Spinal Muscular Atrophy (SMA): Difference between revisions
Jeremy Bryan (talk | contribs) No edit summary |
Jeremy Bryan (talk | contribs) No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Evelin Milev|Evelin Milev]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | <div class="editorbox"> '''Original Editor '''- [[User:Evelin Milev|Evelin Milev]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
Revision as of 18:00, 22 May 2023
Introduction[edit | edit source]
Spinal Muscular Atrophy (SMA) is a genetic disorder also considered to be a neurodegenerative disorder, specifically a motor neurone disease. SMA is characterised by degeneration of alpha motor neurons in the spinal cord, affecting the control of voluntary muscle movement.[1] It occurs in roughly one in 6,000-10,000 births.[2] There are several classification of SMA, which are assigned based on the age that symptoms first occur along with the the highest level of muscle activation attained or expected to be attained. [1][3]
Pathological Process[edit | edit source]
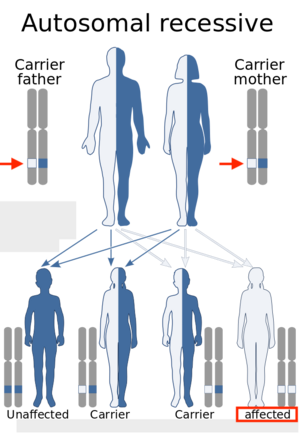
SMA is considered to be an autosomal recessive condition resulting from the homozygous deletion of the gene SMN1 (survival of motor neuron 1).[2] In some cases, it is possible for the neighbouring SMN2 gene to compensate for a lack of the SMN1 gene. Therefore, if there is one or more additional copies of the SMN2 gene, later onset and less severe SMA symptoms can occur.[3]
Clinical Presentation and Classification[edit | edit source]
SMA is classified based on the age that symptoms first occur along with the the highest level of muscle activation attained or expected to be attained. [1][3]SMA symptoms range in severity but often include hypotonia, muscle weakness (proximal muscles greater than distal muscles and lower extremity greater than upper extremity), tremors, bone or joint issues, difficulty swallowing, and or difficulty breathing.[3][5]
Types of SMA[edit | edit source]
- Type 0 - Presence of profound muscle weakness with symptom onset in babies less than six months old. Strong possibility of prenatal symptom onset (third trimester reports of decreased fetal movement).[3]
- Type I (Werdnig-Hoffmann disease of acute infantile SMA) - Symptoms presents in babies less than six months old. Sitting unsupported may never be achieved. Presents with delayed motor development, hypotonia, generalized symmetrical muscle weakness, a lack of deep tendon reflexes, poor head control, weak cough, and difficulty swallowing. Cognitive function, diaphragm function, sphincter control, and sensation are spared. Weak accessory breathing muscles and decreased pulmonary function can contribute to a high incidence of death before age two, due to pulmonary infection.[3]
- Type II (intermediate or chronic infantile SMA) - Symptoms presents in babies between six and eighteen months old. May achieve the ability to sit unsupported, but cannot stand. Joint contractures and kyphoscoliosis are very common along with fine tremors of the upper extremities. Respirator involvement may require ventilator support due to inadequate ventilation/profusion. Leading cause of morbidity and mortality is respiratory failure. However, there is a seventy-five percent survival rate at age twenty-five.[3]
- Type III (Kugelberg-Welander syndrome or juvenile SMA) - Symptoms presents after eighteen months of age. Walking independently is usually achieved. Muscle weakness, worse in the lower extremities, is the main symptom. Patients can expect a normal lifespan.[3]
- Type IV - Generally symptoms present after after ten years of age. Symptoms include mild muscle weakness. Patients can expect normal walking ability and a normal lifespan.[3]
Diagnostic Procedures[edit | edit source]
Diagnosis generally starts with genetic testing to determine whether or not the SMN1 gene is absent. Genetic testing has been found to have a 95% sensitivity (test shows absence of SMN1 gene when it is truly absent) and an almost 100% specificity (test shows presence of SMN1 gene when it is truly present). If genetic testing does return a result consistent with clinical signs and symptoms, additional testing in the form of electrocardiography, a muscle biopsy, a nerve conduction velocity study, or blood tests can be performed.[3][7]
Outcome Measures[edit | edit source]
There are several outcome measures which can be used to detect changes in the course of treatment for patients with SMA. These tools should be appropriately selected according to the age and severity of the disease.
