Shoulder Bursitis: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 45: | Line 45: | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
Bursitis is frequently caused by another medical condition. For example, patients who suffer from subacromial bursitis, are likely to suffer from [http://www.physio-pedia.com/Adhesive_Capsulitis adhesive capsulitis], rotator cuff | Bursitis is frequently caused by another medical condition. For example, patients who suffer from subacromial bursitis, are likely to suffer from [http://www.physio-pedia.com/Adhesive_Capsulitis adhesive capsulitis], rotator cuff tendinopathy, supraspinatus tendinopathy or bicipital tendinopathy.<ref name=":3" /> | ||
Speed’s test is a test to diagnose bursitis. For this test the physician will ask the patient to extend the arm. The physician will then apply resistance while the patient performs an isometric flexion contraction. If the pain increases, the patient may be suffering from bursitis, although other rotator cuff injuries and tendonitis can produce pain with this test. The physician can also let the patient perform Neer’s test to identify the occurrence of an impingement of the rotator cuff. But this test is also sensitive for subacromial bursitis. | Speed’s test is a test to diagnose bursitis. For this test the physician will ask the patient to extend the arm. The physician will then apply resistance while the patient performs an isometric flexion contraction. If the pain increases, the patient may be suffering from bursitis, although other rotator cuff injuries and tendonitis can produce pain with this test. The physician can also let the patient perform Neer’s test to identify the occurrence of an impingement of the rotator cuff. But this test is also sensitive for subacromial bursitis. | ||
Revision as of 00:57, 6 January 2018
Top Contributors - Matthias Proost, Dries Meeusen, Lucinda hampton, Vanderpooten Willem, Mariam Hashem, Rachael Lowe, Fasuba Ayobami, Naomi O'Reilly, Kim Jackson, Admin, Venus Pagare, Wanda van Niekerk, Bouzarpour Faryân and Claire Knott
Definition[edit | edit source]
When the bursae are not irritated and working well, your joints move smoothly and painless.
Bursa is a sac that is filled with liquid that can be find between tissues (bone, skin, tendons and muscle). Because of that fluid the bursa can be use as a cushion that has the function to decrease the friction and the irritation between the tissues that move between each other.[1] When a bursa becomes inflamed and swollen, we speak of a bursitis and you will experience pain during physical activity.
Clinically Relevant Anatomy[edit | edit source]
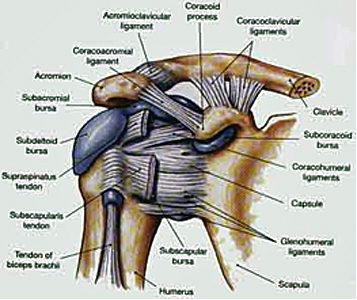
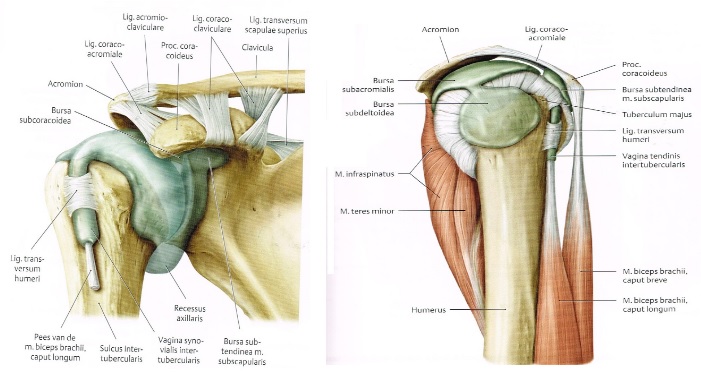
In the shoulder region, we have 8 bursae, the most of any single joint in your body. The major bursae in the shoulder are: the subscapular bursa, the subdeltoid bursa, the subacromial bursa and the subcoracoid bursa. The upper limits of the bursae are the coraco-acromial ligament, acromion bone and the M. deltoid. The under limits are the humeral head, the shoulder joint and the M. supraspinatus.[1]
The bursae do have a nerve supply, for instance the subacromial bursae has suprascapular and axillary nerve endings.[2] Nociceptors such as free nerve endings would give information about painful stimulation and inflammatory responses to the brain. But also mechanoreceptors in the bursae of the shoulder are capable of giving propioceptive information of shoulder joint position.[3] This shows that bursae don’t strictly function as a lubricator between tissues.
