The Flag System: Difference between revisions
No edit summary |
Rachael Lowe (talk | contribs) No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
Yellow flags are psychosocial indicators suggesting increased risk of progression to long-term distress, disability and [[Clinical Pain Presentations|pain]]. [[Image:YellowFlag1.jpg|thumb|right]] | |||
=== Yellow Flags === | |||
Flags in Physiotherapy are a marker of risk factors regarding musculoskeletal diseases and disorders. Yellow Flags are an indication of Psychosocial factors (Depression, Anxiety etc..) and the patient’s beliefs about their condition .<br>While performing a Yellow Flag assessment, the following should be acknowledged: | |||
<br>'''A'''ttitudes/Beliefs – What does the patient think to be the problem and do they have a positive or negative attitude to the pain and potential treatment?<br>'''B'''ehaviour – Has the patient changed their behaviour to the pain? Have they reduced activity or compensating for certain movements. Early signs of catastrophising and fear-avoidance?<br>'''C'''ompensation – Are they awaiting a claim due to a potential accident? Is this placing unnecessary stress on their life? .<br>'''D'''iagnosis/Treatment – Has the language that has been used had an effect on patient thoughts? Have they had previous treatment for the pain before, and was there a conflicting diagnosis? This could cause the patient to over-think the issue, leading to catastrophising and fear-avoidance.<br>'''E'''motions – Does the patient have any underlying emotional issues that could lead to an increased potential for chronic pain? Collect a thorough background on their psychological history.<br>'''F'''amily – How are the patient’s family reacting to their injury? Are they being under-supportive or over-supportive, both of which can effect the patient’s concept of their pain<br>'''W'''ork – Are they currently off work? Financial issues could potentially arise? What are the patient’s thoughts about their working environment? | |||
<br> | |||
Another psychological issue associated with CLBP is catastrophizing. This is outlined through the Fear Avoidance Model (Shown Below). | |||
=== Fear-Avoidance Model === | |||
Fear is the emotional reaction to a specific, identifiable and immediate threat, such as a dangerous injury <ref name="Rachman 1998">Rachman, S., 1998. Anxiety. Psychological Press: Hove</ref>. Fear may protect the individual from impeding danger as it instigates the defensive behaviour that is associated with the fight or flight response <ref name="Cannon 1929">Cannon, W. B., 1929. Bodily changes in pain, hunger, fear and rage: an account of recent researches into the functions of emotional excitement. Appleton-Century-Crofts, New York</ref>.<br>The Fear-Avoidance Model was designed to identify and explain why chronic low back pain problems, and associated disability, develop in members of the population suffering from an onset of low back pain <ref name="Leeuw et al,. 2007">Leeuw, M., Goossens, E.J.B., Linton, S., Crombez, G., Boersma, K., Vlaeyen, J., 2007. The Fear-Avoidance Model of Musculoskeletal Pain: Current State of Scientific Evidence. Journal of Behavioural Medicine, 30(1): 77-94</ref>. This model indicates that a person suffering from pain will undergo one of two different pathways (Fig.1).<br> | |||
[[Image:Pain fear.jpg|center|Fig.1 Fear Avoidance Model]] | |||
Fig.1 Fear Avoidance Model <ref name="Fear avoidance 2014">www.psychomaticmedicine.org (2014) Fear Avoidance Model (photograph). Available at: http://www.psychosomaticmedicine.org/cgi/content-nw/full/67/5/783/F117 (Accessed 11th January 2014)</ref> | |||
This shows that when pain/injury occurs, people will take the path of continuing their independence without negative thoughts of the pain they are suffering from, therefore leading them to accept that they have this pain that ultimately accumulates to a faster recovery. In contrast to this, a cycle can be initiated if the pain is misinterpreted in a catastrophising manner. It has been recognised that these thoughts can lead on to pain-related fear and associated safety seeking behaviours, such as avoidance. However, this could cause the pain to become worse and enter a chronic phase due to the disuse and disability. This in turn can lower the threshold at which the person will experience pain.<br> | |||
== Stepped care approach == | |||
People with pain require: | People with pain require: | ||
| Line 15: | Line 37: | ||
