Spondylodiscitis
Original Editors - Lynn Leemans
Top Contributors - Ine Wittevrongel, Bo Hellinckx, Lucinda hampton, Kim Jackson, Admin, WikiSysop, 127.0.0.1 and Claire Knott
Introduction[edit | edit source]
Spondylodiscitis, also referred to as discitis-osteomyelitis, is characterised by infection involving the intervertebral disc (IVD) and adjacent vertebrae.[1] The condition is difficult to treat due to the the limited blood supply to these segments, a factor that makes it also rare. Treatment consists of an extended antibiotic course, with good outcomes but misdiagnosis or a delay in treatment may result in significant morbidity/mortality.[2]
Terminology: Discitis is discouraged as a term as isolated infection of the spinal disc rarely occurs. Normally the initial infection is the vertebral endplate with secondary involvement of the disc. The terms spondylodiscitis or vertebral osteomyelitis are preferred as they are more accurate.
Pathology[edit | edit source]
In adults, infection is begins at the vertebral body endplate, extending into the IVD space and then into the adjacent vertebral body endplate.
Paediatrics present differently with infection often starting in the intervertebral disc itself as direct blood supply still present).[1]
Etiology[edit | edit source]
Most cases of Spondylodiscitis arise from one of three initial events: direct inoculation, hematogenous spread, or less commonly contiguous spread. Finding the causative agent is very difficult, the most commonly identified organism is being Staphylococcus aureus.[2]
Epidemiology[edit | edit source]
Spondylodiscitis has a bimodal age distribution
- More common in pediatric patients than in the adult population, as consequence of the greater vascular supply of the IVD.
- Older population ~50 years, more often men
Risk Factors[edit | edit source]
Include
- remote infection (present in ~25%)
- ascending infection, e.g. from urogenital tract instrumentation
- spinal instrumentation or trauma
- intravenous drug use (IVDU)
- immunosuppression
- long-term systemic administration of steroids
- advanced age
- diabetes mellitus
- organ transplantation
- malnutrition
- cancer[1]
Characteristics/Clinical Presentation[edit | edit source]
The symptoms are non-specific, diffuse [3] and treacherous [4]. However the usual presentation is back pain (over 90% of patients) and possibly fever (under 20% of patients). Patients are often bacteraemic , originating from eg endocarditis, intravenous drug use.[1]
Differential Diagnosis[edit | edit source]
Differential diagnoses include:
- Erosive osteochondrosis [4]
- Osteoporotic and pathological fracture
- Cancer related destruction
- Ankylosing spondylarthritis
- Scheuermann's kyphosis [5][3]
- Charcot joint
- Modic type I degenerative change
- Schmorl nodes
- Langerhans cell histiocytosis (LCH) [5][3]
- Disc herniation
- Metastatic seeding
- Inflammatory or degenerative spinal disease [6]
Diagnostic Procedures[edit | edit source]
It is important to identify and treat spondylodiscitis as early as possible.
The clinical presentation of spondylodiscitis are manifold. This commonly leads to a several months from initial symptoms to final diagnosis. [7]
A number of different tests and tools help in diagnosis include:
- Magnetic Resonance Imaging (MRI) : Golden standard. Detects any spread of the inflammation. [3][4][8][9][10][9]
- PET and PET/CT [6][11][4]: Due to its high specificity, [3] F-FDG PET/CT should be considered as a first-line imaging procedure in the diagnosis of spondylodiscitis. [6]
- Biopsy: Pathogens are only successfully detected in about half of the patients. To obtain a definite diagnosis: Blood Culture [7][10]
-
Outcome Measures[edit | edit source]
Include:
- Visual Analogue Scale (VAS): [3][6][11][8] to evaluate therapeutic effects, for assessment of pain.
- Oswestry disability index (ODI): [3][6][11] to evaluate therapeutic effects, assessment of quality of life
Examination[edit | edit source]
It is important to identify and treat spondylodiscitis as early as possible. Diagnosis by means of blood culture and MRI and treatment of the infection with antibiotics and possibly surgical interventions seem be very suitable, but need to be individualized to each and every patient.[7] (level of evidence 2B)
Diagnosis is based on clinical, laboratory and radiological features and can be difficult. It is often delayed or missed due to the rarity of the disease, the insidious onset of symptoms and the high frequency of low back pain in the general population.[11][9][8] (level of evidence 2A)
1.Anamnesis:[12][4] (level of evidence 1B)
- Gender, age
- Risk factors (see clinical presentation)
o diabetes mellitus
o advanced aged
o steroid use - Comorbidity
- Clinical symptomatology (see clinical presentation)
o Constant pain, more worse at night [5]
o Radicular pain radiating to the chest or abdomen
o Fever
o Screening red flags [4]
o Thoracic pain
o Widespread neurological deficit, vertebral level involved
o Lower limb weakness
o Drug abuse/human immunodeficiency virus
o Age <20 or >55 years
o Weight loss
o Persistent severe restriction of lumbar flexion
o Constant progressive, mechanical pain
o Positive cough/sneeze
o Previous history of cancer
o Recent history of a trauma
2. Clinical examination [3] (level of evidence 2A)
Inspection concentrating on local changes and taking a detailed neurological status
- Spinal tenderness [5]
- Loss of lumbar lordosis and lower back movement [5]
- Inspection on local changes and neurological status (parese, paralyse,..)
