Shoulder Subluxation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 86: | Line 86: | ||
http://www.youtube.com/watch?v=Z27B3a1lMdU<br>http://www.youtube.com/watch?v=UeMPc9wcD0I<br> | http://www.youtube.com/watch?v=Z27B3a1lMdU<br>http://www.youtube.com/watch?v=UeMPc9wcD0I<br> | ||
[[Category:Shoulder]] | [[Category:Shoulder]][[Category:Musculoskeletal/Orthopaedics|Orthopaedics]] | ||
Revision as of 13:37, 4 November 2013
Original Editor Bart Moreels
Top Contributors - Wendy Walker, Lucinda hampton, Bart Moreels, Khloud Shreif, Admin, Jana Beckers, Simisola Ajeyalemi, WikiSysop, Fasuba Ayobami, Kim Jackson, Wanda van Niekerk, Amanda Ager, Scott Buxton, Naomi O'Reilly and Joao Costa
Definition[edit | edit source]
Glenohumeral subluxation is defined as a partial or incomplete dislocation that usually stems from changes in the mechanical integrity of the joint. In a subluxation, the humeral head slips out of the glenoid cavity as a result of weakness in the rotator cuff or a blow to the shoulder area. A subluxation can occur in one of three types: anterior (forward), posterior (backward), and inferior (downward).
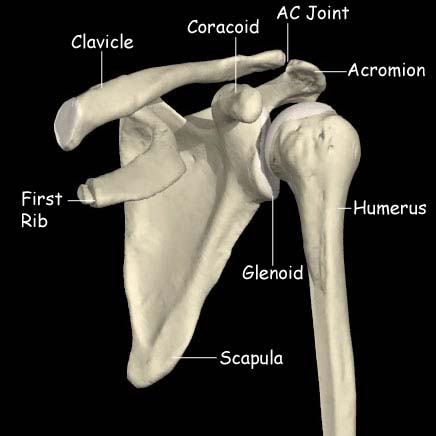
Clinically relevant anatomy[edit | edit source]
The shoulder joint (or glenohumeral joint) consists of 3 bone structures: humerus, scapula and clavicula. These bones make a total of 3 synovial joints: gleno-humeral , sterno-clavicular and acromio-clavicular joint. Besides these you also find the subacromial “joint” and the scapular-thoracal “joint”. The most important muscles acting on the shoulder joint are Deltoid, Supraspinatus,Infrspinatus, Teres minor and major and Pectoralis minor and major. The largest ligament is the Glenohumeral ligament, and this is commonly damaged or overstretched in shoulder joint subluxation. [1].
Epidemiology[edit | edit source]
Studies show that there is no relationship between shoulder pain, shoulder subluxation and gender. It equally occurs within men and women.
Shoulder subluxations frequently occur in people with hemiplegic stroke. The reported incidence varies greatly, from 17% to 81% [2] [3]
Traumatic subluxations of the shoulder can occur in many sports, including football, rugby, wrestling and boxing.
Characteristics/clinical presentation
[edit | edit source]
The main problem with shoulder subluxation is the instability of the gleno-humeral joint. The anatomy of this joint permits a large range of movement, but it sacrifices stability. Research by Basmajian determined that the musculus supraspinatus and in minor ways also the posterior fibres of the deltoid muscle play a key role in maintaining glenohumeralalignment. Chaco and Wolf, did confirm this in their study, which said that the supra spinatus is very important in preventing the downward subluxation of the humerus. Subluxation occurs with the shoulder in abduction and externally rotation.Other research shows that the most important ligamental structure to maintain correct shoulder position and also to prevent shoulder subluxation is the inferior glenohumeral ligament.This ligament is most important during external rotation and abduction during the cocking face of the throwing motion.
Shoulder subluxation can lead to soft tissue damage as traction damage can occur due to gravitational pull forces and poor protection is offered by a weak shoulder.
Diagnostic Procedures[edit | edit source]
Symptoms:
Patients with shoulder subluxations commonly present with:
- Pain in the shoulder region
- Loss of range of movement
- Palpable gap between acromion and humeral head (this can be informally measure in finger-widths)
Functional testing:
The subluxation test is positive = resistance is given, when patient brings arm in throwing stance, in internal rotation direction.
