Sinus Tarsi Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 109: | Line 109: | ||
Articles:<br>• Taillard W, Meyer JM, Garcia J, Blanc Y. The Sinus Tarsi Syndrome. International Orthopaedics (SICOT) 1981; 5:117-130 (level: A1)<br>• Helgeson K. Examination and Intervention for Sinus Tarsi Syndrome. North American Journal of Sports Physical Therapy 2009 February; 4(1):29-37 (level: A1)<br>• Rosenberg ZS, Beltran J, Bencardino JT. From the RSNA Refrecher Courses. MR Imaging of the Ankle and Foot. RadioGraphics 2000; 20:153-179 (level: A1) | Articles:<br>• Taillard W, Meyer JM, Garcia J, Blanc Y. The Sinus Tarsi Syndrome. International Orthopaedics (SICOT) 1981; 5:117-130 (level: A1)<br>• Helgeson K. Examination and Intervention for Sinus Tarsi Syndrome. North American Journal of Sports Physical Therapy 2009 February; 4(1):29-37 (level: A1)<br>• Rosenberg ZS, Beltran J, Bencardino JT. From the RSNA Refrecher Courses. MR Imaging of the Ankle and Foot. RadioGraphics 2000; 20:153-179 (level: A1) | ||
• K. Helgeson, PT, DHSc ; Examination and Intervention for Sinus Tarsi Syndrome ; orth American Journal of Sports Physical Therapy, 2009;4(1):29-37<br>• Thermann H, Zwipp H, Tshcernes H. Treatment algorithm of chronic ankle and subtalar instability. Foot Ankle. 1997; 18:163-169<br>• Kevin Helgeson, Examination and Intervention for Sinus Tarsi Syndrome, N Am Sports Phys ther, feb 2009, 4(1), 29-37 (level: 5)<br>• FW. Roemer et al, Ligamentous Injuries and the Risk of Associated Tissue Damage in Acute Ankle Sprains in Athletes, N Am Sports med, 2014 april 21, 42(7), 1549-1557 (level: 3A)<br> | |||
Books:<br>• Meir Nyska, Gideon Mann, editors. The unstable ankle. Chapter 14: Sinus Tarsi Syndrome. United States: Human Kinetics Publishers, Inc. 2002. p144-120 | Books:<br>• Meir Nyska, Gideon Mann, editors. The unstable ankle. Chapter 14: Sinus Tarsi Syndrome. United States: Human Kinetics Publishers, Inc. 2002. p144-120 | ||
Sites:<br>• American Academy of Podiatric Sports Medicine. Sinus Tarsi Syndrome. http://www.aapsm.org/sinus_tarsi_syndrome.html (accessed 27/11/2010)<br>• MyFootShop. Sinus Tarsi Syndrome. http://www.myfootshop.com/detail.asp?Condition=Sinus%20Tarsi%20Syndrome (accessed 28/11/2010)<br>• PhysioAdviser.com. Sinus Tarsi Syndrome. http://www.physioadvisor.com.au/8074550/sinus-tarsi-syndrome-physioadvisor.htm (accessed 28/11/2010)<br> | Sites:<br>• American Academy of Podiatric Sports Medicine. Sinus Tarsi Syndrome. http://www.aapsm.org/sinus_tarsi_syndrome.html (accessed 27/11/2010)<br>• MyFootShop. Sinus Tarsi Syndrome. http://www.myfootshop.com/detail.asp?Condition=Sinus%20Tarsi%20Syndrome (accessed 28/11/2010)<br>• PhysioAdviser.com. Sinus Tarsi Syndrome. http://www.physioadvisor.com.au/8074550/sinus-tarsi-syndrome-physioadvisor.htm (accessed 28/11/2010)<br> | ||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Revision as of 22:32, 28 August 2015
Original Editors - Merlin Roggeman
Top Contributors - Merlin Roggeman, Vanbeylen Antoine, Yassin Khomsi, Kim Jackson, Rachael Lowe, Admin, Lucinda hampton, Venus Pagare, Simisola Ajeyalemi, Claire Knott, Rucha Gadgil, Aimee Tow, Wanda van Niekerk, Jess Bell, Pinar Kisacik, Khloud Shreif and Peter Vaes
Search Strategy[edit | edit source]
To search for information you can use databases such as PubMed, Web of Science, PEDro or Google Scholar. Use keywords as ‘sinus tarsi syndrome’ or ‘sinus tarsitis’. For specific information you can use ‘AND’ and add ‘physical therapy’, ‘characteristics’, ‘definition’, depending on what you search. Also choose articles from which the full text is available for free, but then the sources have to be controlled. For anatomical information, the use of different anatomical atlas is recommended.
