Template:PCPP
Original Editors - <a href="Pathophysiology of Complex Patient Problems">Students from Bellarmine University's Pathophysiology of Complex Patient Problems project.</a>
Top Contributors - <img class="FCK__MWTemplate" src="http://www.physio-pedia.com/extensions/FCKeditor/fckeditor/editor/images/spacer.gif" _fckfakelement="true" _fckrealelement="1" _fck_mw_template="true">
Definition/Description[edit source]
Cellulitis
Prevalence[edit source]
- 650,000 hospital admissions per year in the United States are due to Cellulitis.4
- When hospitalized, patients with recurrent cellulitis require longer hospitalizations relative to nonrelapsing Cellulitis patients.4
- From 1998-2006, 10% of all infectious-disease hospitalizations were related to Cellulitis4
- 22-49% of patients who have cellulitis report at least one previous episode4
- Recurrences, typically in the same location, occur approximately 14% of cellulitis cases within 1 year and in 45% of cases within 3 years4
Characteristics/Clinical Presentation[edit source]
Typical symptoms include acute poorly demarcated and spreading erythema along with pain, swelling, and warmth of the lower extremity but can occur on any area of skin or underlying subcutaneous tissue.2,3 Additional symptoms may include fever, nausea, vomiting, and rigors.3,10 Other features include proximal dilated and edematous skin lymphatics and bulla formation.3 Cellulitis predominantly has a unilateral presentation.3
Associated Co-morbidities[edit source]
add text here
Medications[edit source]
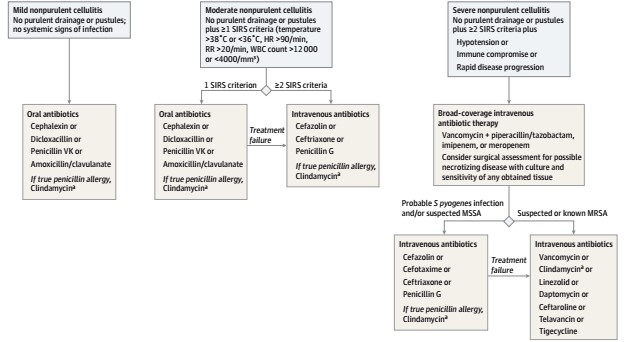
Cephalexin, Dicloxacillin, Penicillin VK, Amoxicillin, and Clindamycin are typical Antistreptococcal Antimicrobial agents for the treatment of typical cellulits that is considered mild and does not show signs of systemic involvement.3 Figure 1 states which medications would be appropriate based on the severity of symptoms and the risk of Methicillin-resistant Staphylococcus aureus (MRSA).4
| Clinical Presentation | Appropriate Antibiotic Treatment |
|---|---|
| Routine Cellulitis with low suspicion of MRSA | Dicloxacillin, Cephalexin, Nafcillin, or Cefazolin |
| High suspicion of MRSA or Penicillin allergy | Doxycycline, Clindamycin, Trimethoprim-sulfamethoxazole |
| High suspicion of MRSA with signs and symptoms of severe infection or did not respond to initial routine treatment | Vancomycin*, Linezolid |
- Vancomycin is the drug of choice for infections resulting from MRSA4
Diagnostic Tests/Lab Tests/Lab Values[edit source]
Cellulitis is most commonly diagnosed by history and physical examination alone. Certain laboratory tests can indicate the presence of infection, but are not specific to cellulitis alone. Elevated white blood cell count, C-reactive protein, and erythrocyte sedimentation rate are the most common laboratory results in people with cellulitis, though the prevalence of these results varies widely on a case by case basis. Imaging studies can identify more severe infections to differentiate from cellulitis, but are not a reliable diagnostic tool for cellulitis itself. (3)
Cultures are typically not beneficial in making a cellulitis diagnosis. Identification of the cause of the infection through blood, needle aspiration or punch biopsy are not recommended unless the patient has a complication or abnormal exposure history. This would include immunosuppressants, a diagnoses of chronic liver disease, aquatic soft tissue injury, animal and human bites, or being in contact with various bacteria.3 If a biopsy and culture is warranted, a histopathologic evaluation will be performed on the sample. Hematoxylin-and-eosin and certain stainings for organisms, bacteria, fungi, and microbacteria will be included. 8
Etiology/Causes[edit source]
add text here
Systemic Involvement[edit source]
add text here
Medical Management (current best evidence)[edit source]
Currently, there are no published national guidelines for the treatment of cellulitis.5 Most common management of the infection is administration of antibiotics. In more severe cases of cellulitis, intravenous antibiotics can be used.8 Elevation and compression of the affected area promotes drainage of edema and can reduce inflammation, speeding up recovery.8
For those with recurrent cellulitis, prophylactic antibiotic therapy is an option. Recent studies show that antibiotic prophylaxis substantially reduced the number or recurrences experienced by patients while actively taking the medication. Although there is reduction during the antibiotic therapy, there is no evidence of persistent protect effect after it has ceased.1
In regards to those patients with recurrent cellulitis due to lymphedema, decongestive therapy including manipulation of the lymphatic system through massage, has shown to reduce the recurrence of cellulitis.9
This flow chart is a treatment algorithm based on the type of cellulitis a patient is diagnosed with from: Raff AB, Kroshinsky D. Cellulitis: A Review. JAMA. 2016;316(3):325-37.
http://jamanetwork.com/pdfaccess.ashx?url=/data/journals/jama/935437/
Physical Therapy Management (current best evidence)[edit source]
add text here
Differential Diagnosis[edit source]
add text here
Case Reports/ Case Studies[edit source]
add links to case studies here (case studies should be added on new pages using the <a href="Template:Case Study">case study template</a>)
Resources
[edit source]
add appropriate resources here
Recent Related Research (from <a href="http://www.ncbi.nlm.nih.gov/pubmed/">Pubmed</a>)[edit source]
see tutorial on <a href="Adding PubMed Feed">Adding PubMed Feed</a>
addfeedhere|charset=UTF-8|short|max=10
References[edit source]
see <a href="Adding References">adding references tutorial</a>.
<span class="fck_mw_references" _fck_mw_customtag="true" _fck_mw_tagname="references" />
<a _fcknotitle="true" href="Category:Bellarmine_Student_Project">Bellarmine_Student_Project</a>