There are 6 bursae in and around the shoulder joint:
1) The subscapular bursa or the scapulothoracic bursa: between the tendon of the subscapularis muscle and the shoulder joint capsule.
2) The Subdeltoid bursa: between the deltoid muscle and the shoulder joint cavity.
3) The Subacromial bursa: below the acromion process and above the greater tubercle of the humerus.
4) The Subcoracoid bursa: between the coracoid process of the scapula and the shoulder joint capsule.
5) The Infraspinatus bursa: between the infraspinatus tendon and the capsule of the joint.
6) The subcutaneous acromial bursa: is located above the acromion just beneath the skin.
The subacromial and the subdeltoid bursa are often taken as a single bursa, the subacromial deltoid bursa.[4]
Epidemiology / Etiology[edit | edit source]
Several factors can be related to shoulder bursitis:[5][6]
We can distinguish two major kind of causes: Aseptic and septic. In case the bursitis is caused by the presence of bacteria in the bursa, we speak of a septic bursitis.
There are several conditions to get a bursitis;
- Overload: the repetition of a certain motion too often can lead to the inflammation of the bursa because of the friction between the bursa on the one hand and another structure on the other hand. This can be a tendon, bone, a ligament, …
- Trauma: Due to an accident, the bursa could become irritated and become inflamed.
- Inflamed joint: When the whole joint is inflamed, the bursa can become inflamed as well as other structures. We keep in mind arthritis and gout.
A bursitis could also be related to some professional activities (e.g. painter, …), although, this is not always the case in shoulder bursitis.
Bursitis often develops secondary to injury, impingement, overuse of the muscle, or calcium deposits.
• There are many factors that may cause shoulder bursitis:[7]
• Chronic irritation
• A trauma
• Bacterial infection
• Involved with the inflammatory response of rheumatoid arthritis
• Upper extremity muscle weakness
• Overuse of the adjacent shoulder
• Degeneration of muscle tendons
• Calcium deposition
• Adjacent inflammation of the supraspinatus tendon
• Glenohumeral instability (excessive movement of the joint)
• Degeneration of the acromioclavicular (AC) joint
• Tears of the surrounding rotator cuff
• Impingement by the coraco-acromial ligament
• Coracoid impingement
• Impingement on the posterosuperior aspect of the glenoid
Characteristics / Clinical Presentation[edit | edit source]
Bursitis of the shoulder occurs commonly in people over 30 years old with a greater incidence in females. Younger and middle-aged patients are much more likely to experience acute bursitis than older patients with chronic rotator cuff syndrome.[8]
No significant difference of incidence was found between men and women specific for subacromial bursitis.[7]
Subacromial bursitis typically present with lateral or anterior shoulder pain. Patients only occasionally report a single macro traumatic event leading to persistent pain. Overhead lifting or reaching activities are uncomfortable, and the pain is often worse at night, interrupting sleep. In a study focused on the treatment of subacromial bursitis they state that this type of bursitis has the presence of following symptoms: shoulder pain and limitation of movement for longer than one month but less than one year (after one year it becomes chronic bursitis), the presence of pain during at least one activity (such as sleep, dress, work, grooming and sports) and at the end range of at least one ROM test (scapulothoracic tilting, scapulothoracic abduction, glenohumeral flexion, glenohumeral abduction, internal rotation, external rotation) with also a loss of 10 degrees or more in one or more of these tests.[9]
Patient who suffer from subacromial bursitis should have a glenohumeral abduction greater than 45 degrees to distinguish from patients with established "frozen shoulders".
