Stroke: Assessment
Original Editor - Your name will be added here if you created the original content for this page.
Top Contributors - Naomi O'Reilly, Kim Jackson, Olajumoke Ogunleye, Lucinda hampton, Simisola Ajeyalemi, WikiSysop, Adam Vallely Farrell and Rucha Gadgil
Introduction[edit | edit source]
’Time is Brain’. Acute Stroke is a medical emergency. Stroke is a major cause of death and disability, and patient outcomes depend on how quickly the blood flow can be restored to the damaged area of the brain. Stroke scales are standardized assessment tools used to identify Stroke and clear a path to reperfusion. Treatment options for stroke include thrombolytic medications that aim to dissolve the clot, and interventional endovascular procedures (similar to a cardiac catheterization) to remove it. Successful stroke care requires early recognition, transporting the patient to a designated stroke center, and early activation of a stroke team at the hospital.
Stroke Assessment Scales[edit | edit source]
Pre Hospital[edit | edit source]
Emergency Medical Services (EMS) provide the first medical contact for upto 70% of all stroke patients, and are therefore in a unique position to reduce delays in presentation and treatment. Reliable identification of stroke patients in the field could decrease delays by permitting paramedics to notify receiving hospitals of the imminent arrival of a stroke case ensuring rapid rapid mobilisation of stroke teams and early access to required scanning on hospital arrival. Pre Hospital assessment and determination of stroke severity is a new concept, with the best scale yet to be determined. The Cincinnati and Los Angeles scales have been validated in hospital trials, but studies are mixed when applied by EMS [1]. The RACE Scale has had some positive results when tested among paramedics in Spain with more studies underway [2], currently it is being adopted by many EMS Systems in the United States.
| Scale | Pros | Cons |
|---|---|---|
|
Cincinnati Pre-Hospital Stroke Scale (CPSS) |
Easy to Conduct - 3 Items < 1 Min Derived from NIHSS Sensitivity 66% Specificity 87% |
Unable to measure Posterior Circulation Strokes Does not assess Stroke Severity |
|
Face Arms Speech Test (FAST) |
Easy to Use Can be used by Medical and Non-Medical
|
Does not assess Stroke Severity |
|
Los Angeles Prehospital Stroke Screen (LAPSS) |
Takes < 3 mins to perform More Sensitive / Specific than CPSS Sensitivity 91% Specificity 97% |
Nine Items to Assess Does not assess Stroke Severity |
|
Los Angeles Motor Scale (LAMS) |
Derived from NIHSS Assess Stroke Severity Can Identify Large Vessel Occlusion Sensitivity 81% Specificity 89% |
Takes more time to complete |
|
Rapid Arterial oCclusion Evaluation (RACE) |
Assess Stroke Severity Can Identify Large Vessel Occlusion Sensitivity 85% Specificity 69% |
Takes more time to complete |
|
Miami Emergency Neurological Deficit (MEND) |
Combines Cincinnati Scale with components of NIHSS Takes < 3 mins to perform |
No Published Studies |
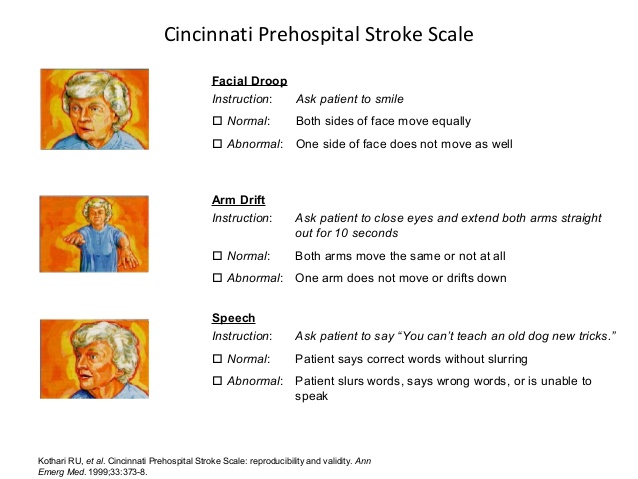
Cincinnati Pre-Hospital Stroke Scale (CPSS)[edit | edit source]
Developed in 1997 at the University of Cincinnati Medical Center for pre-hospital use the Cincinnati Pre-Hospital Stroke Scale (CPSS) was derived from the National Institutes of Health Stroke Scale [3][4]. The CPSS is used to diagnose a potential stroke in a pre-hospital setting through testing the following three signs [3]. If any one of these tests show abnormal findings, the patient may be having a stroke and should be transported to a hospital as soon as possible. Patients with 1 of these 3 findings as a new event have a 72% probability of an ischemic stroke, while if all 3 findings are present the probability of an acute stroke is greater than 85% [5].