- Six-Minute Walking Test (6MWT) - The Six-Minute-Walking-Test can be safely performed in ambulant patients with SMA. It has been proven to detect fatigue-related changes in this population of patients and also correlates with other established outcome measures for patients with spinal muscular atrophy[8].
- Revised Hammersmith Scale for SMA (RHS) - The RHS is predominantly used in patients with SMA type 2 and 3. In a combination with the WHO motor milestones, the scale can be more sensitive toward the description of the SMA phenotype. The RHS has been designed to capture a wide range of abilities across a broad spectrum of SMA, from very young children to adolescents and adults[2].
- WHO Developmental Milestones - The WHO scales aim to link the growth of the child and motor development in one single reference. The final version of the protocol includes six items: "Sitting without support", "Hands-and-knees crawling", "Standing with assistance", "Walking with assistance", "Standing alone", and "Walking alone". The WHO provides important information about a child's gross motor development in different cultural settings[9].
- Revised Upper Limb Module (RULM) for SMA - The RULM is a specifically designed outcome measure for upper limb function in patients with Spinal Muscular Atrophy. The scale has shown good reliability and validity, which makes it a good choice for assessing arm function in children and adults with SMA[10].
Management / Interventions[edit | edit source]
The management of SMA warrants a multi-disciplinary approach coordinated by the patient's primary clinician.[11]
Orthopedic Management[11]
- Spinal deformities
- Scoliosis
- Bracing
- Limit scoliosis progression during growth years, not corrective
- Surgical intervention (hardware implantation)
- Goal is to ultimately promote better breathing mechanics and sitting alignment
- Bracing
- Scoliosis
- Contractures
- Management through Physical Therapy
- Surgical intervention if significant impairment or pain is present
- Fractures
- Cast immobilization if non-ambulatory
- Surgical fixation if ambulatory
Nutrition Management[11]
- Maintenance of adequate nutritional intake
- Adequate calcium and vitamin D
- Maintenance of appropriate body mass index
- Screening and monitoring for complication such as...
- Glucose abnormalities
- Hyperlipidemia
- Abnormal fatty acid metabolism
- Metabolic acidosis
Speech Language Pathology[11]
- Screening and intervention for dysphagia
Medical Management[12]:
- Neuroprotective drugs like riluzole
- Drugs to improve energy metabolism
- Drugs affecting the gene expression of SMN
Gene Therapy:
- Along with advances in medical management, gene therapy approaches have been evaluated for SMA, using viral vectors to replace SMN1 gene.[13]
Physiotherapy[edit | edit source]
- Merconi et al.[11] provides a comprehensive outline of physiotherapy management for SMA broken down by functional level.
| Functional Level | Goals | Possible Deficits | Possible Interventions/Adaptations |
|---|---|---|---|
| Patients not able to sit unsupported |
|
|
|
| Patients able to sit unsupported |
|
|
|
| Patients able to ambulate |
|
|
|
Respiratory Care[edit | edit source]
Many children and adults with Spinal Muscular Atrophy will be dependent on pulmonary management due to loss of muscle function. A respiratory therapist should be included in the multidisciplinary treatment team from an early stage to ensure proper respiratory management.[14]
Chest physiotherapy - Assists with respiratory management and should be one of the primary airway clearance therapies.[14]
Mechanical insufflation–exsufflation - devices such as Cough Assist or VitalCough can be used and this should be one of the primary airway clearance therapies.[14]
Suctioning is a critical part of the treatment and should be used in all patients with excessive secretions or in those with ineffective cough.