Frozen shoulder, or adhesive capsulitis, may develop as a consequence of persistent immobility (see link naar de physiopedia pagina van frozen shoulder/adhesieve capsulitis). The subacromial bursitis pattern of symptoms may occur in relation to rotator cuff tears, an impingement syndrome, frozen shoulder, or a systemic inflammatory disorder such as polymyalgia rheumatica (PMR) or rheumatoid arthritis (RA).
Scapulothoracic bursitis results from the mechanical pressure and friction between the superior-medial angle of the scapula and the adjacent ribs. Pain and a “popping” sensation are typical complaints. Aggravating activities include repetitive movements such as working overhead, reaching up and forward, or doing pushups. Local tenderness and palpable crepitus are characteristic. An effusion or hemorrhage into the area may be seen on MRI.
Maintaining your personal hygiene may be difficult as well. For instance movements where you raise your arms above your head, will induce more pain.
Patients who suffer subacromial deltoid or subcoracoid bursitis will experience painful shoulder movements, particularly during activities requiring abduction and extension.
The pain starts gradual, originating deep inside your shoulder and develops over a few weeks or months. The pain is on the outside of the shoulder and may spread towards the elbow.
Activities like washing, where you raise your arm above your head, will worse the pain.
Patients suffering shoulder bursitis may also have interrupted sleep patterns. Rolling over the affected shoulder during sleeping can cause pressure on the inflamed bursa increasing the pain. The pain depends on the degree of inflammation in the shoulder, the range of motion of patients with shoulder bursitis is increased and the shoulder muscles are weaker.[10][7]
Other activities like contact sports are difficult to perform because they can cause more pain. For instance, if someone nudges you against the shoulder it will hurt.
Differential Diagnosis[edit | edit source]
Bursitis is frequently caused by another medical condition. For example, patients who suffer from subacromial bursitis, are likely to suffer from adhesive capsulitis, rotator cuff tendinopathy, supraspinatus tendinopathy or bicipital tendinopathy.[7]
Speed’s test is a test to diagnose bursitis. For this test the physician will ask the patient to extend the arm. The physician will then apply resistance while the patient performs an isometric flexion contraction. If the pain increases, the patient may be suffering from bursitis, although other rotator cuff injuries and tendonitis can produce pain with this test. The physician can also let the patient perform Neer’s test to identify the occurrence of an impingement of the rotator cuff. But this test is also sensitive for subacromial bursitis.
Therefore it is hard to distinguish whether a patient is suffering from bursitis, tendinitis or another injury that usually occurs when the bursa is inflamed. This makes it hard to determine the cause of bursitis when a patient seeks for medical help. One of the methods used by doctors is by extending the arm in front of the body actively. The doctor will try to extend the arm even further away from the patient's body while the patient has to resist this force. If pain occurs, a bursa injury may be the cause of this pain. Nonetheless, this may also mean that indicate a rotator cuff injury or tendinitis, which can give the same kind of pain. The positive impingement test is another example of a diagnostic test, although it doesn’t exclude the other medical conditions that can be confused with bursitis.
To differentiate a bursitis from a supraspinatus tendinitis, which are often confused, we can perform a test to where we isolate the supraspinatus muscle. The patient abducts the arms to 90 degrees with the elbows extended and the arms internally rotated. The arms are placed 30 degrees anteriorly (in the coronal plane), and the patient resists as the examiner forces the arms downward. This is often referred to as the "empty beer can" test.
Frozen shoulder is another medical condition which can be confused with bursitis. In this case, we can differentiate the two symptoms with an easy test: if the patient cannot abduct the arm (glenohumeral abduction), this means the patient has a frozen shoulder. The downside of this test: we can not say with certainty that this patient is suffering from bursitis, only whether this person has a frozen shoulder or not.[11]
Range of Motion Location of pain
Capsular syndrome Restriction of lateral rotation, abduction and medial roation. Pain in C5 dermatome.
Acute bursitis Restriction of abduction. Severe pain in C5 dermatome. Acute onset, no evident preceding trauma.
Acromioclaviculair syndroom Restriction of horizontal adduction. Pain in the area of the acromioclavicular joint and/or C4 dermatome.
Subacromiale syndroom
- rotator cuff tendinitis
- chronic bursitis
- rotator cuff tears No restriction of passive movement. At least one positive resistance test.