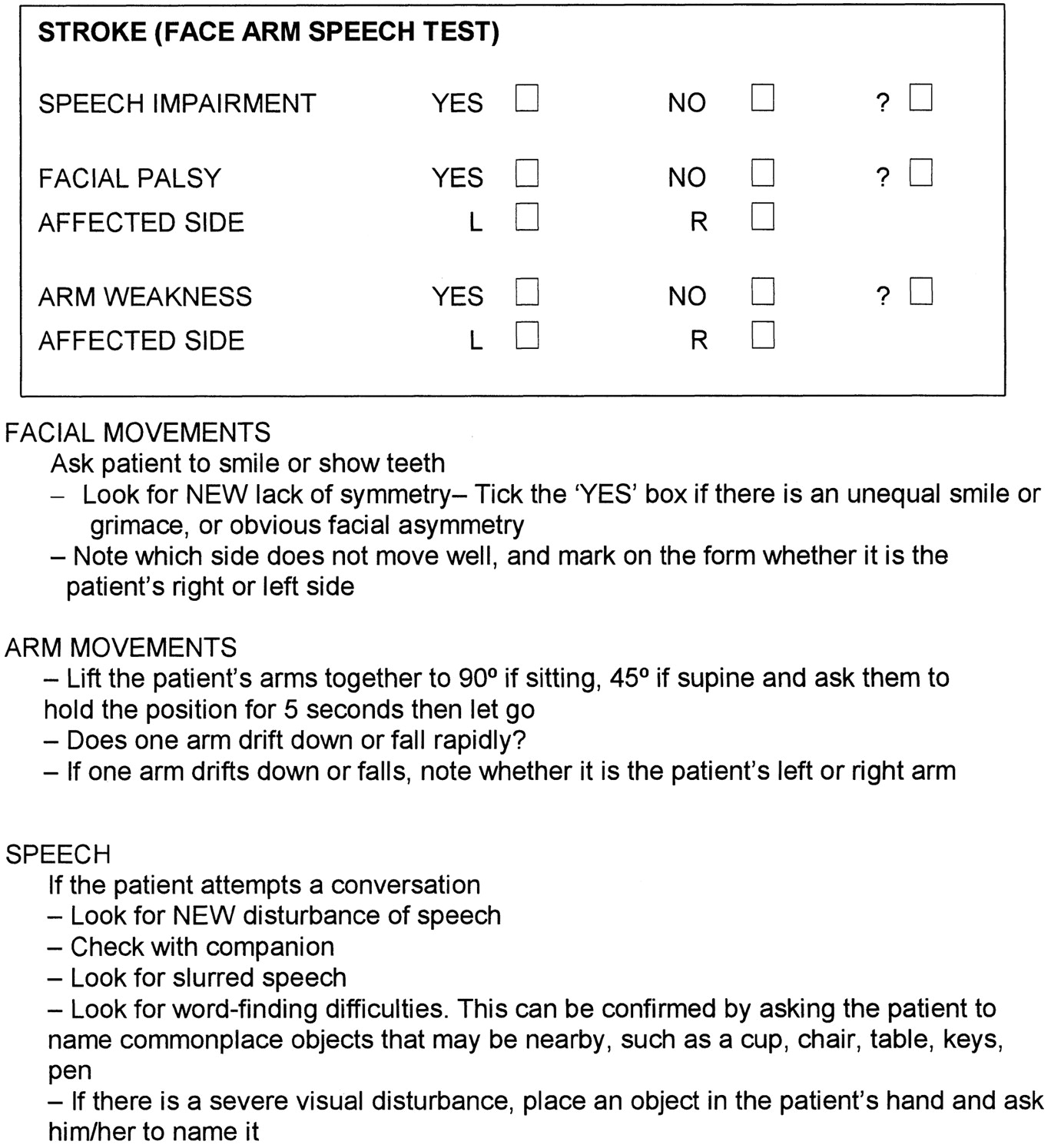
FAST (Face, Arm, Speech Test)[edit | edit source]
FAST was developed in the UK in 1998 by a group of stroke physicians, ambulance personnel, and an emergency room physician and was designed to be an integral part of a training package for ambulance staff. The FAST was derived following a review of existing stroke identification instruments including the Cincinnati Prehospital Stroke Scale (CPSS) and the Los Angeles Prehospital Stroke Screen (LAPSS). FAST was created to expedite administration of intravenous tissue plasminogen activator to patients within 3 hours of acute stroke symptom onset. During the development of FAST Scale, emphasis was placed on producing a simple test that would complement existing assessments used by UK paramedics, such as the Glasgow Coma Scale. FAST contains 3 key elements from the CPSS ((Facial Weakness, Arm Weakness, and Speech Disturbance) but avoids the need to repeat a sentence as a measure of speech, instead using assessment of language ability by the paramedic during normal conversation with the patient. The 3 assessments contained within the FAST were incorporated into the standard ambulance report form used for recording all ambulance contacts within the UK [6].