*the opportunity and encouragement to return to normal physical activity | *the opportunity and encouragement to return to normal physical activity | ||
In addressing the factors above, the difference between treatment and rehabilitation becomes clearer but must still take into account the barriers to rehabilitation. These are the non-physical or clinical factors that are important to determine recovery and failure to address them can lead to a suboptimal outcome, no matter how technically good you are as a clinician (Waddell & Watson, 2004). | In addressing the factors above, the difference between treatment and rehabilitation becomes clearer but must still take into account the barriers to rehabilitation. These are the non-physical or clinical factors that are important to determine recovery and failure to address them can lead to a suboptimal outcome, no matter how technically good you are as a clinician (Waddell & Watson, 2004). | ||
Von Korff and Moore (2001) advocate a stepped care approach, evident in the following table: | Von Korff and Moore (2001) advocate a stepped care approach, evident in the following table: | ||
| Line 45: | Line 65: | ||
*Psycho (psychological distress, fear/avoidance beliefs, current coping methods and attribution) | *Psycho (psychological distress, fear/avoidance beliefs, current coping methods and attribution) | ||
*Social (work issues, family circumstances and benefits/economics) | *Social (work issues, family circumstances and benefits/economics) | ||
Key predictors include: | Key predictors include: | ||
| Line 59: | Line 77: | ||
<rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1tmbGqZ-sGnYR-hI6lOB0IW_LNudiGf6mTz3KNoONOlQpn0MYh|charset=UTF-8|short|max=10</rss> | <rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1tmbGqZ-sGnYR-hI6lOB0IW_LNudiGf6mTz3KNoONOlQpn0MYh|charset=UTF-8|short|max=10</rss> | ||
<br> | |||
== References == | == References == | ||
<references /> | <references /> | ||
<ref name="BMJ">BMJ (2003) CHRONIC LOW BACK PAIN [ONLINE] AVAILABLE AT &lt; http://www.bmj.com/content/326/7388/535&gt;</ref><br></div> | |||
<ref name="BMJ">BMJ (2003) CHRONIC LOW BACK PAIN [ONLINE] AVAILABLE AT < http://www.bmj.com/content/326/7388/535></ref><br> | |||
Revision as of 15:13, 23 February 2014
Original Editor - The Open Physio project.
Top Contributors - Admin, Faye Underwood, Rachael Lowe, Scott Buxton, Kim Jackson, Naomi O'Reilly, WikiSysop, Simisola Ajeyalemi, Jess Bell, 127.0.0.1, Venus Pagare, Adam Vallely Farrell, Luke Dinan, Claire Knott and Amanda Ager
Introduction[edit | edit source]
Yellow flags are psychosocial indicators suggesting increased risk of progression to long-term distress, disability and pain.
Yellow Flags[edit | edit source]
Flags in Physiotherapy are a marker of risk factors regarding musculoskeletal diseases and disorders. Yellow Flags are an indication of Psychosocial factors (Depression, Anxiety etc..) and the patient’s beliefs about their condition .
While performing a Yellow Flag assessment, the following should be acknowledged:
Attitudes/Beliefs – What does the patient think to be the problem and do they have a positive or negative attitude to the pain and potential treatment?
Behaviour – Has the patient changed their behaviour to the pain? Have they reduced activity or compensating for certain movements. Early signs of catastrophising and fear-avoidance?
Compensation – Are they awaiting a claim due to a potential accident? Is this placing unnecessary stress on their life? .
Diagnosis/Treatment – Has the language that has been used had an effect on patient thoughts? Have they had previous treatment for the pain before, and was there a conflicting diagnosis? This could cause the patient to over-think the issue, leading to catastrophising and fear-avoidance.
Emotions – Does the patient have any underlying emotional issues that could lead to an increased potential for chronic pain? Collect a thorough background on their psychological history.
Family – How are the patient’s family reacting to their injury? Are they being under-supportive or over-supportive, both of which can effect the patient’s concept of their pain
Work – Are they currently off work? Financial issues could potentially arise? What are the patient’s thoughts about their working environment?
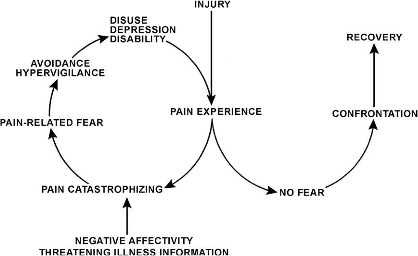
Another psychological issue associated with CLBP is catastrophizing. This is outlined through the Fear Avoidance Model (Shown Below).