Bursitis: variable/little pain, normal power
Tendinitis: pain, normal power
Cuff tears: little pain, loss of power Pain in the C5 dermatome. Painful arc during elevation.
Shoulder calcification Restriction of abduction Pain on the most craniolateral side of the shoulder[2]
Diagnostic Procedures[edit | edit source]
Bursitis can often be diagnosed by physically examining of the patient. By (visual) inspection it is possible to notice some redness and warmth, local tenderness or stiffness in the joint with some swelling when the inflammation is worse.
By x-ray it is possible to confirm the presence of gout crystals and calcification (which means that the bursitis is chronic or recurrent).
With bursa fluid puncture is it possible to rule out infections.
The subacromial deltoid bursa comes into conflict with the acromion. By executing the painful arc, pain will be felt between 70 and 120 degrees of abduction. When the test is positive, we speak of a bursitis sub acromiodeltoid. The movement restriction is not in accordance with the capsular pattern. This means that the abduction is more restricted than the exorotation.
The subcoracoid bursa stands in relation with the anterior joint capsule. We speak of an subcoracoid bursa when the passive exorotation in 90 degrees of abduction is negative and the passive exorotation on 0 degrees is positive.
A test for the scapulothoracic bursa focusses on the strength of the scapular muscles—including the trapezius (upper, middle, and lower), levator scapula, serratus anterior, latissimus dorsi, deltoids, and rotator cuff muscles. A loss of muscle tone or an alteration of scapulothoracic rhythm may lead to increased friction between the medial border of the scapula and the rib cage, resulting in crepitus or snapping.
Snapping scapula is a painful crepitus of the scapulothoracic articulation. This crepitus is a grinding or snapping noise with scapulothoracic motion that may or may not accompany pain. This condition is commonly seen in overhead-throwing athletes. Treatment of patients with this syndrome begins with nonoperative methods; when nonoperative treatment fails, several surgical options exist.[1][4]
Previous to bursitis, there’s always any other pathology which causes bursitis.
It is not rare that people suffering bursitis also have other pathologies. Shoulder bursitis commonly co-exists with different shoulder pathologies (see differential diagnosis), which can make it hard to diagnose. Torn tendons or ligaments can cause as well the irritated bursa.
Shoulder bursitis can be caused due a repeated minor trauma. This can be an overuse of the shoulder joint and muscles according to a more single significant trauma such as a fall for example.[12]
The subacromial bursa lies between the coracoacromial ligament and the supraspinatus muscle. His function is to reduce friction in the space under the acromion. Tests which can include subacromial bursitis are given at the outcome measures.[13]
Bursitis is typically determined by pain or swelling which is localized, tenderness and pain with motion of the affected area tissues. Procedures which can include bursitis or X-ray testing and MRI scanning.
Bursitis is typically identified by localized pain or swelling, tenderness, and pain with motion of the tissues in the affected area. X-ray testing can sometime detect calcifications in the bursa when bursitis has been chronic or recurrent. While MRI scanning can be used to identify bursitis, it is not always necessary.[14]
Outcome Measures[edit | edit source]
The Visual Analogue Scale is filled in by the patient. It is a scale used to describe the pain after the joint is palpated by the physiotherapist.
The DASH-questionnaire, Disability in Arm, Shoulder and Hand-questionnaire, is a 30-item questionnaire that looks at the ability of a patient to perform certain upper extremity activities. This questionnaire is a self-report questionnaire where patients can rate difficulty and interference with daily life on a 5 point Likert scale.
The Shoulder Pain and Disability Index (SPADI) was made to measure shoulder pain and disability. The SPADI contains thirteen items: five of them question pain, eight of them measure disability. The second version of this questionnaire was established to make the tool easier, and the tests take less than 5 minutes to complete.
The Constant-Murley score (CMS) is a 100-points scale composed of a number of individual parameters. These parameters define the level of pain and the ability to carry out the normal daily activities of the patient. The Constant-Murley score was introduced to determine the functionality after the treatment of a shoulder injury. The test is divided into four subscales: pain (15 points), activities of daily living (20 points), strength (25 points) and range of motion: forward elevation, external rotation, abduction and internal rotation of the shoulder (40 points). The higher the score, the higher the quality of the function.
