Spinal Muscular Atrophy (SMA): Difference between revisions
Jeremy Bryan (talk | contribs) No edit summary |
Jeremy Bryan (talk | contribs) No edit summary |
||
| Line 17: | Line 17: | ||
=== Types of SMA === | === Types of SMA === | ||
* Type 0 - Presence of profound muscle weakness with symptom onset in babies less than six months old. Strong possibility of prenatal symptom onset (third trimester reports of decreased fetal movement).<ref name=":3" /> | * Type 0 - Presence of profound muscle weakness with symptom onset in babies less than six months old. Strong possibility of prenatal symptom onset (third trimester reports of decreased fetal movement).<ref name=":3" /> | ||
* Type I (Werdnig-Hoffmann disease of acute infantile SMA) - | * Type I (Werdnig-Hoffmann disease of acute infantile SMA) - Symptoms presents in babies less than six months old. Sitting unsupported may never be achieved. Presents with delayed motor development, hypotonia, generalized symmetrical muscle weakness, a lack of deep tendon reflexes, poor head control, weak cough, and difficulty swallowing. Cognitive function, diaphragm function, sphincter control, and sensation are spared. High incidence of death before age two due to pulmonary infection.<ref name=":3" /> | ||
* Type II (intermediate or chronic infantile SMA) - | * Type II (intermediate or chronic infantile SMA) - Symptoms presents in babies between six and eighteen months old. May achieve the ability to sit unsupported, but cannot stand. Joint contractures and kyphoscoliosis are very common along with fine tremors of the upper extremities. May require ventilator support due to inadequate ventilation/profusion. Leading cause of morbidity and mortality is respiratory failure. However, there is a seventy-five percent survival rate at age twenty-five.<ref name=":3" /> | ||
* Type III (Kugelberg-Welander | * Type III (Kugelberg-Welander syndrome or juvenile SMA) - Symptoms presents after eighteen months of age. Walking independently is usually achieved. Muscle weakness, worse in lower extremities, is the main symptom. Patients can expect a normal lifespan.<ref name=":3" /> | ||
* Type IV - Generally symptoms presents after after ten years of age. Symptoms include mild muscle weakness. Patients can expect normal walking ability and a normal lifespan.<ref name=":3" /> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Revision as of 17:38, 26 April 2023
Introduction[edit | edit source]
Spinal Muscular Atrophy (SMA) is a genetic disorder also considered to be a neurodegenerative disorder, specifically a motor neurone disease. SMA is characterised by degeneration of alpha motor neurons in the spinal cord, affecting the control of voluntary muscle movement.[1] It occurs in roughly one in 6,000-10,000 births.[2] There are several classification of SMA, which are assigned based on the age that symptoms first occur along with the the highest level of muscle activation attained or expected to be attained. [1][3]
Pathological Process[edit | edit source]
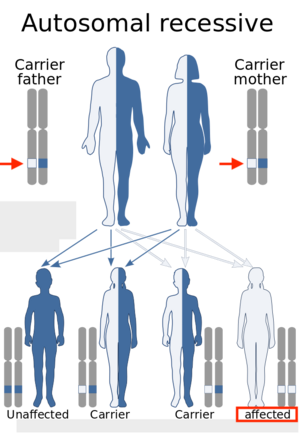
SMA is considered to be an autosomal recessive condition resulting from the homozygous deletion of the gene SMN1 (survival of motor neuron 1).[2] In some cases, it is possible for the neighbouring SMN2 gene to compensate for a lack of the SMN1 gene. Therefore, if there is one or more additional copies of the SMN2 gene, later onset and less severe SMA symptoms can occur.[3]
Clinical Presentation and Classification[edit | edit source]
SMA is classified based on the age that symptoms first occur along with the the highest level of muscle activation attained or expected to be attained. [1][3]SMA symptoms range in severity but often include hypotonia, muscle weakness, tremors, bone or joint issues, difficulty swallowing, and or difficulty breathing.[5]
Types of SMA[edit | edit source]
- Type 0 - Presence of profound muscle weakness with symptom onset in babies less than six months old. Strong possibility of prenatal symptom onset (third trimester reports of decreased fetal movement).[3]
- Type I (Werdnig-Hoffmann disease of acute infantile SMA) - Symptoms presents in babies less than six months old. Sitting unsupported may never be achieved. Presents with delayed motor development, hypotonia, generalized symmetrical muscle weakness, a lack of deep tendon reflexes, poor head control, weak cough, and difficulty swallowing. Cognitive function, diaphragm function, sphincter control, and sensation are spared. High incidence of death before age two due to pulmonary infection.[3]
- Type II (intermediate or chronic infantile SMA) - Symptoms presents in babies between six and eighteen months old. May achieve the ability to sit unsupported, but cannot stand. Joint contractures and kyphoscoliosis are very common along with fine tremors of the upper extremities. May require ventilator support due to inadequate ventilation/profusion. Leading cause of morbidity and mortality is respiratory failure. However, there is a seventy-five percent survival rate at age twenty-five.[3]
- Type III (Kugelberg-Welander syndrome or juvenile SMA) - Symptoms presents after eighteen months of age. Walking independently is usually achieved. Muscle weakness, worse in lower extremities, is the main symptom. Patients can expect a normal lifespan.[3]
- Type IV - Generally symptoms presents after after ten years of age. Symptoms include mild muscle weakness. Patients can expect normal walking ability and a normal lifespan.[3]
Diagnostic Procedures[edit | edit source]
Diagnoses could be made by prenatal screening or by gene panel investigation and/or muscle biopsy. In the early stages, the diagnosis may be suspected due to symptoms like floppiness and muscular weakness. Children with type I SMA can present with a lack of head control, minimal to absent anti-gravity movements and severe respiratory complications.
