tests and 3 out of 4 of these tests must be positive.[1] The tests are:[1]
- Asymmetrical hip internal rotation (IR) range of motion (>10 degrees between sides)
- Asymmetry/ tenderness of the symphysis pubis
- Unilateral tenderness of ASIS and/or the Iliac Crest
- Unilateral tenderness of PSIS and/or long dorsal sacroiliac ligament
1. Special Test: Asymmetrical Hip Rotation Range of Motion (ROM)[edit | edit source]
- Comparison of hip internal and external range of motion between sides
- Optimal assessment position is prone
- Can be assessed in other positions
- Use an inclinometer or smartphone application to measure the range of motion
- A difference of more than 10° between left and right internal hip rotation is regarded as a positive test result
- Important to assess:
- "Perceived" tightness unilaterally
- Reproduction of symptoms unilaterally during the assessment
Evidence for the Relationship of Hip Range of Motion and Low Back Pain and Pelvic Girdle Dysfunction[edit | edit source]
Ellison et al. (1990)[2] reported differences in hip rotation in patients with low back pain compared to patients without low back pain (controls). The researchers reported that the total hip external rotation was greater than the total hip internal rotation in patients with low back pain. A significant result was a difference of more than 10°.[2]
Cibulka et al. (2002)[3] indicated that the presence of asymmetrical hip rotation range of motion may be an indication of sacroiliac region pain.[3]
Prather et al. (2017)[4] indicated an association between reduced hip internal rotation and low back pain.[4]
Hartigan et al. (2020)[5] investigated hip angles, joint moments and muscle activity during gait in women with self-reported stress urinary incontinence and found the following in this population[5]:
- Weakness, poor endurance and timing of the pelvic floor muscles
- Decreased ability of hip position control in the non-dominant leg
- Decreased strength of the hip abductors and hip external rotators
- Increased gluteus maximus activity of the non-dominant leg
- Women with stress urinary incontinence present with altered hip biomechanics during the stance phase of gait. Although women with stress urinary incontinence seem to be using greater hip abduction and external rotation forces, motor control strategies seem to be lacking and unable to avoid greater hip adduction and internal rotation positions.[5]
Test Reliability[edit | edit source]
Inter- and intra-rater reliability have been established for the measurement of hip internal and external rotation in prone.[2] Measurement of hip internal and external rotation in prone with a goniometer is performed as follows:
Hip internal rotation (IR) and external rotation (ER) are measured with the subject in prone, with the hip in a neutral position and the knees flexed to 90°. The goniometer is centred at the joint line, with the movement arm of the goniometer aligned along the midline of the tibia and the stationary arm aligned perpendicular to the floor.[6] The patient is asked to move the hip into internal rotation while keeping the hips stationary on the table. The patient is then asked to move the hip into external rotation while keeping the hips stationary on the table. Measures are assessed on the contralateral hip as well.
Measurement of hip rotation in prone with a smartphone application (there are various applications available, the method described here is for the Clinometer app) may be done as follows:[7]
The top of the smartphone is placed 3cm below the tibial tuberosity and the base of the smartphone is positioned towards the midline of the medial and lateral malleoli.[6] The patient is asked to move the hip into internal rotation (IR) and then into external rotation (ER). The clinician provides verbal cues to ensure that no compensatory movements occur during the motion.[8] Measures are also assessed on the contralateral limb.