Another scale which we can use is the Shoulder Disability Questionnaire (SDQ). It contains 16 questions about your daily life where shoulder pain can occur. The scale questions you physical, social and emotional restrictions. Using this questionnaire, a functional status of symptoms (pain and / or restricted movement) in the shoulder region can be made.
We can also use the Simple Shoulder Test questionnaire (SST). This is a 12-questions scale about the functioning of the shoulder which the patient must answer with yes or no. The results of this test gives us the possibility to compare the functioning of the shoulder before and after treatment.
Hawkins Test
The examinator has to hold the arm in 90° anteflexion. Next he has to a do passive endoration of the arm by use of his other arm. During this manoeuvre the tuberculum majus appears under the coracoacromial ligament which causes the pain within subacromial bursitis.
The same test is conducted for bankart lesion, which causes pain in the region of the m. deltoid.[15]
Patient stands up, arm alongside the body.
Test: active abduction from 0° to 180°
Test is positive when the patient complains of pain between 60°-120° abduction.
Arm lifted above 120° and the pressure on the bursa decreases.
Background: the subacromial space, becomes smaller during abduction and causes compression of the supraspinatus tendon and the subacromial bursa.[16][17]
Physical Examination[edit | edit source]
Bursitis can often be diagnosed by physically examining of the patient. By (visual) inspection it is possible to notice some redness and warmth, local tenderness or stiffness in the joint with some swelling when the inflammation is worse.
Physical examination of the subacromial bursitis reveals a reduced active range of motion with decreased elevation, internal rotation and abduction, primarily because of pain. The most painful arc of motion is between 70 and 120 degrees of abduction. Tenderness is found laterally below the acromion, anteriorly at the insertion of the supraspinatus tendon on the greater tuberosity and, occasionally, along the supraspinatus muscle belly beneath the trapezius. Strength testing may reveal weakness with internal and external rotation, a finding that demonstrates an important factor in the etiology of these injuries: functional instability due to rotator cuff weakness.
The impingement signs are usually positive. The Neer's sign is performed by forcibly forward flexing the internally rotated arm maximally above 90 degrees. The Hawkin's impingement sign refers to forced internal rotation of the arm performed during forward elevation to 90 degrees. Both tests are considered positive if they produce pain.
Compressiontest (bursa subacromialis)
Test description:
Starting attitude: patient stand or sits down (picture), arms along the body, elbow in 90° flexion.
Therapist stand beyond the patient onto the homolateral side, fixation at the height of the acromion. The moving hand is placed under the elbow and gives pressure in the length direction of the humerus.
Findings:
Test is positive if the patient experiences subacromial pain, this test only puts pressure on a part of the bursa. When the test is positive it can also be due to a tendinitis of the m. supraspinatus. It’s also an axis pressure test for the humerus.[18]
Walch Duplay
The European Society of Shoulder and Elbow Surgery recommended using the Walch-Duplay score which was inspired by the Rowe rating scale and takes into account both subjective and objective data (stability, pain, sport level recovery, mobility) to assess clinical outcome. The Walch-Duplay score is the most currently used score in Europe for the assessment of the patient undergoing shoulder stabilization surgery. However, it is not a self-administrated questionnaire.
The Walch-Duplay score (0 to 100 points) and the WOSI (0 to 2100 points) were recorded at the last follow-up. The Walch-Duplay score is composed of four items: activity, stability, pain and mobility. According to the Walch-Duplay score, results were classified as excellent (91 and 100 points), good (76 and 90 points), fair (51–75 points) or poor (under 50).