The FAST Test is now used in many countries as a Campaign for to help the public achieve a better understanding of the warning signs of stroke, ensuring that individuals get the medical assistance they need quicker.
|
Los Angeles Prehospital Stroke Screen (LAPSS)[edit | edit source]
The Los Angeles Prehospital Stroke Screen (LAPSS) is a longer and widely used validated screening tool for early identification of stroke by Emergency Medical Technicians / Paramedics. The LAPSS showed a Sensitivity of 91%, Specificity of 97% with Positive Predictive Value of 86% and Negative Predictive Value of 97% following a Prospective Study In Field Validation Study with 19 UCLA Paramedic Crews, who following a 60-min Training Session [7][8]. If Items 1 - 6 below are all Yes's or Items 5 - 7 Unknown then LAPSS Screening Criteria is met. Note: the patient may still be experienceing a Stroke even if LAPSS Criteria are not met.
| Criteria | Yes | No | Unknown |
|
1. Age greater than 45 years |
|||
|
2. History of Seizures or Epilepsy |
|||
|
3. Onset of Neurological Symptoms is less than 24 hours |
|||
|
4. Patient was Ambulatory prior to onset of symptoms |
|||
|
5. Blood Glucose between 60 and 400 mg/dl |
|||
|
6. Motor Exam: Examine for Motor Asymmetry Based on Exam below, patient has only Unilateral 'Weakness: |
|||
| Equal | Right | Left | |
| Facial Smile / Grimace | Droop | Droop | |
| Grip Strength |
Weak Grip No Grip |
Weak Grip No Grip | |
| Arm Srength |
Drifts Down Falls Rapidly |
Drifts Down Falls Rapidly |
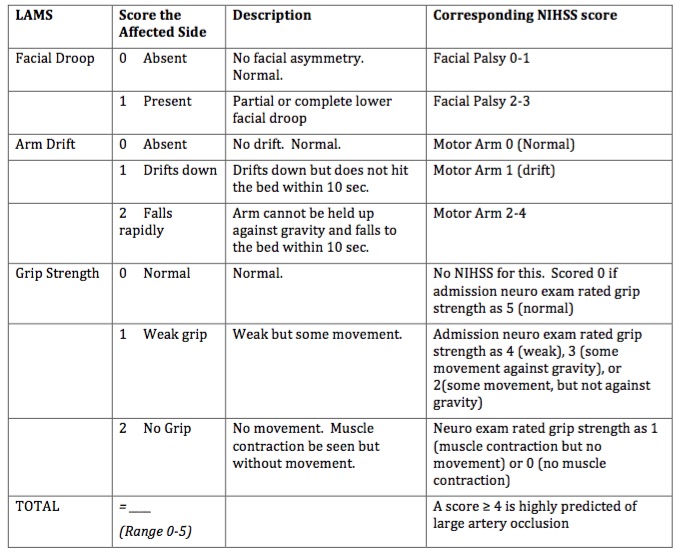
Los Angeles Motor Scale (LAMS)[edit | edit source]
The Los Angeles Motor Scale (LAMS) is a brief 3-item stroke severity assessment measure designed for prehospital and Emergency Department use, derived from the Los Angeles Prehospital Stroke Screen which quantitatively characterizes stroke severity in the field, and predicts functional outcomes with accuracy nearly comparable to that of the full NIHSS. The Los Angeles Motor Scale (LAMS) was constructed by assigning point values to LAPSS items of Facial Weakness (0,1), Arm Strength (0,1,2) and Grip (0,1,2) to yield a total 0–5 Scale [9]. A motor score derived from the LAMS rapidly quantifies stroke severity in the field and predicts functional outcomes with accuracy comparable to that of the full NIHSS and the sNIHSS [10]. A score ≥ 4 is highly predicted of large artery occlusion [11]. Compared with other instruments proposed for prehospital stroke severity assessment the LAMS has advantages of greater simplicity, more rapid administration, and of being immediately derivable from a validated stroke recognition instrument, rather than requiring separate examinations for stroke diagnosis and stroke severity assessment [12].