Pain in the ventral capsule indicates a frontal capsule lesion.
Pressure during resistance test on the dorsal part of the humerus can provoke ventral gliding. The result is sudden pain in the shoulder and in a number of cases there is a subluxation to the front. This test can be conducted in different degrees of abduction and with or without the support of the upper arm.
Radiographic measurements are considered to be the most accurate way of evaluating the degree of subluxation[4]
Physical Therapy Management[edit | edit source]
In the hemiplegic patient[edit | edit source]
Sling/support:[edit | edit source]
Traditionally supportive devices, in the form of slings or braces, have been used to manage shoulder subluxation following CVA; the aim being to support the weight of the arm thus preventing/minimising the inferior pull on the humerus and reducing the stretch on the joint capsule. A Cochrane Review [5] in 2009 concluded that there is insufficient evidence to conclude whether supportive devices are of benefit.
Electrical Stimulation:
[edit | edit source]
In a Cochrane Review [6] Functional Electrical Stimulation was found to bring about improvement in pain-free range of passive humeral lateral rotation and to reduce the severity of glenohumeral subluxation; however there was no significant effect on upper limb motor recovery.
Advice/Management:[edit | edit source]
- Teach patient/carers/relatives how to position the limb so that the weight of the arm is supported [7]
- Judicious passive or active assisted exercises should be started within 24 hours poststroke with the aim of maintaining range of movement of the shoulder joint[8]
In the non-hemplegic patient[edit | edit source]
-Prevention of reccurance:
Strengthening exercises to re-establish the strength of the rotator cuff muscles is recommended.
Initial physical therapy interventions may include:
- Mobility exercises including PROM, AAROM, AROM
- Motor control training
- Scapular stabilization
- Isometric and low-grade strengthening exercises
- Manual therapy directed at the Gleno-humeral, Acromio-Clavicular and Sterno-
Clavicular joint
- Manual therapy of cervicothoracic spine and upper ribs
- Activity modification
Late stages of rehabilitation of rotator cuff injury include progressive resistive strengthening, proprioception and sport-specific exercises.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Aras MD, Gokkaya NK, Comert D, Kaya A, et al. (2004). Shoulder pain in hemiplegia: results from a national rehabilitation hospital in Turkey. American Journal of Physical Medicine and Rehabilitation 83(9):713-9.
- ↑ Huang SW, Liu SY, Tang HW, Wei TS, Wang WT, Yang CP. Relationship between severity of shoulder subluxation and soft-tissue injury in hemiplegic stroke patients. J Rehabil Med. 2012 Sep;44(9):733-9.
- ↑ Hartwig M, Gelbrich G, Griewing B. Functional orthosis in shoulder joint subluxation after ischaemic brain stroke to avoid post-hemiplegic shoulder-hand syndrome: a randomized clinical trial. Clin Rehabil. 2012 Sep;26(9):807-16.
- ↑ Paci M, Nannetti L, Rinaldi LA. Glenohumeral subluxation in hemiplegia: An overview. J Rehabil Res Dev. 2005 Jul-Aug;42(4):557-68.
- ↑ Ada L, Foongchomcheay A, Canning C. Supportive devices for preventing and treating subluxation of the shoulder after stroke. Cochrane Database Syst Rev. 2005 Jan 25;(1):CD003863.
- ↑ Price CI, Pandyan AD Electrical stimulation for preventing and treating post-stroke shoulder pain: a systematic Cochrane review Clinical Rehabilitation. Clin Rehabil. 2001;15:5-19.
- ↑ Kaplan MC. Hemiplegic shoulder pain-early prevention and rehabilitation. West J Med. Feb 1995;162(2):151-2
- ↑ Kumar R, Metter EJ, Mehta AJ, Chew T. Shoulder pain in hemiplegia. The role of exercise. Am J Phys Med Rehabil. Aug 1990;69(4):205-8
Visual support:
http://www.youtube.com/watch?v=Z27B3a1lMdU
http://www.youtube.com/watch?v=UeMPc9wcD0I