Recent research demonstrated moderate to excellent intra-rater reliability for the measurement of active hip IR and ER when using the goniometer and a smartphone application (Clinometer).[7] Good to excellent interrater reliability was also reported with the measurement of active hip IR and ER with both goniometer and smartphone application. Additionally, it is suggested that the smartphone application may be a valid alternative to hand-held goniometry when measuring active hip IR and ER in clinical practice.[7]
Hip rotation range of motion can also be assessed in sitting as well as in supine in the PGM method.[1]
2. Special Test: Asymmetry/ Tenderness of the Symphysis Pubis[edit | edit source]
Palpation of the Symphysis Pubis[edit | edit source]
The presence of unilateral tenderness with palpation of the symphysis pubis is considered a positive result in the PGM method.[1] The sensitivity (66%) and specificity (99%) of palpation of the anterior surface of the symphysis pubis with the person in supine have been established. The examiner uses palpation to elicit pain that persists for more than 5 seconds after removal of the examiner’s hand.[12]
Anteroposterior or superoinferior displacement of the upper border of the pubic symphysis or pubic tubercle can also be felt with palpation.[13] This may sometimes be more difficult, for example, in the third trimester of pregnancy.[1]
A painful unilateral response on the side that the patient is complaining of the pain is a positive result in the PGM method.[1]
Range of Motion at the Symphysis Pubis[edit | edit source]
Garras et al. (2008)[15] investigated the range of movement at the symphysis pubis by using single-leg stance radiographs. Multiparous women had a significantly increased physiologic range of pubic translation compared to men and nulliparous women. Up to 5 mm of physiologic motion can occur at the pubic symphysis in asymptomatic individuals.[15]
3. Special Test: Unilateral Tenderness of ASIS and/or the Iliac Crest[edit | edit source]
As part of the PGM Method, only unilateral tenderness of the iliac crest and/or the anterior superior iliac spine (ASIS) is assessed and not asymmetry.[1] The standing ASIS asymmetry test has poor reliability and has no value during the examination.[16]
Test Reliability[edit | edit source]
Research has shown a good discriminative ability and inter-rater reliability when two criteria (localised tenderness and pain recognition) were combined.[17] Good interobserver agreement was reported for “localised tenderness” and “typical pain” criteria on iliac crest pain syndrome in patients with non-specific low back pain.[18] McCombe et al. (1989)[19] reported that palpation tests for bony tenderness were more reliable than palpation tests for soft tissue tenderness.[19]
4. Special Test: Unilateral Tenderness of PSIS and/or Long Dorsal Sacroiliac Ligament[edit | edit source]
In the PGM Method, tenderness with palpation of the posterior superior iliac spine (PSIS) and/or the long dorsal sacroiliac ligament on the symptomatic side is considered a positive test result.[1]
Palpation of the Long Dorsal Sacroiliac Ligament[edit | edit source]
The long dorsal sacroiliac ligament is known as a major pain generator for pelvic pain.[21][22] Tenderness with palpation of this ligament does seem to indicate sacroiliac joint pain versus a low back problem. The sensitivity of this palpation test increases when it is combined with the active straight leg raise test and the thrust test.[23]
Sacral Imbalance Special Tests[edit | edit source]
There are two reasons/indications for performing the sacral tests in the PGM Method:[1]
- A negative cluster of PGM signs for the innominate (less than 3 out of 4 positive tests), but the patient has clinical history and symptoms consistent with sacroiliac pelvic girdle pain
- After having completed the interventions for the innominate dysfunction to address the positional strain, the patient’s improve, innominate tests are negative, but the patient is still displaying some clinical signs and complaints of sacroiliac pain or pelvic girdle dysfunction
1. Special Test: Sacral Springing Test[edit | edit source]
This test is similar to the sacral thrust test and involves gross springing of the sacrum. The patient is in prone, the therapist uses the pisiform of their hand and applies a gentle springing of the sacrum. If this relieves the symptoms of the patient, this can be used as a treatment technique. The test is positive if pain is elicited. If no pain is elicited with this test, but pelvic girdle dysfunction is still suspected, move on to assessing each individual pole of the sacrum.[1]
2. Special Test: Springing of Four Poles of Sacrum[edit | edit source]
This test involves the individual springing of the four poles of the sacrum in a similar way that the sacral springing test is performed and is considered positive if pain is present.[1] The four poles of the sacrum are:
- The right and left base of the sacrum
- The right and left inferior lower angles of the sacrum (ILA)
If the patient's symptoms are relieved with the individual springing on a specific pole, this can be used as a treatment technique.