The correlation between the Walch-Duplay score and the WOSI is strong. The better the Walch-Duplay score is, the lower the WOSI.[19]
Medical Management[edit | edit source]
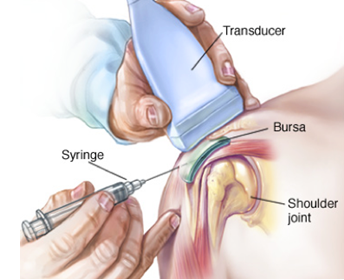
A common treatment for bursitis is the use of injections with or without the use of ultrasound guidance or palpation. These injections could contain steroids or other analgesic substances.
One study examined the use and effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. The conclusion was that botulinum type B can be a useful strategy and that it has a great potential for replacing steroids as a treatment for subacromial bursitis or shoulder impingement syndrome.[14]
Inflammation can also be treated with anti-inflammatory medications such as Motrin, Advil, Aleve, Celebrex, or one of many others. These all fall within the category of 'non-steroidal anti-inflammatory medications.' Taken by mouth, these medications help with the inflammation of the tendons and bursa, and also help reduce the discomfort.[20]
Since the appearance of bursitis is due to another medical condition, treating the cause of this bursitis should be the first step. But since the bursa is still painful, injection is often used to cure this pain. This injection can be in the bursa, or in the muscle itself. A recent study has shown that both methods reduce the pain, but there’s no significant difference between the two methods[2].
Physical Therapy Management[edit | edit source]
Immediate treatment: discontinue all activity, RICE regime to reduce inflammation and treat pain. Then heat to promote blood flow and healing.[21]
The aim of the therapy:
1) Reduce the symptoms
2) Minimize damage
3) Maintain rotator cuff motion and strength
The first step in treating bursitis is applying cold to the bursa. It will help decrease the swelling and redness around the bursa.
Apply ice every day 12-20 minutes.
In the acute stage, also use Codman’s pendulum exercises and AAROM exercises.[22]
Once the inflammation has been reduced, you can begin using ultrasound therapy to continue the healing process.[23]
For the best of the recovery, it is designated to keep the joint in motion. This will prevent that the joint becomes stiff and the recovery process is slowed down.
Since the appearance of bursitis is due to another medical condition, treating the cause of this bursitis should be the first step. One of these causes can be a rotator cuff tendinopathy, and so we first have to treat this pathology.
But since the bursa is still painful, injection is often used to cure this pain. This injection can be in the bursa, or in the muscle itself. A recent study has shown that both methods reduce the pain, but there’s no significant difference between the two methods.[2]
We can use ultrasound-guided injection or palpation-guided injection. Study shows us that the ultrasound-guided injection is more precisely to find the exact location of the bursa/muscle which we are planning to inject in.[3][24]
The best initial approach for a scapulothoracic bursitis is a nonoperative treatment plan that combines scapular strengthening, postural reeducation, and core strength endurance. The addition of local modalities, nonsteroidal antiinflammatory drugs, and localized injections may also be helpful. If an appropriate trial of nonoperative management proves unsuccessful, surgical correction can produce good results.[1]
One study focusing on the treatment of subacromial bursitis they examined the difference between one group treated with ultrasound-guided injection (UGI) and another group with ultrasound-guided injection and home exercise program (UGI-exercise) for 1 month. The exercises included exercises for shoulder lowering with decoaptation that the patient must remember to reproduce during all the common daily activities. Another exercise is assisted active self-mobilization for the recovery of range of motion in all directions. Also isometric strengthening with elastic bands of rotator cuff muscles and deltoid was an exercise given to this patients. A last exercise is the stretching in elevation, abduction and rotation performed statically by placing the patient-specific postures that allow the lengthening of the shortened muscles and the recovery of the last degrees of movement. The conclusion in this article is that ultrasound-guided injection combined with shoulder exercises in the treatment of subacromial bursitis is effective to relieve pain in the short and medium term.[25]
Once the pain starts to diminish, the physiotherapist will set up an individualized shoulder strengthening and stretching exercise program. It is important to strengthen your muscles properly as they may have weakened during the period of non-use.
Patients with shoulder bursitis can learn ways to move the shoulder that will not cause inflammation.[12]
Here are a few exercises that can be built up progressively:
Table Slides (Flexion): Start with your hand on a table (facing the table) on a towel as shown below, Stretch your arm forward on the table by sliding the towel. Feel a stretch under your arm. Do 20-30 repetitions. This exercise is modified for abduction as well.