Performing the LAMS is a good strategy to identify stroke patients in the field, assess their severity, and determine the likelihood that they are candidates for endovascular therapies. Where those with a LAMS score of ≥4, prearrival notification could accelerate endovascular interventions by permitting early mobilization of the endovascular team and readying of the angiographic suite[12].
|
Rapid Arterial oCclusion Evaluation (RACE)[edit | edit source]
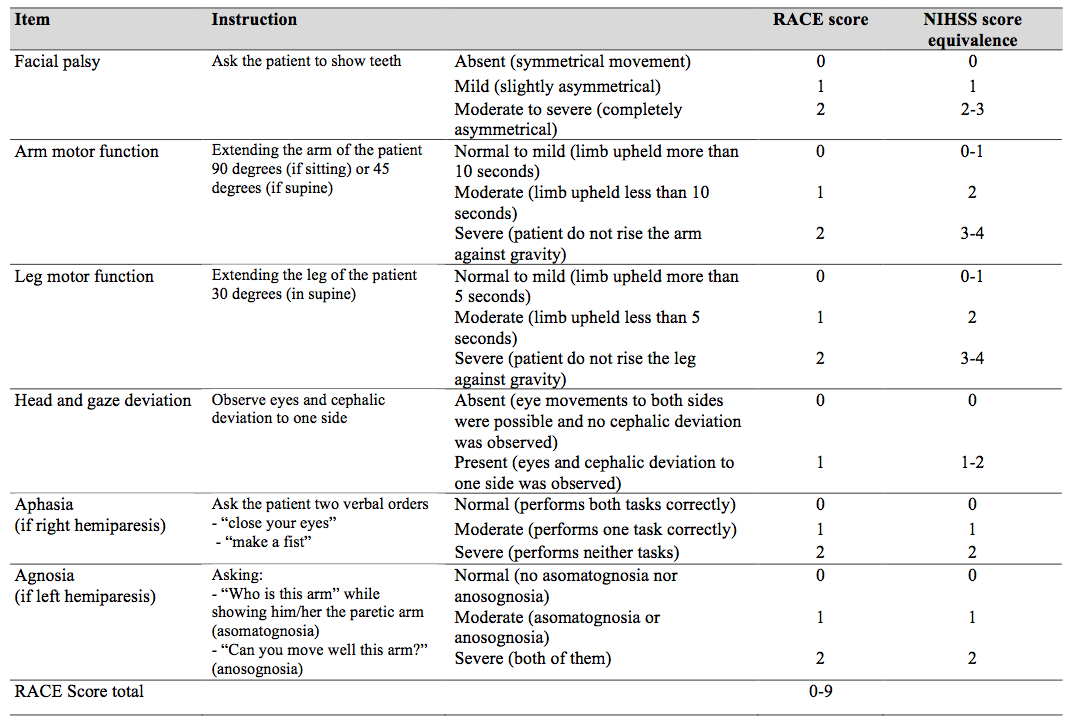
The Rapid Arterial oCclusion Evaluation (RACE) Scale is the most recent scale developed and was designed based on the National Institutes of Health Stroke Scale (NIHSS) to accurately assess stroke severity and identify patients with acute stroke with large artery occlusion at prehospital setting by medical emergency technicians who may be candidates to be treated with endovascular techniques in a comprehensive stroke center[13]. The RACE Scale takes slightly more time to perform than the CPSS and the LAPSS with the goal of the scale to more accurately identify Stroke Severity and localise the area affected [14].