Fear-Avoidance Model[edit | edit source]
Fear is the emotional reaction to a specific, identifiable and immediate threat, such as a dangerous injury [1]. Fear may protect the individual from impeding danger as it instigates the defensive behaviour that is associated with the fight or flight response [2].
The Fear-Avoidance Model was designed to identify and explain why chronic low back pain problems, and associated disability, develop in members of the population suffering from an onset of low back pain [3]. This model indicates that a person suffering from pain will undergo one of two different pathways (Fig.1).
Fig.1 Fear Avoidance Model [4]
This shows that when pain/injury occurs, people will take the path of continuing their independence without negative thoughts of the pain they are suffering from, therefore leading them to accept that they have this pain that ultimately accumulates to a faster recovery. In contrast to this, a cycle can be initiated if the pain is misinterpreted in a catastrophising manner. It has been recognised that these thoughts can lead on to pain-related fear and associated safety seeking behaviours, such as avoidance. However, this could cause the pain to become worse and enter a chronic phase due to the disuse and disability. This in turn can lower the threshold at which the person will experience pain.
Stepped care approach[edit | edit source]
People with pain require:
- a rationale for returning to activity
- an appropriate strategy to manage their symptoms
- a safe environment to engage in physical exercise to restore confidence in movement
- the opportunity and encouragement to return to normal physical activity
In addressing the factors above, the difference between treatment and rehabilitation becomes clearer but must still take into account the barriers to rehabilitation. These are the non-physical or clinical factors that are important to determine recovery and failure to address them can lead to a suboptimal outcome, no matter how technically good you are as a clinician (Waddell & Watson, 2004).
Von Korff and Moore (2001) advocate a stepped care approach, evident in the following table:
| 1. | Most patients who are at the acute stage | Identify and address the common worries of patients with back pain using simple, symptomatic measures. Provide information and advice to encourage the resumption of ordinary activities. |
| 2. |
The substantial minority of patients who do not resume ordinary activities by 3-6 weeks with simple advice. |
Provide brief, structured interventions that help patients to identify obstacles to recovery, set functional goals and develop plans to achieve them. Provide support for physical exercise and return to ordinary activities |
| 3. | The small minority of patients who have persisting disability in work or family life and who require more intensive intervention. | Address dysfunctional beliefs and behaviour. Provide a progressive exercise or graded activity programme. Enable and support patients to return to ordinary activities. |
Predictors of chronic disability[edit | edit source]
A biopsychosocial assessment should seek to identify the following:
- Bio (triage and identification of the pathology)
- Psycho (psychological distress, fear/avoidance beliefs, current coping methods and attribution)
- Social (work issues, family circumstances and benefits/economics)
Key predictors include:
- The belief that pain is harmful or severely disabling
- Fear-avoidance behaviour (avoiding activity because of fear of pain)
- Low mood and social withdrawal
- Expectation that passive treatment rather than active participation will help
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1tmbGqZ-sGnYR-hI6lOB0IW_LNudiGf6mTz3KNoONOlQpn0MYh|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ Rachman, S., 1998. Anxiety. Psychological Press: Hove
- ↑ Cannon, W. B., 1929. Bodily changes in pain, hunger, fear and rage: an account of recent researches into the functions of emotional excitement. Appleton-Century-Crofts, New York
- ↑ Leeuw, M., Goossens, E.J.B., Linton, S., Crombez, G., Boersma, K., Vlaeyen, J., 2007. The Fear-Avoidance Model of Musculoskeletal Pain: Current State of Scientific Evidence. Journal of Behavioural Medicine, 30(1): 77-94
- ↑ www.psychomaticmedicine.org (2014) Fear Avoidance Model (photograph). Available at: http://www.psychosomaticmedicine.org/cgi/content-nw/full/67/5/783/F117 (Accessed 11th January 2014)
- ↑ BMJ (2003) CHRONIC LOW BACK PAIN [ONLINE] AVAILABLE AT < http://www.bmj.com/content/326/7388/535>