The first step in diagnosing someone with SMA would be by taking a full clinical examination and family history. A blood test might be required to look at the amount of creatine kinase (CK), an investigation to indicate if muscle damage has occurred. High levels of CK in the blood is not damaging itself, but it is an important indicator of a muscle disorder condition. Electrophysiological tests such as electromyography (EMG), and nerve conduction study should be performed, if EMG suggests a motor neuron disease, then, further testing should be done.
Further investigation will probably include genetic testing as this is the most accurate way to diagnose if a patient has Spinal Muscular Atrophy.
Differential Diagnosis[edit | edit source]
Neuromuscular conditions:
- Duchenne Muscular Dystrophy
- Charcot-Marie-Tooth
- Amyotrophic Lateral Sclerosis
Congenital Myopathies:
- congenital myotonic dystrophy,
- congenital myasthenic syndromes,
- metabolic myopathies
Congenital disorders of the motor neuron and the peripheral nerve (congenital hypomyelinating neuropathy).
Non-Neuromuscular Conditions:
- Prader-Willi syndrome,
- acute hypoxic ischemic encephalopathy,
- neonatal sepsis and
- dyskinetic or metabolic conditions
The tools that can address these differential diagnostic possibilities beyond the clinical examination and careful family history are CK determination, EMG/nerve conduction studies, MRI of the brain, muscle biopsy, and specific genetic or metabolic testing.
Outcome Measures[edit | edit source]
There are several outcome measures which can be used to detect changes in the natural history of patients with SMA. These tools should be appropriately selected according to the age and severity of the disease.
- Six-Minute Walking Test (6MWT) - The Six-Minute-Walking-Test can be safely performed in ambulant patients with SMA. It has been proven to detect fatigue-related changes in this population of patients and also correlates with other established outcome measures for patients with spinal muscular atrophy[7].
- Revised Hammersmith Scale for SMA (RHS) - The RHS is predominantly used in patients with SMA type 2 and 3. In a combination with the WHO motor milestones, the scale can be more sensitive toward the description of the SMA phenotype. The RHS has been designed to capture a wide range of abilities across a broad spectrum of SMA, from very young children to adolescents and adults[2].
- WHO Developmental Milestones - The WHO scales aim to link the growth of the child and motor development in one single reference. The final version of the protocol includes six items: "Sitting without support", "Hands-and-knees crawling", "Standing with assistance", "Walking with assistance", "Standing alone", and "Walking alone". The WHO provides important information about a child's gross motor development in different cultural settings[8].
- Revised Upper Limb Module (RULM) for SMA - The RULM is a specifically designed outcome measure for upper limb function in patients with Spinal Muscular Atrophy. The scale has shown good reliability and validity, which makes it a good choice for assessing arm function in children and adults with SMA[9].
Management / Interventions[edit | edit source]
Spinal Muscular Atrophy (SMA) is a severe genetic condition which requires precise diagnosis and extensive physiotherapy treatment in order to protect the muscles from rapid deterioration and development of contractures. The management of SMA must be as a part of a broad multi-disciplinary team which should include rehabilitation, spinal management, orthopaedics, nutritional and gastrointestinal management.
Recently, it has been stated that SMA might be a multi-organ disease and a more detailed examination should be performed. Further recommendations have been made on pulmonary management and acute care issues in the severe forms of spinal muscular atrophy[10].
Medical Management[11]:
- Neuroprotective Drugs like riluzole,
- Drugs to improve energy metabolism and
- Drugs affecting the gene expression of SMN
Gene Therapy:
Along with advances in medical management, gene therapy approaches have been evaluated for SMA, using viral vectors to replace SMN1 gene[12].
Stem Cell Therapy: cellular replacement strategy in the treatment of SMA[13]. However, this therapy is still in the testing stages.
Cell replacement may be achieved by :
- Transplantation of stem cell-derived cells which have undergone maturation in vitro
- Activation of endogenous stem cells in the CNS
Physiotherapy[edit | edit source]
- Assessment of the patient with neuromuscular disease and particularly with SMA is of great importance. Looking at baseline function, joint range and power will assist the physiotherapist to follow on the progression of the condition.