The RACE scale is a simplification of the NIHSS scale using those items with a higher ability to predict the presence of a large vessel occlusion. It evaluates 5 items: Facial Palsy, Brachial Paresis, Crural Paresis, Oculocephalic Deviation and Aphasia/Agnosia, with a total score of 0-9. Based on the RACE Scale a Stroke is likely with a score above 1 and an Emergent Large Vessel Occlusion is likely if the cumulative score is > 4 with a sensitivity of 85% and specificity of 69%.
|
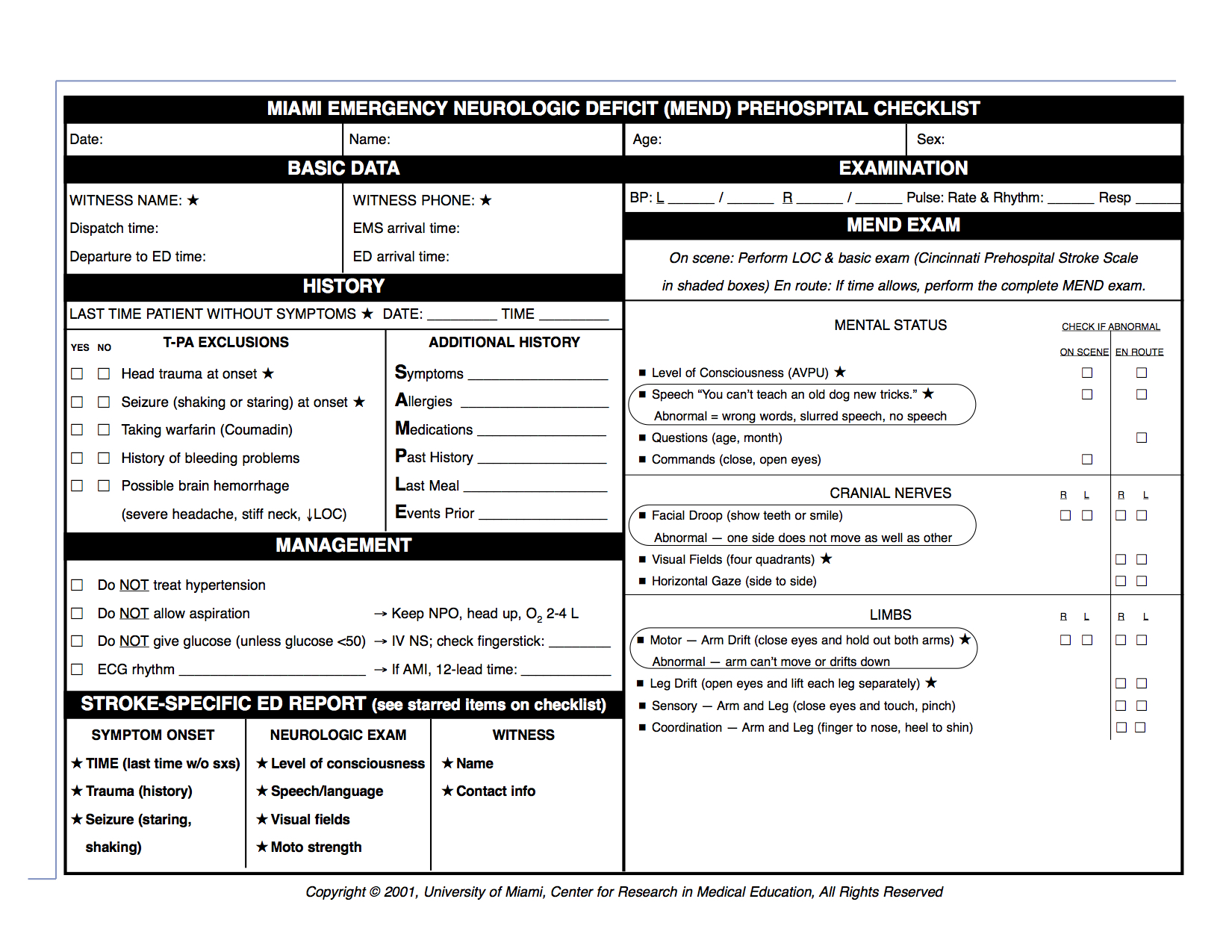
Miami Emergency Neurological Deficit (MEND)[edit | edit source]
The Miami Emergency Neurologic Deficit (MEND) is an easy-to-learn, easy-to-use checklist that provides key information which incorporates the three components of the Cincinnati Prehospital Stroke Scale (CPSS) as well as additional components from the NIH Stroke Scale (NIHSS). The MEND was devised to facilitate communication between healthcare providers throughout the continuum of care for stroke patients as it can be used to obtain a baseline exam in the prehospital setting and then for initial evaluation and subsequent exams in the emergency department or ICU. It is more thorough than the CPSS but takes less than 3 minutes to perform and requires no additional tools. in the prehospital setting is that the CPSS be performed on scene and the MEND exam be performed en route, to minimize transport delays.