Scapular wall slides: Stand in an upright position with your back against the wall. Raise your arms in 90 degrees abduction and flex your elbows to the 90 degree position as well. Your arms have to be pressed against the wall at all times. Make sure your handpalms are facing forward. Now you will abduct your arms as high as you can while extending the elbows at the same time. Do this slowly and go back to the starting position. Do 10 – 12 repititions.[22]
Upper Trap (UT): Sit on a table or chair and use the hand of the affected side to grip under the table, stabilizing the shoulder downward. With the opposite hand, pull the head to the opposite shoulder, maintaining your gaze forward and feeling a stretch in the upper trap muscle. Hold for 30 seconds and do 1-3 repetitions two times a day. [23]
Open Book Stretch: Placed a rolled up towel on a mat table between the shoulder blades and lie flat on your back. Keep your arms folded together over
the top of your body, with your hands together. Open your arms up, similar to the second picture, like you are simulating the opening of a book, feeling a stretch in the front of your shoulder. Hold for 30-60 seconds and do 1-3 repetitions two times a day.
Rowing (using a theraband): This is a good exercise to train the scapular stabilizing muscles.[24]
Sit in a chair as shown or stand. Anchor a theraband to a door or pole, making sure that the anchor point is around
chest level. Pull the theraband backwards most importantly pulling the shoulder blades together. Do two sets of 10-20 repetitions three times a week.
Low Row Isometric: Push your hand back into the table as shown in the picture. Think like you are trying to push your shoulder blade down into your back pocket. Do 20 repetitions and hold each for five seconds.[1]
Key Evidence[edit | edit source]
Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61. Level of evidence: 1B
Resources[edit | edit source]
Websites:
http://www.webmd.com/pain-management/understanding-bursitis-basics#1
http://www.medicinenet.com/shoulder_bursitis/patient-comments-763-page4.htm
http://www.orthopaedicscore.com/scorepages/disabilities_of_arm_shoulder_hand_score_dash.html
http://www.orthop.washington.edu/?q=patient-care/articles/shoulder/simple-shoulder-test.html
www.err.eg.net/articles/2014/41/4/images/EgyptRheumatolRehabil_2014_41_4_172_147360_t4.jpg
http://www.orthopaedicscore.com/scorepages/constant_shoulder_score.html
http://www.drplace.com/Upper_extremity_bursitis.16.23039.htm
Book:
Moore, et al. Clinical oriented anatomy, 2014, 7th edition
Clinical Bottom Line[edit | edit source]
Shoulder bursitis is a common cause of shoulder pain. This bursitis is in most cases caused by an overload, trauma, an inflamed joint or elder age as it lays between different structures such as muscles, bones or other structures. Since it’s mostly caused by another pathology nearby, it is very difficult to differentiate these many shoulder pathologies. Pain, a decrease in range of motion, loss of strength and loss of functionality are the main complaints of the patients. There is evidence that injection of pain reducers by using ultrasound guided-injection in combination with physical therapy are beneficial for the recovery.
Recent Related Research[edit | edit source]
Warth, Ryan J., Ulrich J. Spiegl, and Peter J. Millett. "Scapulothoracic Bursitis and Snapping Scapula Syndrome A Critical Review of Current Evidence." The American journal of sports medicine 43.1 (2015): 236-245.
Level of evidence: 1A
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Conduah, Augustine H., and Champ L. Baker. "Clinical management of scapulothoracic bursitis and the snapping scapula." Sports Health: A Multidisciplinary Approach 2.2 (2010): 147-155
- ↑ 2.0 2.1 2.2 2.3 Chang, Won Hyuk, et al. "Comparison of the therapeutic effects of intramuscular subscapularis and scapulothoracic bursa injections in patients with scapular pain: a randomized controlled trial." Rheumatology international34.9 (2014): 1203-1209
- ↑ 3.0 3.1 Hsieh, Lin-Fen, et al. "Is ultrasound-guided injection more effective in chronic subacromial bursitis?." Medicine and science in sports and exercise 45.12 (2013): 2205-2213.