Definition/Description[edit | edit source]
The sinus tarsi syndrome is a foot pathology, mostly following after a traumatic injury to the ankle. It may also occur if the person has a pes planus or an (over)-pronated foot, which can cause compression in the sinus tarsi. Some characteristics are pain at the lateral side of the ankle and a feeling of instability. [1][2]
Recent discussions of sinus tarsi syndrome (STS) describe this entity as primarily an instability of the subtalar joint due to ligamentous injuries that results in a synovitis and infiltration of fibrotic tissue into the sinus tarsi space.[8]
Clinically Relevant Anatomy[edit | edit source]
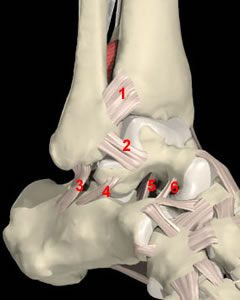
The sinus tarsi is a tunnel between the talus and the calcaneus, which contains some anatomic structures that can be injured in STSand filled with connective tissues, those contribute to the stability of the ankel and to its proprioception. The joint between the talus and calcaneus is also known as the subtalar joint. This articulation incudes 3 facets: an anterior, middle and posterior facet. Variation in structure of those facets affects the stability of the subtalar joint. This joint is also composed of numbers of ligaments as: the extrensic ligaments (calcaneofibular and deltoid ligament), the interosseus, the talo-calcaneal ligament (number 5 in figure 1), the cervical ligament (number 6 in figure 1), and the medial, lateral and intermediate roots of the inferior extensor retinaculum.[1][2][3][4]
Which all provide extra stability to the articulation.
What concerns nerve structures. Laterally of the sinus tarsi we can observe the sinus tarsi
and some branches of it may run through the tarsi.[4]
Figure 1: an image of the ankle, with the sinus tarsi between the talus and calcaneus, and the ligaments in the sinus (numbers 5 and 6) (source: http://www.blackburnfeet.org.uk/hyperbook/trauma/ankleFx/ankleFxBasic1.htm)
Extrinsic and intrinsic ligaments provide static stability for the subtalar joint. Extrinsic ligaments include the calcaneofibular ligament and the deltoid ligament, which also provide stability for the talocrural joint.
The intrinsic ligaments are the talocalcaneal, interosseuous, and cervical ligaments. They provide a strong connection for the calcaneal and talar joint surfaces. Ruptures of the intrinsic ligaments allow increased movement of the subtalar joint that may result in instability.[8]
Akiyama K did a study where the suggest that the sinus tarsi is not only a talocalcaneal joint space but a source of nociceptive and proprioceptive information on the movement of the foot and ankle. Sinus tarsi syndrome may result from disorders of nociception and proprioception in the foot. [12]
Epidemiology /Etiology[edit | edit source]
Mostly the sinus tarsi syndrome occurs after a traumatic lateral ankle sprainor multiple ankle sprains (mostly due to a weak anterior talofibular ligament)[11] which consequences result in injuries to the interosseus and cervical ligaments.