- Pain on heelstrike, impactation and percussion
- Relieving posture (avoid stressing the ventral sections of the spinal column
- Inclination and re-erection are painful
- Reduction of mobility
- Paravertebral muscle spasm [5]
3. Basic objective tools [3]
Medical Management[edit | edit source]
There are several treatments for spondylodiscitis, par example: surgical and conservative treatment. Surgical and conservative treatment for postoperative lumbar spondylodiscitis is effective. Surgical treatment is superior to conservative treatment in a short time, while conservative treatment can achieve long-term satisfactory curative effects. [LoE: 2B] [3]
Randomized trials are needed to assess the optimal treatment duration, route of administration, and the role of combination therapy and newer agents.
[LoE: 2A] [5]
1. Conservative treatment:
This treatment is based on antibiotics and immobilization of the spine.[6] It can be considered when the clinical symptoms and destruction are relatively mild or the risk of operation is too great. The main problem in conservative treatment is to achieve adequate fixation of the affected section of the spinal column. Reclining orthosis distribute the stress over the unaffected spinal column joints, thus decreasing stress in the infected ventral area. The mobilization of the patient is only recommended once osseous infiltration becomes visible. Aside from the risk of immobilization, there is a high rate of pseudoarthroses (16% to 50%), which may eventually lead to kyphotic malposition and chronic pain syndrome. If there is no fusion reaction, continuing destruction, when the symptoms persist or worsen [4], or there’s no clinical improvement, it is not promising to continue conservative treatment beyond four to six weeks.[3] Although protracted bed rest used to be prescribed, this practice is now being abandoned. There’s also a correlation between early diagnosis and successful results obtained with suitable conservative treatment.[3]
A review of case series has demonstrated the effectiveness of intravenous antibiotic therapy. While no official guidance exists for when to switch from intravenous to oral antibiotics, our study shows that CRP at 1 month is >30mg/l and we recommend 6 weeks of intravenous therapy, followed by 6 further weeks of oral therapy.[LoE: 2B] [11]
Treatment of spondylodiscitis at children should be conservative with antibiotics only. [10]
2. Surgery
Surgery has an important role in alleviating pain, correcting deformities and neural compromise and restoring function.[LoE: 2B][7]
- Indications for surgical intervention:
o compression of neural elements
o spinal instability due extensive bony destruction
o severe kyphosis
o failure of conservative management
o (sometimes) inatractable pain
o (sometimes) epidural abscess even in the absence of neurogical deficits - Indications for surgical emergency
o spinal cord compression
o outcomes are worse if paralysis has been present over 24-36h (there are also investigators who improve improvement with prolonged paralysis) [LoE: 2B] [10] - Methodes
o While radical surgical debridement, stable reconstruction together with antibiotic therapy remained a reliable approach to achieve complete healing of the inflammation, anterior alone surgery became more applicable. [2B][9][12]
A debridement and fixation with anterior column support in combination with an antibiotic therapy appear to be the key points for successful treatment of pyogenic spondylodiscitis. [2B][4]
Physical Therapy Management[edit | edit source]
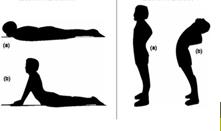
Spondylodiscitis has several clinical symptoms, a severe one is low back pain. This can be treated with exercises. (LOE 3B) [3] Prognosis seems to be good with conservative treatment including NSAID’S, physiotherapy (exercises), and a corset. Wearing the corset for a period of 6–10 weeks is instead confirmed by most authors. (LOE 5) [4][10][5]Several exercises can be done with the emphasis on extension exercises and exercises for trunk balance. This is important to maintain a good posture. (LOE 5, 3B, 3A, 1A) [7][5][3][4][10][5][10][5]
Thoracal extension exercises
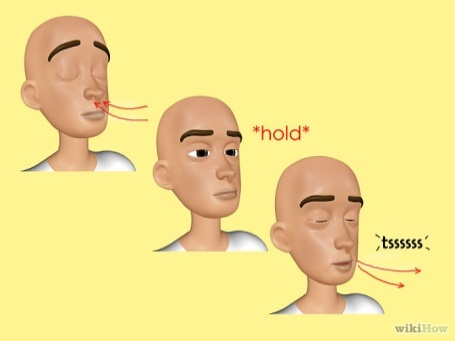
Early mobilization is important. (LOE 3A) [4] But also limb exercises are considered to be good for the therapy.(LOE 3B) [4] These exercises should be done daily at home. Also general fitness, like swimming, should be encouraged. This therapy can lead to a decrease in pain and the ability to accomplish activities of daily living. (LOE 5, 3B) [10][5]In a severe disease TNF therapy can be done. (LOE 5) [5] Lung re-expansion exercises (breathing exercises) are taken into the physical therapy. These exercises help the stability in the lower back. (LOE 3B, 3A) [4][12]