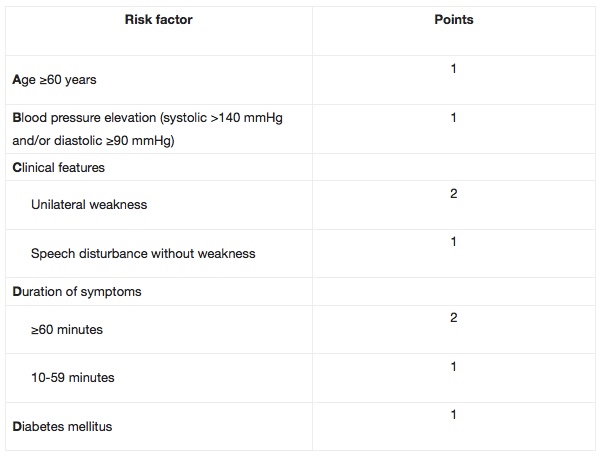
ABCD / ABCD2[edit | edit source]
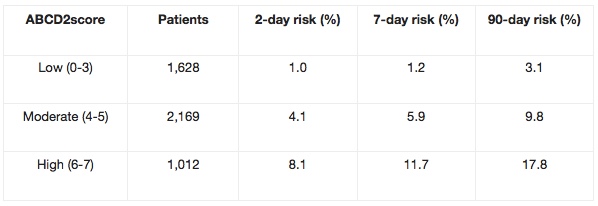
The ABCD / ABCD2 can be used to predict the risk of stroke during the first seven days after having a Transient Ischemic Attack (TIA). Researchers found there to be over 30% risk of stroke in TIA patients with an 'ABCD score' of six, as compared to no strokes in those with a low ABCD score. Can be used in routine clinical practice to identify high-risk individuals who require emergency investigation and treatment.
The ABCD2 score was created by merging two previously validated clinical decision rules - the ABCD and the California scores. The ABCD score was created to estimate the 7-day risk of stroke following a TIA, while the California score predicted the 90-day risk.The ABCD2 score is a validated, seven-point, risk-stratification tool to identify patients at high risk of stroke following a TIA. Patients with scores ≥4 are at considerably higher risk of stroke in the 2-day period following a TIA, and may potentially require urgent intervention as inpatients.
Acute[edit | edit source]
Main role to measure deficits and stroke severity, which predicts patient discharge disposition. It provides a Standardized Neurological Exam, that can be utilised to monitor Neurological Status and can also be used to match patients to allow for comparison in clinical trials.
National Institutes of Health Stroke Scale (NIHSS)[edit | edit source]
The National Institutes of Health Stroke Scale (NIHSS) is a systematic assessment tool that provides a quantitative measure of stroke-related neurologic deficit. The NIHSS was originally designed as a research tool to measure baseline data on patients in acute stroke clinical trials. Now, the scale is also widely used as a clinical assessment tool to evaluate acuity of stroke patients, determine appropriate treatment, and predict patient outcome.
The NIHSS can be used as a clinical stroke assessment tool to evaluate and document neurological status in acute stroke patients[15]. The stroke scale is valid for predicting lesion size and can serve as a measure of stroke severity. The NIHSS has been shown to be a predictor of both short and long term outcome of stroke patients[16]. Additionally, the stroke scale serves as a data collection tool for planning patient care and provides a common language for information exchanges among healthcare providers.
The scale is designed to be a simple, valid, and reliable tool that can be administered at the bedside consistently by physicians, nurses or therapists.
[edit | edit source]
Canadian Neurological Scale - 1986[edit | edit source]
One of the first scales developed to assess stroke patients- 1986.