- ↑ 4.0 4.1 Hitzrot, James Morley. "Surgical diseases of the shoulder bursae." Annals of surgery 98.2 (1933): 273.
- ↑ Van Alfen N, Van Engelen B, Van Der Tas P, Walravens C, onderzoek en behandeling van de schouder, Bohn stafleu van Loghum,2007
- ↑ H. B. Skinner, Current Diagnosis & treatment in orthopaedics, the McGraw-Hills companies, 2008.
- ↑ 7.0 7.1 7.2 7.3 Walker‐Bone, Karen, et al. "Prevalence and impact of musculoskeletal disorders of the upper limb in the general population." Arthritis Care & Research 51.4 (2004): 642-651.
- ↑ J. Willis Hurst, Douglas C. Morris, Chest pain, Futura publishing company, 2001.
- ↑ Downing, Deborah Swan, and Arthur Weinstein. "Ultrasound therapy of subacromial bursitis A double blind trial." Physical therapy 66.2 (1986): 194-199
- ↑ Salzman, Keith L., W. A. Lillegard, and J. D. Butcher. "Upper extremity bursitis." American family physician 56 (1997): 1797-1814
- ↑ Downing, Deborah Swan, and Arthur Weinstein. "Ultrasound therapy of subacromial bursitis A double blind trial." Physical therapy 66.2 (1986): 194-199
- ↑ 12.0 12.1 O. Dreeben-Irimia, introduction to physical therapy for physical therapist assistants, 2011, p 84-85.
- ↑ Bakker J F, Jongh L de, Jonquiere M, et al. Standaard Schouderklachten. Huisarts en Wetenschap 1990; 33:196-202
- ↑ 14.0 14.1 Lee JH, Lee SH, Song SH. Clinical effectiveness of botulinum toxin type B in the treatment of subacromial bursitis or shoulder impingement syndrome. Clinical journal Pain. 2011 Jul-Aug: 27 page 523 - 528
- ↑ Hardwick DH, Beebe JA, McDonnell MK, Lang CE. A comparison of serratus anterior muscle activation during a wall slide exercise and other traditional exercises. Journal of Orthopedic Sports Physical Therapy, 2006 December: 36(12) page 903 – 910.
- ↑ Lee S, Park J, Lee D. The Effects of Cervical Stabilization Exercises on the Electromyographic Activity of Shoulderstabilizers. Journal Of Physical Therapy Science, 2013 December: 12 page 1557 - 1660
- ↑ Gardner E. The innervation of the shoulder joint. The Anatomical Record,1948:102 page 1-18.
- ↑ Ide K, Shirai Y, Ito H, Ito H. Sensory nerve supply in the human subacromial bursa. Journal of Shoulder and Elbow Surgery, 1996 September – October: 5 page 371 – 382.
- ↑ Mamiko Noguchi, Jaclyn N. Chopp, Stephanie P. Borgs, Clark R. Dickerson. Scapular orientation following repetitive prone rowing: Implications for potential subacromial impingement mechanisms. Journal of Electromyography and Kinesiology, 2013 Decemeber: 23 page 1356 – 61
- ↑ Cluett J., Shoulder bursitis treatment, 2009
- ↑ Walker B., The anatomy of sports injuries, lotus publishing, 2007, p 131-132
- ↑ 22.0 22.1 O. Dreeben, physical therapy clinical handbook, Jones and Barlett, 2008, p209-211.
- ↑ 23.0 23.1 Williams, bursitis of the shoulder, home therapy, 2001
- ↑ 24.0 24.1 Chen, Max JL, et al. "Ultrasound-guided shoulder injections in the treatment of subacromial bursitis." American journal of physical medicine & rehabilitation 85.1 (2006): 31-35.
- ↑ Gasparre, Giuseppe, et al. "Effectiveness of ultrasound-guided injections combined with shoulder exercises in the treatment of subacromial adhesive bursitis." Musculoskeletal surgery 96.1 (2012): 57-61.