Subacromial Pain Syndrome
Original Editor - David Drinkard, Dorien De Strijcker
Lead Editors
Definition/Description[edit | edit source]
Subacromial (SA) impingement is defined as the mechanical compression of subacromial structures between the coraco-acromial arch and the humerus during active elevation of the arm above shoulder height.
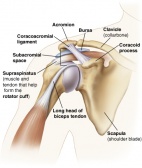
Clinically Relevant Anatomy[edit | edit source]
Structures involved in subacromial impingment:
- the coracoacromial arch[1] composed of acromion, processus coracoideus and ligamentum coracoacromiale
- the humerus
- the tendons of the Rotator Cuff
- the long head of de m. biceps brachii
- the subacromial bursa[2]
- shoulder capsule
The subacromial space is the margin between the superior portion of the humeral head and the inferior portion of the acromion. It contains:
- belly and tendon of the supraspinatus muscle
- long head of the biceps muscle
- subacromial bursa
The shape of the acromion plays an important role in impingment syndromes. 3 types of acromial shape can be distinguished:[1]
- Type I acromion: flat shape
- Type II acromion: curved shape
- Type III acromion: hooked shape (most likely to contribute to impingement and irritation)
Bony spurs at the bottom aspect of the acromion can also be involved.
Epidemiology /Etiology[edit | edit source]
Impingement syndrome occurs in one out of three persons, half of whom still report pain after three years.
Subacromial impingement occurs when the subacromial space is narrowed and weak structures in that space get compressed. Several causes for subacromial impingment have been detected: [3]
- Anatomical variations such as narrow SA space, type II or III acromion, osteophytes.
- Rotator cuff weakness, causing the humeral head to drift more superior.
- Chronic rotator cuff irritation due to overuse.
- Posterior GH capsule tightness
- Poor posture (forward shoulder posture can cause functional narrowing of SA space)
- Abnormal muscle activation
Mentioned biomedical aspects but also psychological factors as kinesiophobia or catastrophizing can have negative influence and thus cause chronic pain and disability. [4]
Clinical Presentation[edit | edit source]
The shoulder pain during active elevation of the arm is usually reported at the anterior or lateral side of the shoulder. Activities performed with the involved arm below shoulder level are mostly not painful. [3]
Onset is more of a gradual, degenerative condition rather than due to a strong external force. Therefore, patients have difficulty determining the exact time of onset.
- First stage:
Moderate pain during exercise
No loss of strength
No limitation in movement
- Second stage:
Pain during ADL-activities and especially during the night
Loss of mobility
- Third stage:
Strong restriction in movement due to calcifications
Loss of muscle strength
Diagnostic Procedures[edit | edit source]
Diagnosis should be based on: [4]
- History
- Clinical examination
- X-rays
- MRI
History and clinical examination are imparitive. X-rays may be used as an extra test detect sclerosis and osteophyte-formation on the acromion. The size of the subacromial space can also be measured. MRI can show full or partial tears in the tendons of the rotator cuff, cracks in the capsule and inflammation to weak structures.
Examination[edit | edit source]
Also see Impingement Cluster page
Following tests help to confirm or rule out subacromial impingment syndrome: [5]
- Hawkins-Kennedy
- Neer impingement test (useful screening test to rule out SAI)
- Painful Arc (between 60° and 120°) (useful screening and helpful confirming test to rule out SAI)
- Empty can (Jobe) (helpful test to confirm SAI)
- External rotation resistance tests (useful screening and helpful confirming test to rule out SAI)
Cluster[edit | edit source]
Individual special tests for sub-acromial impingement have varying psychometric properties. For this reason, it is best to utilize special test clusters in order to diagnose this injury. Two special test clusters are provided below that can be used in order to diagnose sub-acromial impingement[6].
