Stroke Medical Management: Difference between revisions
No edit summary |
No edit summary |
||
| Line 106: | Line 106: | ||
tPA is no different from other medications in that it has potential adverse effects, which makes it essential that a careful consideration is given to exclusion criteria, risks and benefits for use in each individual patient. The major complications is symptomatic intracranial hemorrhage which occurs at a rate of roughly 5.2%. Other complications include orolingual angioedema (allergic reaction), acute hypotension, and systemic bleeding. (Circulation 2010: Part 11: Adult Stroke).<br> | tPA is no different from other medications in that it has potential adverse effects, which makes it essential that a careful consideration is given to exclusion criteria, risks and benefits for use in each individual patient. The major complications is symptomatic intracranial hemorrhage which occurs at a rate of roughly 5.2%. Other complications include orolingual angioedema (allergic reaction), acute hypotension, and systemic bleeding. (Circulation 2010: Part 11: Adult Stroke).<br> | ||
=== Thrombectomy === | === Thrombectomy === | ||
Clot retrieval devices: There are currently four FDA- approved devices for clot disruption or removal.<br>The Mechanical Embolus Removal in Cerebral Ischemia (MERCI) Thrombectomy System is a looped wire with progressively smaller helical loops, advanced via a small catheter through the clot. As the catheter is withdrawn, the coiled wire is deployed, which captures the clot for removal. | |||
The Penumbra Thrombectomy System is designed to aspirate clots from large intracranial vessels. With a suction catheter at the proximal end of the clot, the device continuously debulks and aspirates clot debris until the vessel is clear. The device can remove a clot in a matter of minutes,<br>whereas fibrinolytics, even those delivered intra-arterially, may take as long as 2 hours to dissolve a thrombus. | |||
The Solitaire Flow Restoration device and the Trevo Retriever device have the unique ability to both immediately bypass the clot and restore flow and retrieve the clot. | |||
Studies have shown that when clot retrieval is performed within eight hours of symptom onset, 60-68% of patients achieved post-procedure revascularization. Patients eligible for clot retrieval are those with recent ischemic stroke, who can receive treatment within at least 12 (preferably 3-6) hours of the onset of stroke. Those patients with uncontrolled HTN, internal bleeding, seizures, blood clotting problems, or those on anticoagulants are not candidates for this procedure.<br> | |||
Complications from clot retrieval procedures include hemorrhage, internal bleeding, death and recurrence of stroke. | |||
== Haemorrhagic Stroke == | == Haemorrhagic Stroke == | ||
Revision as of 23:43, 6 May 2017
Original Editor - Naomi O'Reilly
Top Contributors - Naomi O'Reilly, Kim Jackson, Lucinda hampton, Admin, Simisola Ajeyalemi, 127.0.0.1, Karen Wilson, Claire Knott, Rucha Gadgil and Wanda van Niekerk
Introduction[edit | edit source]
The team approach to stroke management starts with Emergency Medical Services and continues at a hospital within a Stroke System of Care capable of delivering Acute Stroke Care in the Emergency Department and in a dedicated Stroke Unit.The goal for the acute medical management of patients with stroke is to stabilize the patient and to complete initial evaluation and assessment, including imaging and laboratory studies, within a short time frame. Critical decisions focus on the need for intubation, blood pressure control, and determination of risk / benefit for thrombolytic intervention.[1] Patients presenting with Glasgow Coma Scale scores of 8 or less or rapidly decreasing Glasgow Coma Scale scores, require emergent airway control via intubation.
Goals of Emergency Management
- Support Vital Functions
- Restore Cerebral Circulation
- Reduce Neurological Deficits
- Prevent Progression and Cell Death
- Restore Patient to Optimal Level of Pre-Stroke Function
| American Stroke Association Stroke Chain of Survival | |
| Detection |
Patient/Bystander or EMS recognition of Stroke Signs & Symptoms |
| Dispatch |
EMS Activation; Priority Dispatch & Response |
| Delivery |
Prompt Triage - In the interest of saving time, some EMS actions can be accomplished enroute. Limit assessments / Care on scene to those that are urgently needed or clearly indicated by the patients presentation. Transport to most appropriate Stroke Hospital Prehospital Notification |
| Door |
Immediate Emergency Department triage to high-acuity area |
| Data |
Prompt Emergency Department Evaluation. Stroke Team Activation Lab Studies and Brain Imaging Time barriers at the hospital which should be minimised:
|
| Decision |
Diagnosis and determination of most appropriate therapy; Discussion with Patient and Family |
| Drug |