The ligaments of the sinus tarsi can be sprained or torn, and an inflammation and hemorrhage of the synovial recess in the sinus tarsi can occur. This happens in 70% of the cases.[1][2][4]
This pathology is mostly a result of synovitis and infiltration of fibrotic tissue into the sinus tarsi space due to an instability of the subtalar joint, caused by ligamentous injuries.[10]
The sinus tarsi syndrome can also occur as a compression injury, for example to people who have flat or pronated feet. The talus and calcaneus are pressed together as a result of the deformation. This causes bone to bone contact of the talus and calcaneus, with inflammation or arthritis in the sinus.[1][4]
Characteristics/Clinical Presentation[edit | edit source]
The characteristics of the syndrome are pain at the lateral side of the ankle. “The pain is most severe when standing, walking on uneven ground or during the movements of supination and adduction of the foot'.”[1] People suffering from the sinus tarsi syndrome also have a feeling of instability (functional instability) in the hind foot.[1][4]
When the syndrome is a result of an inverted ankle sprain there is a major chance the lateral collateral ligaments of the ankle are also damaged, since the ligaments in the sinus tarsi are the last ones to tear with a traumatic ankle sprain.[1][4]
Moreover the loss of stability in our ankle will allow a greater range of motion to our subtalar joint. This execessive movement will increase the forces onto the synovium and across the sinus tarsi. It is this subtalar joint synovitis whom is responsible for chronic inflamation and infiltration of fibrotic tissues in the sinus tarsi and results in ankle pain.
Furthermore those injuries can also dammage ligaments of the tibiotallar and talocalcaneal joints and increase the mobility between the talocrural and subtalar joints.[10]
Differential Diagnosis[edit | edit source]
These common pathologies may give the same pain characteristics or symptoms:[5]
-ankle sprain
-calcaneal fracture
-talar fracture
-peroneal tendonitis
-subtalar joint arthritis
-tarsal tunnel syndrome
Localization of pain to the sinus tarsi with the presence of ankle instability is a good indication that the patient has developed STS. The diagnosis of STS has typically been confirmed by the cessation of symptoms upon injection of lidocaine into the sinus tarsi. [8]
Diagnostic Procedures[edit | edit source]
Diagnosis of the sinus tarsi syndrome is usually made by excluding other foot pathologies. CT-scans exclude bone fractures, but are not specific enough to diagnose STS. The most commonly used methods are MRI’s. MRI findings may include filling of the sinus tarsi space with fluid or scar tissue, alterations in the structure of the ligaments or degenerative changes in the subtalar joint.[2][3][6]
Magnetic resonance imaging (MRI) is the best method to visualize the structure within the sinus tarsi, especially the interosseous and cervical ligaments. The MRI findings may also include alterations in the structure of the interosseous and cervical ligaments and degenerative changes in the subtalar joint. [8]
Cadaveric study results indicate that initial and reconstructed MR arthrograms along and perpendicular to the ligament axes are potentially useful for further evaluation of individual tarsal sinus structures. 18
Outcome Measures[edit | edit source]
add links to outcome measures here (also see Outcome Measures Database)
Examination[edit | edit source]
When having a patient with pain in the lateral ankle, the physiotherapist should check eventual functional instability and compensation with the other ankle.[2]
An acute ankle injury will typically present with pain accompanied by swelling, ecchymosis, and tenderness in the anterolateral ankle. Because the synovitis and fibrotic tissues associated with STS will take time to develop, athletes with injuries to the subtalar joint may not initially have symptoms that can be localized to the sinus tarsi. [8]
Stability of the subtalar joint is assessed with medial and lateral subtalar joint glides performed by moving the calcaneus over a stabilized talus in the transverse plane and with subtalar joint distraction. [8]
https://www.youtube.com/watch?v=un7eANQq29g
In standing posture the patients may demonstrate a pes planus posture or an asymmetry of the rearfoot angle with the leg.[2]
In passive examination, the range of motion of the ankle may be limited in pronation and supination, but pain over the sinus tarsi at the end range of plantar flexion combined with supination is a typical sign for STS. The subtalar joint may have increased translation mobility if the interosseus and cervical ligaments are disrupted, but this is not always the case.[2]
The therapist should examine the talocrural and subtalar joints for signs of hypermobility as injuries can affect both of these important articulations of the lower extremity. Localized ankle discomfort to the sinus tarsi space and feelings of instability with pronation and supination movements of the subtalar joint will help identify STS.[8]
The therapist should also evaluate if there is any muscle weakness of the peroneal and planatr flexor muscles. This is done with resistance tests of the ankle: pronation tests and flexion tests.[2][4]
There is a stability test that is thought to recreate instability of the subtalar joint. The test is performed with the athlete in supine with the ankle in 10 degrees of dorsiflexion to keep the talocrural joint in a stable position. The forefoot is first stabilized by the examiners hand, while an inversion and internal rotational force is applied to the calcaneus. Then an inversion force is applied to the forefoot. The examiner assesses for an excessive medial shift of the calcaneus and a reproduction of the athlete’s complaint of instability and symptoms. [8] [9]
(http://www.arthritis.co.za/the%20clinical%20examination%20technique.html)
Medical Management
[edit | edit source]
The treatment of the sinus tarsi syndrome can be conservative or operative.