The high-frequency chest wall oscillation (Vest) is another option for managing secretions. However, there is no evidence that the Vest improves airway clearance and secretions.[14]
Non-invasive positive pressure ventilation (NIV) should be used for respiratory failure or to prevent chest wall distortion.[14]
Continuous positive airway pressure (CPAP) should be used only when NIV is not tolerated or in the treatment of chronic respiratory failure.[14]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Darras BT, Markowitz JA, Monani UR, De Vivo DC. Spinal muscular atrophies (2015) Neuromuscular Disorders of Infancy. Childhood, and Adolescence: A Clinician’s Approach.:117-45.
- ↑ 2.0 2.1 2.2 Ramsey D, Scoto M, Mayhew A, Main M, Mazzone ES, Montes J, de Sanctis R, Dunaway Young S, Salazar R, Glanzman AM, Pasternak A. Revised Hammersmith Scale for spinal muscular atrophy: A SMA specific clinical outcome assessment tool. PloS one. 2017 Feb 21;12(2):e0172346.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Umphrend D, Lazaro R, Roller M, Burton G. Umphrend's Neurological Rehabilitation. Sixth Edition. St. Louis, MO, USA. Elsevier Mosby, 2013.
- ↑ Genentech. Understanding Spinal Muscular Atrophy (SMA). Available from: https://www.youtube.com/watch?v=5mI_ZsWkkc4 (last accessed 7.6.2019)
- ↑ National Health Service. Spinal muscular atrophy. Available from https://www.nhs.uk/conditions/spinal-muscular-atrophy-sma/ Last accessed 4/24/2023.
- ↑ Cure SMA. Learn to Spot the Warning Signs of SMA – Snapshot of Hallmark Symptoms (Video 9) Available from: https://www.youtube.com/watch?v=G5yIdH0yans&feature=emb_logo [last accessed 31/01/2021]
- ↑ National Institute of Neurological Disorders and Stroke. Spinal Muscle Atrophy. Available from https://www.ninds.nih.gov/health-information/disorders/spinal-muscular-atrophy (accessed 4/26/2023).
- ↑ Montes J, McDermott MP, Martens WB, Dunaway S, Glanzman AM, Riley S, Quigley J, Montgomery MJ, Sproule D, Tawil R, Chung WK. Six-Minute Walk Test demonstrates motor fatigue in spinal muscular atrophy. Neurology. 2010 Mar 9;74(10):833-8.
- ↑ Wijnhoven TM, de Onis M, Onyango AW, Wang T, Bjoerneboe GE, Bhandari N, Lartey A, Rashidi BA. Assessment of gross motor development in the WHO Multicentre Growth Reference Study. Food and nutrition bulletin. 2004;25(1_suppl_1):S37-45.
- ↑ Mazzone ES, Mayhew A, Montes J, Ramsey D, Fanelli L, Young SD, Salazar R, De Sanctis R, Pasternak A, Glanzman A, Coratti G. Revised upper limb module for spinal muscular atrophy: development of a new module. Muscle & nerve. 2017 Jun;55(6):869-74.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Mercuri E, Finkel RS, Muntoni F, Wirth B, Montes J, Main M, Mazzone ES, Vitale M, Snyder B, Quijano-Roy S, Bertini E. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscular Disorders. 2018 Feb 1;28(2):103-15.
- ↑ Tiziano FD, Lomastro R, Pinto AM, Messina S, D'Amico A, Fiori S, Angelozzi C, Pane M, Mercuri E, Bertini E, Neri G. Salbutamol increases survival motor neuron (SMN) transcript levels in leucocytes of spinal muscular atrophy (SMA) patients: relevance for clinical trial design. Journal of medical genetics. 2010 Dec 1;47(12):856-8.
- ↑ Passini MA, Cheng SH. Prospects for the gene therapy of spinal muscular atrophy. Trends in molecular medicine. 2011 May 1;17(5):259-65.
- ↑ 14.0 14.1 14.2 14.3 14.4 14.5 Finkel RS, Mercuri E, Meyer OH, Simonds AK, Schroth MK, Graham RJ, Kirschner J, Iannaccone ST, Crawford TO, Woods S, Muntoni F. Diagnosis and management of spinal muscular atrophy: Part 2: Pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscular Disorders. 2018 Mar 1;28(3):197-207.