Administration of appropriate Drugs / Treatment / Interventions Tissue Plasminogen Activator (tPa) for the treatment of acute ischemic stroke must be given within 4.5 hours from the onset of symptoms. Ideally, tPA should be administered (“door to drug”) in less than 60 minutes after Emergency Department arrival. Evidence confirms that the sooner tPA is administered, the more optimal the results. |
| Disposition |
Timely Admission to Stroke Unit, ICU, or Transfer Outcomes are best when patients are admitted directly to and receive care in a dedicated stroke unit, where recovery and rehab can begin immediately. Hospitals without full stroke care capabilities should have official transfer agreements with hospitals offering a full complement of stroke care, and patients should be transferred as soon as reasonably possible. |
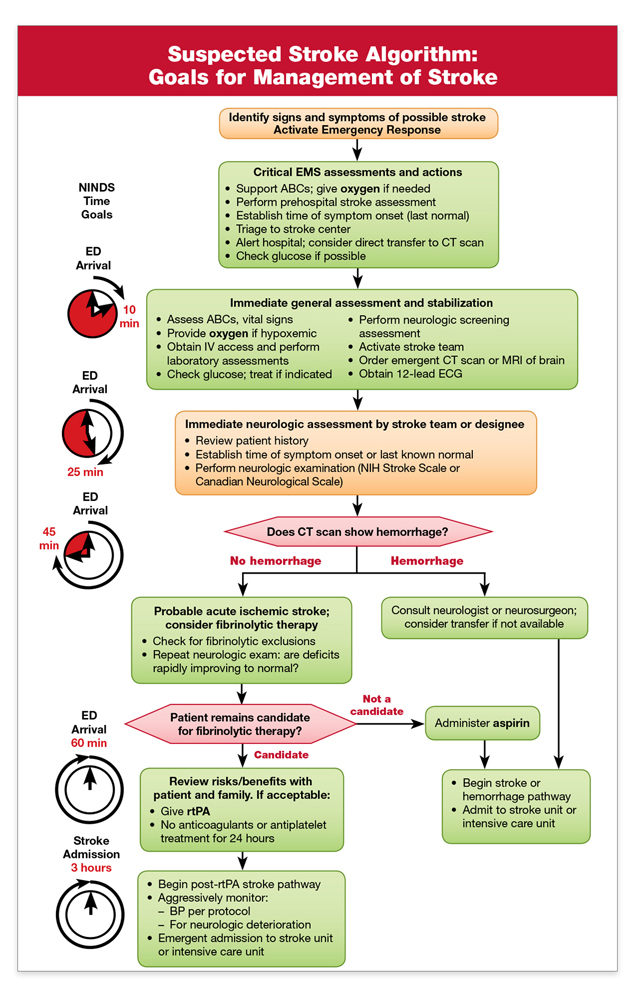
Suspected Stroke Algorithm[edit | edit source]
Ischemic Stroke[edit | edit source]
In the case of an Ischemic Stroke, the more rapidly blood flow is restrored, the ore likely for improved recovery and fewer brain cell deaths. Primary treatment is aimed at breaking down the clot through means of medication (Thrombolysis) or mechanical removal of clot (Thrombectomy). Other treatments aim to minimisethe clot becoming larger or prevention of new clot formation by means of anticoagulant type medications such as Aspirin, Clopidogrel or Dipyridamole. In conjunction with this, overall patient medical condition should be managed including montoring of blood sugars, oxygen levels and hydration and providing adequate treatment for same[2].
Thrombolysis[edit | edit source]
The goal of therapy for ischemic stroke is to safely maximize patient functional recovery to pre-stroke baseline by rapidly reperfusing the ischemic penumbra. tPA has optimal use within 3 hours from onset of symptoms but in carefully selected patients there is a longer time window for treatment of 4.5 hours. Studies continue to support that time from onset to treatment with tPA is directly related to outcomes in ischemic stroke. The sooner tPA is given, the greater the benefit (Stroke, 2013). Beyond the approved and recommended time windows for tPA use, risk of complications rises.
tPA is no different from other medications in that it has potential adverse effects, which makes it essential that a careful consideration is given to exclusion criteria, risks and benefits for use in each individual patient. The major complications is symptomatic intracranial hemorrhage which occurs at a rate of roughly 5.2%. Other complications include orolingual angioedema (allergic reaction), acute hypotension, and systemic bleeding. (Circulation 2010: Part 11: Adult Stroke).
Thrombectomy[edit | edit source]
Clot retrieval devices: There are currently four FDA- approved devices for clot disruption or removal.
The Mechanical Embolus Removal in Cerebral Ischemia (MERCI) Thrombectomy System is a looped wire with progressively smaller helical loops, advanced via a small catheter through the clot. As the catheter is withdrawn, the coiled wire is deployed, which captures the clot for removal.
The Penumbra Thrombectomy System is designed to aspirate clots from large intracranial vessels. With a suction catheter at the proximal end of the clot, the device continuously debulks and aspirates clot debris until the vessel is clear. The device can remove a clot in a matter of minutes,
whereas fibrinolytics, even those delivered intra-arterially, may take as long as 2 hours to dissolve a thrombus.
The Solitaire Flow Restoration device and the Trevo Retriever device have the unique ability to both immediately bypass the clot and restore flow and retrieve the clot.
Studies have shown that when clot retrieval is performed within eight hours of symptom onset, 60-68% of patients achieved post-procedure revascularization. Patients eligible for clot retrieval are those with recent ischemic stroke, who can receive treatment within at least 12 (preferably 3-6) hours of the onset of stroke. Those patients with uncontrolled HTN, internal bleeding, seizures, blood clotting problems, or those on anticoagulants are not candidates for this procedure.
Complications from clot retrieval procedures include hemorrhage, internal bleeding, death and recurrence of stroke.
Haemorrhagic Stroke[edit | edit source]
In the case of Haemorrhagic Stroke the main aim is to stop the bleeding as early as possible, often requiring Neurosurgical Intervention.
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Adams H, Adams R, Del Zoppo G, Goldstein LB. Guidelines for the early management of patients with ischemic stroke: 2005 guidelines update a scientific statement from the Stroke Council of the American Heart Association/American Stroke Association. Stroke. Apr 2005;36(4):916-23.
- ↑ Verheyen G and Ashbury A. IN Physical Management for Neurological Conditions 3rd Edition. Southampton: Elsevier 2011 pp.12-13