The first one includes physiotherapy (see physical therapy management), injections with corticosteroids in the sinus tarsi, local gels or drugs.[1][4]
Operative treatment is also very effective in most cases, but needs to be considered as a last resort if conservative treatment fails.[4]
Subtalar arthroscopy is useful for the diagnosis and treatment of STS. Furthermore, subtalar arthroscopy allows for direct visualization of pathologic findings in STS. [13]
STS can be treated by open surgery and subtalar arthroscopy when conservative treatments are ineffective. Kuwada [14] (level : 2B)reported a long-term treatment results of STS where all patients who underwent open excision during a 15-year period were reported to achieve 100% pain relief, and there were no complications. Lowy et al. [15] (level :4) reported that 15 of 21 STS patients who underwent open surgery achieved complete pain relief and that the remaining 6 achieved partial relief. Moreover, Frey et al. [16] (level :4) reported that, among 21 STS patients, 43% had an excellent result and 43% had a good result after subtalar arthroscopy; only 3 patients (14%) had a poor result. Thus, according to these studies, open surgery and arthroscopic treatments produce similarly satisfactory results. Notable is that arthroscopic treatment alone resolves the symptoms of STS as well as open surgery, which involves the excision of all synovial tissue in the lateral contents of the sinus tarsi.
Subtalar arthroscopy has been reported to be associated with complications of neuritis, sinus tract formation, and superficial wound infection, although these responded to nonsurgical treatment. [13] (level:4)
Subtalar arthroscopy identified pathologies in the subtalar joint in patients with STS and showed that treatment of these pathologies led to improved function. [13] (level:4)Given the preliminary clinical results and present degree of instrument sophistication, one would expect that the excision of an os trigonum and subtalar joint arthrodesis would evolve into mainstay procedures. Moreover, as the definitive value of thermally induced capsule-ligamentous shrinkage is established, the possibility of addressing subtalar instability may be envisioned. [17]
Physical Therapy Management
[edit | edit source]
Since the STS often occurs after an ankle sprain, the foot has been immobilized by a brace or tape during recovery of the joint and the ligaments. Therefore mobilization of the ankle, especially of the subtalar and talocrural joint is necessary in the treatment of STS. Joint mobilization exercises should be done in all directions, but especially in pro- and supination. Also important is they should be executed at full range of motion, provided there is no pain provocation.[2][7]
“'No random control trials for the efficacy of a rehabilitation program for STS are available'.”[2] To influence the tissues in the sinus tarsi, the therapy may consist of friction massages, electrotherapy (for example ultrasound), laser-therapy, cryotherapy and other types of deep massages. The use of ice massage over the lateral ankle may be useful to diminish inflammation and pain.[2][4][7]
Activities should be started as soon as possible, if they can be done without pain. As the peroneal muscles and Achilles tendon tend to weaken when having sinus tarsi, it’s vital to adjust a program therapy to reinforce those muscles. Flexion of the ankle by standing on the toes is a good exercise, and when done on the edge of a stair eccentric exercises can be done for a better strength gain. Stability training is the last stage of the rehabilitation. The patient must do proprioceptive exercises, for example lunges, to improve the proprioception and stability in the ankle.[2][7]