When performing the individual springing on the four different poles it is important to take note of the pain provocation patterns.[1]
Pain Provocation Patterns[edit | edit source]
- Diagonal
- For example, painful with the springing of the right superior pole and the left inferior lateral angle (ILA) of the sacrum - this may indicate a torsion dysfunction[1]
- Vertical
- For example, pain provocation with the springing of the right superior pole and right inferior lateral angle of the sacrum - this may indicate the presence of an "up slip" or a "down slip." This is often best treated with postural type education and manual myofascial releases[1]
- Horizontal
- Pain provocation on both superior poles or inferior lateral angles of the sacrum (ILA) - this is not a torsion or "up slip/down slip" dysfunction and would more likely indicate a positional postural type dysfunction[1]
Virtual Assessment of Pelvic Girdle Dysfunction[edit | edit source]
The COVID-19 pandemic has brought telehealth and virtual patient assessments to the forefront in physiotherapy.[26][27][28] For more info on telehealth and rehabilitation, have a look at these pages:
- Introduction to Telehealth
- Fundamentals of Telehealth Technology
- Telehealth Evaluation
- Practical Considerations in Telehealth
- The basics of Telehealth Assessment and Treatment
- Ethical and Professional Considerations with Telehealth
Recommendations for Virtual Consultation[edit | edit source]
Here are some recommendations on what and how to assess pelvic girdle dysfunction virtually:[1]
Initial screening
Rule out centralisation with the McKenzie approach (repeated back extensions or prone press-ups). If the patient's symptoms centralise, initial treatment should be focused on the lumbar spine before further assessment using the PGM Method.
PGM Method screening
- Patient in standing (Special Tests 2-4):
- Assess unilateral tenderness or pain with palpation of ASIS/iliac crest
- Assess unilateral tenderness or pain with palpation of symphysis pubis
- Assess unilateral tenderness or pain of the PSIS/long dorsal sacroiliac ligament
- Patient in sitting (Special Test 1):
- Asymmetrical hip rotation range of motion (ROM)
- The patient can place the lateral malleoli of the ankle on the contralateral knee (figure of 4 - examining external rotation of the hip)
- From the previous position, the patient can bring the leg across the body and assess pain with this movement (moving hip into internal rotation)
- Knee to chest
Transitional movements should be assessed when the patient moves from sitting to supine
- Patient in supine:
- Asymmetrical Hip Rotation Range of Motion (ROM)
- Figure of 4 (placing lateral malleoli of the ankle on the contralateral knee)
- Piriformis stretch, knee pulled across body
- Looking for pain, perceived tightness between sides
- The patient can also palpate the anterior bony landmarks of the pelvis in supine
- Other assessments as indicated (self palpation of muscles, other flexibility)
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 Riczo, D. Introduction to the Pelvic Girdle Musculoskeletal Method Course. Plus , 2021.
- ↑ 2.0 2.1 2.2 Barbee Ellison J, Rose SJ, Sahrmann SA. Patterns of hip rotation range of motion: a comparison between healthy subjects and patients with low back pain. Physical therapy. 1990 Sep 1;70(9):537-41.
- ↑ 3.0 3.1 Cibulka MT. Understanding sacroiliac joint movement as a guide to the management of a patient with unilateral low back pain. Manual Therapy. 2002 Nov 1;7(4):215-21.
- ↑ 4.0 4.1 Prather H, Cheng A, Steger-May K, Maheshwari V, Van Dillen L. Hip and lumbar spine physical examination findings in people presenting with low back pain, with or without lower extremity pain. journal of orthopaedic & sports physical therapy. 2017 Mar;47(3):163-72.
- ↑ 5.0 5.1 5.2 Hartigan E, McAuley JA, Lawrence M, Brucker W, King A, Tryon B, DeSilva M. Hip Angles, Joint Moments, and Muscle Activity During Gait in Women With and Without Self-reported Stress Urinary Incontinence. Journal of Women’s Health Physical Therapy. 2020 Jul 1;44(3):107-16.
- ↑ 6.0 6.1 Charlton PC, Mentiplay BF, Pua YH, Clark RA. Reliability and concurrent validity of a Smartphone, bubble inclinometer and motion analysis system for measurement of hip joint range of motion. Journal of Science and Medicine in Sport. 2015 May 1;18(3):262-7.
- ↑ 7.0 7.1 7.2 Miley E, May J, Albertin E, Takahashi E, Goodman C, Pettaway A. Reliability and Validity for Measuring Active Hip Rotation with the Clinometer Smartphone Application™. Journal of Rehabilitation Sciences & Research. 2019 Dec 1;6(4):193-9.