| Sensitivity | Specificity | Accuracy% | PPV% | NPV% | |
| Hawkins-Kennedy | .92 | .25 | 72.8 | 75.2 | 56.2 |
| Neers | .89 | .31 | 72.0 | 75.9 | 52.3 |
| Horizontal-adduction | .82 | .28 | 66.4 | 73.7 | 38.4 |
| Speed | .69 | .56 | 64.8 | 79.2 | 41.6 |
| Yergason | .37 | .86 | 51.2 | 86.8 | 35.6 |
| Painful arc | .33 | .81 | 46.4 | 80.5 | 32.5 |
| Drop arm | .08 | .97 | 33.6 | 87.5 | 29.9 |
A total of 5 positive special tests is indicative for subacromial impingement[6].
| Positive tests | Sensitivity | Specificity | Accuracy% | PPV% | NPV% |
| All positive | .04 | .97 | 31.2 | 80.0 | 29.1 |
| ≥6 positive | .30 | .89 | 47.2 | 87.0 | 34.0 |
| ≥5 positive | .38 | .86 | 52.0 | 87.1 | 36.0 |
| ≥4 positive | .70 | .67 | 68.8 | 83.7 | 47.0 |
| ≥3 positive | .84 | .44 | 72.8 | 72.8 | 44.4 |
Accuracy: The percentage of time that the result of the test reflects the true nature of the condition
A second cluster utilizes a slightly different set of special tests[7].
| Sensitivity | Specificity | Positive LR | Negative LR | |
| Hawkins-Kennedy | .63 | .62 | 1.63 | .61 |
| Neers | .81 | .54 | 1.17 | .35 |
| Painful arc | .75 | .67 | 2.25 | .38 |
| Empty can | .50 | .87 | 3.90 | .57 |
| External rotation resistance | .56 | .87 | 4.39 | .50 |
Any combination of 3 or more positive tests are indicative of sub-acromial impingement[7]
| Sensitivity | Specificity | Positive LR | Negative LR | |
| 3+ positive tests | .75 | .74 | 2.93 | .34 |
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Medical Management (current best evidence)[edit | edit source]
Several surgical techniques are available, depending on the character and severity of the injury:
- Surgical repair of torn tissues, mostly of supraspinatus muscle, long head of biceps tendon or joint capsule.
- Bursectomy or removal of the subacromial bursa.
- Subacromial decompression to increase the subacromial space by removing bony spurs or the coracoacromial ligament
- Acromioplasty to increase the subacromial space by removing a part of the acromion. Arthroscopic acromioplasty is less invasive and requires lesser rehabilitation than the open (Neer) acromioplasty.
Physical Therapy Management (current best evidence)[edit | edit source]
There is strong evidence that non-operative rehabilitation - when supervised - both decreases pain in the shoulder and increase function. [2] Non-operative treatment should therefor be attempted first, assuming there is no tear that requires surgery. No data guarantee that surgical treatment is more effective than conservative treatment.
Several conservative treatments are available: [8]
- RICE therapy in the acute phase to reduce pain and swelling
- NSAIDS or nonsteroidal anti-inflammatory drugs
- Corticosteroid injections
- Physical therapy
- Manual therapy techniques of the shoulder that have a significant effect on decreasing pain levels.
- Acupuncture
- Electrical stimulation
- Ultrasound
- Low-level laser therapy has positive effects on all symptoms except on muscle strength. [9]
Although exercise therapy alone has prooved efficiency, the addition of manual therapy insures further increase in muscle strength. [10] Exercise therapy is a vital part of treatment for subacromial impingement but results showed no significant difference between home-based exercises and clinical exercise.
Therapeutic exercise should include: [11]
- rotator cuff strengthening
- lower and middle trapezius strengthening
- anterior and posterior shoulder stretching.
Strengthening of the lower part of the trapezius muscle is an important part of exercise therapy. Individuals with impingement syndrome show greater ratios of upper and lower trapezius activity than asymptomatic individuals. [12] Soft tissue mobilization to normalize muscle spasm and other soft tissue dysfunction has been shown to be effective alongside joint mobilizations to restore motion in treatment of SAI. [12]
Differential Diagnosis
[edit | edit source]
There are a variety of shoulder conditions that can initially be confused with subacromial impingement, although a thorough examination is usually sufficient for identifying this condition.