Training programs to improve the stability of the subtalar joint and lower extremity function will be the hallmark of treatment plans for STS. Joint stability relies on passive joint structures, dynamic muscular responses, and neurological control.[8]
The treatment program of STS includes proprioceptive training, balance training, taping and bracing, muscle strengthening exercises and orthese. Some athletes have synovitis of the joint and anti-inflammatory medication would be helpful to reduce the inflammation. Ice on the affected area can help too. [19]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Articles:
• Taillard W, Meyer JM, Garcia J, Blanc Y. The Sinus Tarsi Syndrome. International Orthopaedics (SICOT) 1981; 5:117-130 (level: A1)
• Helgeson K. Examination and Intervention for Sinus Tarsi Syndrome. North American Journal of Sports Physical Therapy 2009 February; 4(1):29-37 (level: A1)
• Rosenberg ZS, Beltran J, Bencardino JT. From the RSNA Refrecher Courses. MR Imaging of the Ankle and Foot. RadioGraphics 2000; 20:153-179 (level: A1)
• K. Helgeson, PT, DHSc ; Examination and Intervention for Sinus Tarsi Syndrome ; orth American Journal of Sports Physical Therapy, 2009;4(1):29-37
• Thermann H, Zwipp H, Tshcernes H. Treatment algorithm of chronic ankle and subtalar instability. Foot Ankle. 1997; 18:163-169
• Kevin Helgeson, Examination and Intervention for Sinus Tarsi Syndrome, N Am Sports Phys ther, feb 2009, 4(1), 29-37 (level: 5)
• FW. Roemer et al, Ligamentous Injuries and the Risk of Associated Tissue Damage in Acute Ankle Sprains in Athletes, N Am Sports med, 2014 april 21, 42(7), 1549-1557 (level: 3A)
Books:
• Meir Nyska, Gideon Mann, editors. The unstable ankle. Chapter 14: Sinus Tarsi Syndrome. United States: Human Kinetics Publishers, Inc. 2002. p144-120
Sites:
• American Academy of Podiatric Sports Medicine. Sinus Tarsi Syndrome. http://www.aapsm.org/sinus_tarsi_syndrome.html (accessed 27/11/2010)
• MyFootShop. Sinus Tarsi Syndrome. http://www.myfootshop.com/detail.asp?Condition=Sinus%20Tarsi%20Syndrome (accessed 28/11/2010)
• PhysioAdviser.com. Sinus Tarsi Syndrome. http://www.physioadvisor.com.au/8074550/sinus-tarsi-syndrome-physioadvisor.htm (accessed 28/11/2010)
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
see tutorial on Adding PubMed Feed
Extension:RSS -- Error: Not a valid URL: Feed goes here!!|charset=UTF-8|short|max=10
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Taillard W, Meyer JM, Garcia J, Blanc Y. The Sinus Tarsi Syndrome. International Orthopaedics (SICOT) 1981; 5:117-130 (level: A1)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 Helgeson K. Examination and Intervention for Sinus Tarsi Syndrome. North American Journal of Sports Physical Therapy 2009 February; 4(1):29-37 (level: A1)
- ↑ 3.0 3.1 Rosenberg ZS, Beltran J, Bencardino JT. From the RSNA Refrecher Courses. MR Imaging of the Ankle and Foot. RadioGraphics 2000; 20:153-179 (level: A1)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Meir Nyska, Gideon Mann, editors. The unstable ankle. Chapter 14: Sinus Tarsi Syndrome. United States: Human Kinetics Publishers, Inc. 2002. p144-120
- ↑ MyFootShop. Sinus Tarsi Syndrome. http://www.myfootshop.com/detail.asp?Condition=Sinus%20Tarsi%20Syndrome (accessed 28/11/2010)
- ↑ American Academy of Podiatric Sports Medicine. Sinus Tarsi Syndrome. http://www.aapsm.org/sinus_tarsi_syndrome.html (accessed 27/11/2010)
- ↑ 7.0 7.1 7.2 PhysioAdviser.com. Sinus Tarsi Syndrome. http://www.physioadvisor.com.au/8074550/sinus-tarsi-syndrome-physioadvisor.htm (accessed 28/11/2010)