- ↑ Cheatham S, Hanney WJ, Kolber MJ. Hip range of motion in recreational weight training participants: a descriptive report. International Journal of Sports Physical Therapy. 2017 Oct;12(5):764.
- ↑ ATX Physical Therapy. Prone hip external and internal rotation assessment. Available from https://vimeo.com/399220225 (last accessed 3 January 2021)
- ↑ MCCCPTAP. Hip IR and ER ROM with a goniometer. Available from https://www.youtube.com/watch?v=jFBD1wZvXIc (last accessed 3 January 2021)
- ↑ FITT. 19 Medial Hip Rotation Goni. Available from https://www.youtube.com/watch?v=0MQ01JbJOGs (last accessed 3 January 2021)
- ↑ Albert H, Godskesen M, Westergaard J. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. European Spine Journal. 2000 Apr 1;9(2):161-6.
- ↑ Jain S, Eedarapalli P, Jamjute P, Sawdy R. Symphysis pubis dysfunction: a practical approach to management. The Obstetrician & Gynaecologist. 2006 Jul;8(3):153-8.
- ↑ Orthopedic Physical Examination Tests. Pubic symphysis palpation. Available from https://www.youtube.com/watch?v=JKuBjqbzpc8. (last accessed 3 January 2021)
- ↑ 15.0 15.1 Garras DN, Carothers JT, Olson SA. Single-leg-stance (flamingo) radiographs to assess pelvic instability: how much motion is normal?. JBJS. 2008 Oct 1;90(10):2114-8.
- ↑ Cook C, Hegedus E. Orthopedic Physical Examination Tests: An Evidence-Based Approach. 2nd ed. Prentice Hall; 2012
- ↑ Njoo KH, Van der Does E. The occurrence and inter-rater reliability of myofascial trigger points in the quadratus lumborum and gluteus medius: a prospective study in non-specific low back pain patients and controls in general practice. Pain. 1994 Jan 1;58(3):317-23.
- ↑ Njoo KH, Van der Does E, Stam HJ. Interobserver agreement on iliac crest pain syndrome in general practice. The Journal of rheumatology. 1995 Aug 1;22(8):1532-5.
- ↑ 19.0 19.1 McCombe PF, Fairbank JC, Cockersole BC, Pynsent PB. 1989 Volvo Award in clinical sciences. Reproducibility of physical signs in low-back pain. Spine. 1989 Sep 1;14(9):908-18.
- ↑ SapiensMove_PT_Videos. Anterior and Lateral Hip & Pelvis Palpation. Available from https://www.youtube.com/watch?v=dCzuLb3Cng8&t=125s (last accessed 3 January 2021)
- ↑ Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, Stoeckart R, Snijders CJ, Mens JM. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996 Mar 1;21(5):556-62.
- ↑ Vleeming A, De Vries HJ, Mens JM, Wingerden JP. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta obstetricia et gynecologica Scandinavica. 2002 Jan 1;81(5):430-6.
- ↑ Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal. 2008 Jun 1;17(6):794-819.
- ↑ SapiensMoves_PT_Videos. Posterior Pelvis & Lumbar Palpation. Available from https://www.youtube.com/watch?v=ers5kA9vK_o (last accessed 3 January 2021)
- ↑ Thomasz Grass. Sacral Spring Test. Available from https://www.youtube.com/watch?v=zySIMEn3u7w (last accessed 3 January 2021)
- ↑ Bennell KL, Lawford BJ, Metcalf B, Mackenzie D, Russell T, van den Berg M, et al. Physiotherapists and patients report positive experiences overall with telehealth during the COVID-19 pandemic: a mixed-methods study. J Physiother. 2021 Jul;67(3):201-9.
- ↑ Brigo E, Rintala A, Kossi O, Verwaest F, Vanhoof O, Feys P, Bonnechère B. Using telehealth to guarantee the continuity of rehabilitation during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2022 Aug 19;19(16):10325.
- ↑ Haines KJ, Sawyer A, McKinnon C, Donovan A, Michael C, Cimoli C, et al. Barriers and enablers to telehealth use by physiotherapists during the COVID-19 pandemic. Physiotherapy. 2022 Sep 7;118:12-9.