- Orthotics
- Splinting
- Taping
- Management of contractures
- Exercise and activity
Respiratory Care[edit | edit source]
Many children and adults with Spinal Muscular Atrophy will be dependent on pulmonary management due to loss of muscle function. When a patient with SMA has a respiratory failure they need to be transferred on non-invasive positive pressure ventilation (NIV). In order for this to be implemented in the best possible way, a respiratory physiotherapist should be involved in the assessment and the management of pulmonary complications[14].
Airway clearance (chest physio) is best administered with the combination of Cough Assist and this should be the primary airway clearance therapy for all SMA patients with respiratory illness.
Suctioning is a critical part of the treatment and should be used in all patients with excessive secretions or in those with ineffective cough.
The high-frequency chest wall oscillation (Vest) is another option for managing secretions. However, there is no evidence that the Vest improves airway clearance and secretions.
Non-invasive positive pressure ventilation (NIV) should be used for respiratory failure or to prevent chest wall distortion.
Continuous positive airway pressure (CPAP) should be used only when NIV is not tolerated or in the treatment of chronic respiratory failure[14].
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Darras BT, Markowitz JA, Monani UR, De Vivo DC. Spinal muscular atrophies (2015) Neuromuscular Disorders of Infancy. Childhood, and Adolescence: A Clinician’s Approach.:117-45.
- ↑ 2.0 2.1 2.2 Ramsey D, Scoto M, Mayhew A, Main M, Mazzone ES, Montes J, de Sanctis R, Dunaway Young S, Salazar R, Glanzman AM, Pasternak A. Revised Hammersmith Scale for spinal muscular atrophy: A SMA specific clinical outcome assessment tool. PloS one. 2017 Feb 21;12(2):e0172346.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Umphrend D, Lazaro R, Roller M, Burton G. Umphrend's Neurological Rehabilitation. Sixth Edition. St. Louis, MO, USA. Elsevier Mosby, 2013.
- ↑ Genentech. Understanding Spinal Muscular Atrophy (SMA). Available from: https://www.youtube.com/watch?v=5mI_ZsWkkc4 (last accessed 7.6.2019)
- ↑ National Health Service. Spinal muscular atrophy. Available from https://www.nhs.uk/conditions/spinal-muscular-atrophy-sma/ Last accessed 4/24/2023.
- ↑ Cure SMA. Learn to Spot the Warning Signs of SMA – Snapshot of Hallmark Symptoms (Video 9) Available from: https://www.youtube.com/watch?v=G5yIdH0yans&feature=emb_logo [last accessed 31/01/2021]
- ↑ Montes J, McDermott MP, Martens WB, Dunaway S, Glanzman AM, Riley S, Quigley J, Montgomery MJ, Sproule D, Tawil R, Chung WK. Six-Minute Walk Test demonstrates motor fatigue in spinal muscular atrophy. Neurology. 2010 Mar 9;74(10):833-8.
- ↑ Wijnhoven TM, de Onis M, Onyango AW, Wang T, Bjoerneboe GE, Bhandari N, Lartey A, Rashidi BA. Assessment of gross motor development in the WHO Multicentre Growth Reference Study. Food and nutrition bulletin. 2004;25(1_suppl_1):S37-45.
- ↑ Mazzone ES, Mayhew A, Montes J, Ramsey D, Fanelli L, Young SD, Salazar R, De Sanctis R, Pasternak A, Glanzman A, Coratti G. Revised upper limb module for spinal muscular atrophy: development of a new module. Muscle & nerve. 2017 Jun;55(6):869-74.
- ↑ Mercuri E, Finkel RS, Muntoni F, Wirth B, Montes J, Main M, Mazzone ES, Vitale M, Snyder B, Quijano-Roy S, Bertini E. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscular Disorders. 2018 Feb 1;28(2):103-15.
- ↑ Tiziano FD, Lomastro R, Pinto AM, Messina S, D'Amico A, Fiori S, Angelozzi C, Pane M, Mercuri E, Bertini E, Neri G. Salbutamol increases survival motor neuron (SMN) transcript levels in leucocytes of spinal muscular atrophy (SMA) patients: relevance for clinical trial design. Journal of medical genetics. 2010 Dec 1;47(12):856-8.
- ↑ Passini MA, Cheng SH. Prospects for the gene therapy of spinal muscular atrophy. Trends in molecular medicine. 2011 May 1;17(5):259-65.
- ↑ Harper JM, Krishnan C, Darman JS, Deshpande DM, Peck S, Shats I, Backovic S, Rothstein JD, Kerr DA. Axonal growth of embryonic stem cell-derived motoneurons in vitro and in motoneuron-injured adult rats. Proceedings of the National Academy of Sciences. 2004 May 4;101(18):7123-8.
- ↑ 14.0 14.1 Finkel RS, Mercuri E, Meyer OH, Simonds AK, Schroth MK, Graham RJ, Kirschner J, Iannaccone ST, Crawford TO, Woods S, Muntoni F. Diagnosis and management of spinal muscular atrophy: Part 2: Pulmonary and acute care; medications, supplements and immunizations; other organ systems; and ethics. Neuromuscular Disorders. 2018 Mar 1;28(3):197-207.