Partial and full rotator cuff tears are or rotator cuff tendinitis are often the result of subacromial impingement syndrome, but can occur without impingement and usually demonstrate some sort of lag sign upon evaluation.
Adhesive capsulitis, or "frozen shoulder", can also present with limitation of active arm elevation and significant shoulder pain; however, adhesive capsulitis usually presents with glenohumeral motion loss in a capsular pattern, meaning that external rotation and abduction are the two directions with the greatest magnitude of motion lost.
Further on, calcific tendinitis and an acute or chronic inflammation of the bursa subacromialis could be differential diagnosis, as well as a subluxating shoulder or thoracic outlet syndrome. [3]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Presentations[edit | edit source]
Alice Thompson. Shoulder Impingement An insight into the causes, clinical presentation, assessment and treatment of shoulder impingement. A reference for physiotherapists. 2012
Read 4 Credit[edit | edit source]
|
Would you like to earn certification to prove your knowledge on this topic? All you need to do is pass the quiz relating to this page in the Physiopedia member area.
|
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1VsHRGSo3HXVCiE3YsXdoVtjngMaV1dlFS8HD8_1UNglqkq9z-|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ 1.0 1.1 Kachingwe AF, Phillips B, Sletten E, Plunkett SW. Comparison of Manual Therapy Techniques with Therapeutic Exercise in the Treatment of Shoulder Impingement: A Randomized Controlled Pilot Clinical Trial. The Journal of Manual fckLRManipulative Therapy 2008;16(4):238-‐247
- ↑ 2.0 2.1 TATE A.R., MCCLURE P.W., YOUNG I.A., SALVATOR R., MICHENER L.A. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. The Journal of orthopaedic and sports physical therapy. 2010 Aug; 40(8): 474-93
- ↑ 3.0 3.1 3.2 BIRRER R.B., O’CONNOR F.G. Sports medicine for the primary care physician. 3rd edition, Boca Raton: RCR PRESS, 2004.p507- 10
- ↑ 4.0 4.1 DE BIE R.A., BASTIANENEN C.H.G. Effectiveness of individualized physiotherapy on pain and functioning compared to a standard exercise protocol in patients presenting with clinical signs of subacromial impingement syndrome. A randomized controlled trial. BMC Musculoskeletal Disorders. 2010 Jun 9; 11:114
- ↑ MICHENER L.A., WALSWORTH M.K., DOUKAS W.C., MURPHY K.P. Reliability and Diagnostic Accuracy of 5 Physical Examination Tests and Combination of Tests for Subacromial Impingement. Archives of Physical Medicine and Rehabilitation. 2009 Nov; 90(11): 1898-903
- ↑ 6.0 6.1 Caliş M, Akgün K, Birtane M, Karacan I, Caliş H, Tüzün F. Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome. Ann Rheum Dis. 2000 Jan;59(1):44-7.
- ↑ 7.0 7.1 Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009 Nov;90(11):1898-903.
- ↑ DORRESTIJN O., STEVENS M., WINTERS J.C., VAN DER MEER C.,DIERCKS R.l. Conservative or surgical treatment for subacromial impingement syndrome? A systematic review.Journal of shoulder and elbow surgery board of trustees.2009 Jul-Aug;18(4):652-60
- ↑ YELDAN I., CETIN E., OZDINCLER A.R. The effectiveness of low-level laser therapy on shoulder function in subacromial impingement syndrome. Disability and rehabilitation. 2009; 31(11): 935–940
- ↑ Bang MD, Deyle GD. Comparison of Supervised Exercise With and Without Manual Physical Therapy for Patients with Shoulder Impingement Syndrome. Journal of Orthopaedic and Sports Physical Therapy. 2000;30(3):126-137
- ↑ Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and synthesized evidence-based rehabilitation protocol. Journal fo Shoulder and Elbow Surgery. 2009;18:138-160
- ↑ 12.0 12.1 Smith M, Sparkes V, Busse M, Enright S. Upper and Lower trapezius muscle activity in subjects with subacromial impingement symptoms: Is there imbalance and can taping change it? Physical Therapy in Sport. 2009:10, 45-50