Respiratory exercises
Low back pain is strongly related with tight and strained hamstrings. Patients should do flexibility exercises for the hamstrings, maintain a good position while sitting and move enough to help this. Keeping the hamstrings flexible is important for pain control as well as in prevention of spinal pain flare-ups. (LOE 5) [7]
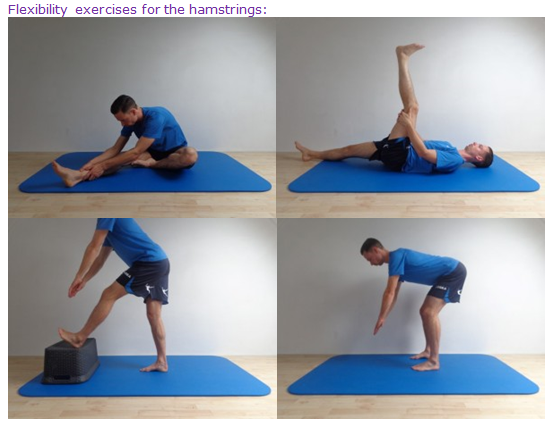
Flexibility exercises
In general the rehabilitation program will improve the patient’s sensory and motor skills, develop the balance and proprioception and will help the patient’s to do their daily living activities. During the total program the onset and increase of pain should be evaluated. Pain intensity increases or exercises that provoke too much pain or exhaust the patient should not be in the rehabilitation program and there has to be enough rest after the exercises. It is important that when there is a resting period, this one has to be kept minimal. Immobilization lead to weakness of the trunk and lower extremity muscles and will contribute to complications. Secondary problems because of immobilization and musculoskeletal problems should be looked after and prevented. The patient also gets a home exercise program that is based on the patient’s capacity. (LOE 5) [5]
Back school is less effective compared to the active programme. (LOE 1A) [6] Exercises were significantly better than no intervention and reduced back pain experience and work absenteeism. Exercises may be effective in prevention of back pain (LOE 1A) [6]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
- Pubmed (VUB BIBLIO)
- Web of Knowledge
- Pedro
- Google Scholar
Clinical Bottom Line[edit | edit source]
Spondylodiscitis can be defined as a primary infection of the intervertebral disc (discitis), with secondary infections of the vertebrae (spondylitis). It can lead to osteomyelitis of the spinal column. Pyogenic spondylodiscitis is frequently caused by the staphylococcus. Tuberculous spondylodiscitis is caused by the mycobacterium tuberculosis. The symptoms are non-specific, diffuse and treacherous. Diagnosis is difficult and often delayed or missed due to the rarity of the disease. The basic diagnostic examination to establish spondylodiscitis is MRI. Surgical and conservative treatment for postoperative lumbar spondylodiscitis is effective. Prognosis seems to be good with conservative treatment including NSAID’S, physiotherapy (exercises), and a corset.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Radiopedia Spondylodiscitis Available:https://radiopaedia.org/articles/spondylodiscitis (accessed 26.11.2022)
- ↑ 2.0 2.1 Muscara JD, Blazar E. Diskitis. InStatPearls [Internet] 2022 May 13. StatPearls Publishing. Available: https://www.ncbi.nlm.nih.gov/books/NBK541047/ (accessed 26.11.2022)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 F. Postacchini, 1999, Lumbar disc herniation, Springer, 481p. (Level of evidence 5)
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 Erhard R, Relative Effectiveness of an Extension Program and a Combined Program of Manipulation and Flexion and Extension Exercises in Patients With Acute Low Back Syndrome, Journal of The American Physical Therapy Association 1994. (level of evidence 1A)
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 R. Sobottke et al., Current Diagnosis and Treatment of Spondylodiscitis. Deutsches ärzteblatt International, 2008. (Level of evidence 2A)
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 M. Titlic et al., Spondylodiscitis, Journal Citation/ Science Edition, 2008; 109(8) 345-347. (Level of evidence 2A)
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 A. Hegde, et al., Infections of the deep neck spaces, Singapore Med J. 2012 May;53(5):305-312 (level of evidence 5)
- ↑ 8.0 8.1 8.2 Enrique G. et al., Surgical treatment of spondylodiscitis. An update, International Orthopaedics 2012. (level of evidence 5)
- ↑ 9.0 9.1 9.2 9.3 Kapsalaki E. et al., Spontaneous spondylodiscitis: presentation, risk factors, diagnosis, management, and outcomes, International Journal of Infectious Diseases 2009. (level of evidence 1B)
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 P. Prithvi, et al., Intervertebral Disc: Anatomy-Physiology-Pathophysiology-Treatment, Department of Anesthesiology and Pain Management, World Institute of Pain, 2008 (level of evidence 2A)
- ↑ 11.0 11.1 11.2 11.3 11.4 M. Hasenbring et al., Intervertebral disk diseases, Thieme, 2008, 236p. (Level of evidence 5)
- ↑ 12.0 12.1 12.2 Sans N. et al., Infections of the spinal column — Spondylodiscitis, Diagnostic and Interventional Imaging 2012. (level of evidence 5)