• Validity: Has not been validated prospectively- only retrospective
studies.
• Strengths : Standardized neurological assessment. Could be used as a monitoring tool.
• Weaknesses: Long, scoring is too complex
European Stroke Scale - 1994[edit | edit source]
Sub Heading 3[edit | edit source]
Recent Related Research (from Pubmed)[edit | edit source]
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Asimos AW, Ward S, Brice JH, Rosamond WD, Godstein LB, Studnek J. Out-of-hospital stroke screen accuracy in a state with an emergency medical services protocol for routing patients to acute stroke centers. Annals of Emergency Medicine, 2014; 64 (5) 509-515.
- ↑ Perez de la Ossa N, Carrera D, Gorchs M, Querol M, Millan M, Gomis M, et al. Design and validation of a prehospital stroke scale to predict large arterial occlusion: The rapid arterial occlusion evaluation scale. Stroke, 2014; 45:87–91
- ↑ 3.0 3.1 Hurwitz AS, Brice JH, Overby BA, Evenson KR. Directed use of the Cincinnati Prehospital Stroke Scale by laypersons. Prehospital Emergency Care. 2005 Jan 1;9(3):292-6.
- ↑ Kothari, R.; Hall, K.; Brott, T.; Broderick, J. (1997-10-01). "Early stroke recognition: developing an out-of-hospital NIH Stroke Scale". Academic Emergency Medicine. 4 (10): 986–990. ISSN 1069-6563. PMID 9332632.
- ↑ American Heart Association (2011). Advanced Cardiovascular Life Support Provider Manual. USA: First American Heart Association Printing. p. 137. ISBN 978-1-61669-010-6.
- ↑ Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke. 2003 Jan 1;34(1):71-6.
- ↑ Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field: prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS) Stroke. 2000; 31 (1): 71–76. doi: 10.1161/01. STR.;31:71.
- ↑ Chen S, Sun H, Lei Y, Gao D, Wang Y, Wang Y, Zhou Y, Wang A, Wang W, Zhao X. Validation of the Los Angeles pre-hospital stroke screen (LAPSS) in a Chinese urban emergency medical service population. PLoS One. 2013 Aug 7;8(8):e70742.
- ↑ Llanes JN, Starkman S, Kidwell CS, Eckstein M, Saver JL. The LAPSS Motor Scale (LAMS): a new measure for characterizing stroke severity in the field.
- ↑ Llanes JN, Kidwell CS, Starkman S, Leary MC, Eckstein M, Saver JL. The Los Angeles Motor Scale (LAMS): a new measure to characterize stroke severity in the field. Prehospital Emergency Care. 2004 Jan 1;8(1):46-50.
- ↑ Llanes
- ↑ 12.0 12.1 Nazliel B, Starkman S, Liebeskind DS, Ovbiagele B, Kim D, Sanossian N, Ali L, Buck B, Villablanca P, Vinuela F, Duckwiler G. A brief prehospital stroke severity scale identifies ischemic stroke patients harboring persisting large arterial occlusions. Stroke. 2008 Aug 1;39(8):2264-7.
- ↑ de la Ossa NP, Carrera D, Gorchs M, Querol M, Millán M, Gomis M, Dorado L, López-Cancio E, Hernández-Pérez M, Chicharro V, Escalada X. Design and Validation of a Prehospital Stroke Scale to Predict Large Arterial Occlusion. Stroke. 2014 Jan 1;45(1):87-91.
- ↑ de la Ossa NP, Ribó M, Jiménez X, Abilleira S. Prehospital Scales to Identify Patients With Large Vessel Occlusion. Stroke. 2016 Nov 1;47(11):2877-8.
- ↑ Spilker J1, Kongable G, Barch C, Braimah J, Brattina P, Daley S, Donnarumma R, Rapp K, Sailor S. Using the NIH Stroke Scale to assess stroke patients. The NINDS rt-PA Stroke Study Group. J Neurosci Nurs. 1997 Dec;29(6):384-92.
- ↑ H.P. Adams Jr., P.H. Davis, E.C. Leira, K.-C. Chang, B.H. Bendixen, W.R. Clarke, R.F. Woolson, Hansen, MS. Baseline NIH Stroke Scale score strongly predicts outcome after stroke: A report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology July 1, 1999 vol. 53 no. 1 126