Scapular Dyskinesia
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (14/04/2023)
Introduction[edit | edit source]
The condition of abnormal mobility or function of the scapula is called scapular dyskinesis (SD).[1][2]
Scapular dyskinesis is not a specific injury in itself; rather it is hypothesized to be an alteration in scapular function as a reaction to changes within its bony and muscular environment.[3]
Scapular winging has been used as a term synonymous with dyskinesis; however, it refers to an abnormal prominence of the scapula as a result of its elevation from the chest wall. This can cause a static prominence of the scapula or a dynamic dysfunction of the normal, smooth scapulothoracic motion, known as scapular dyskinesis or dysrhythmia. [4][5]
Scapular dyskinesis can be present in healthy individuals as in patients with shoulder pathology.[6] According to data reported in the literature, SD incidence is frequent in patients with shoulder diseases, including RC diseases, GH instability, impingement syndrome, and labral tears.[7]
Scapular Biomechanics[edit | edit source]
Typical movement of the scapula occurs in the sagittal, coronal, and transverse planes. The primary movements consist of two translations: superior/inferior, and protraction/ retraction, as well as three rotations: upward/downward, internal/external, and anterior/posterior. Upward rotation is primary and posterior tilt is secondary during normal overhead UE elevation with internal/external rotation being minimal until 100°. [8],[9]
A review of the normal ratio of glenohumeral (GH) to scapulothoracic (ST) motion analyzed by Doody et al[10] under three-dimensional analysis found that the ratio of GH to ST motion changes from 7.3: 1 in the first 30° of elevation to 0.78: 1 between 90 and 150°. Bagg and Forrest found a ratio of 4.4:1 during the early phase and 1.7:1 within 80 to 140° of shoulder elevation.[11]
Etiology[edit | edit source]
The causes of scapular dyskinesis can be split into three groups:
- Shoulder-related;
- Neck-related;
- Posture-related. [12]
1. Shoulder related: The most common pathologies that are associated with some form of scapular dyskinesis are (1) acromioclavicular instability, (2) shoulder impingement, (3) rotator cuff injuries, (4) glenoid labrum injuries, (5) clavicle fracture and (6) nerve-related. The common characteristic of all these pathologies is the disturbance of the scapulohumeral rhythm. [13][14]
The soft tissues that surround the shoulder have been linked to the development of altered scapular mechanics. [15] Inflexibility and stiffness of the pectoralis minor and short head of the biceps muscles create anterior tilt and protraction as a result of their pull on the coracoid. [16] Furthermore, stiffness of the posterior aspect of the glenohumeral capsule shows an altered resting scapular position, further anteriorly compared to normal individuals, a similar pattern to shoulder impingement. [9]
2. Neck-related: There are two subtypes of neck pathologies that can affect the shoulder: a) “mechanical neck pain” syndromes and b) cervical nerve root-related syndromes. [12]
3. Posture-related: Excessive thoracic kyphosis and cervical lordosis alter the resting position of the scapula. Athletes are more susceptible to these changes. Depending on their sport, they develop core muscle imbalances that alter spinal curvatures and soft tissue tensions. [17]
Clinical Presentation[edit | edit source]
Burkhart et al [18] have used the acronym SICK to refer to the syndrome associated with scapular dyskinesia. “SICK” Scapula Syndrome refers to Scapular Malpositioning, Inferior medial border prominence, Coracoid pain and malposition, and DysKinesis of scapular movement.
Symptomatic patients with an isolated SICK scapula may complain of anterior shoulder pain, posterosuperior scapular pain, superior shoulder pain, proximal lateral arm pain, or any combination of the above. In addition, posterosuperior scapular pain may radiate into the ipsilateral para spinous cervical region or the patient may complain of radicular/thoracic outlet-type symptoms into the affected arm, forearm, and hand or any combination of the above. [18]
Scapular dyskinesis is also highly prevalent in the absence of shoulder symptoms. [19]
Clinical Examination[edit | edit source]
Current tests and measures, while proven to be reliable, have not altogether shown strong validity by demonstrating a correlation with biomechanical motion, symptoms, pathology, or outcomes.[20]
Determining The Presence or Absence of Dyskinesia[edit | edit source]
A good screening tool for the presence of SD is the yes/no method that categorizes abnormal shoulder types I, II, and III of SD into the “yes” category and type IV into the “no” category. [21]
Manually Assisted Movements of Scapula[edit | edit source]
To evaluate if scapular position contributes to shoulder pain, symptom alteration tests have been developed, where the scapula is manually assisted during provocation testing. Two tests are involved in this step, the scapular assistance test (SAT) and the scapular reposition (retraction) test (SRT). [22]
The SAT involves the examiner pushing the inferior-medial border of the scapula outwards and upwards whilst stabilizing the upper medial border when the patient has his humerus elevated. This test assesses how differently the pain is perceived. In a positive test, the pain is reduced and it is usually positive in patients with painful arc or shoulder impingement. There are no false positives in asymptomatic patients. [23][24][25]
In SRT the examiner has to position and stabilize the medial scapular border with one hand, whilst the patient is asked to elevate his arm isometrically (no change in the angle of the joint) against the examiner’s other hand. Again the test is positive when this maneuver reduces the pain felt by the patient. This test is also positive if the patient’s strength is increased during the isometric elevation of the arm. The scapular reposition test is sufficiently specific and sensitive in rotator cuff injuries. [26]
Assessment of Surrounding Structures[edit | edit source]
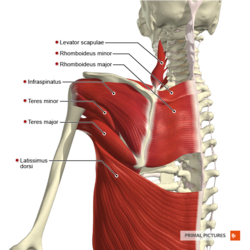
The structures around the scapula (thoracic spine, the acromioclavicular joint, rotator cuff muscles, two heads of the biceps, and the glenoid labrum) are assessed. It is important to assess these structures thoroughly in order to exclude or confirm alternative causes of the symptoms. The assessor is looking for symptoms (pain, loss of function) in other structures, soft tissue laxity, and muscle power. [26]
The sternoclavicular (SC) and acromioclavicular (AC) joints should be evaluated for instability, and the clavicle should be evaluated for angulation, shortening, or malrotation. Anterior-posterior (AP) laxity of the AC joint is evaluated clinically by stabilizing the clavicle with one hand while grasping and mobilizing the acromion in an AP direction with the other hand. [27]
The infraspinatus strength test showed good reliability to assess infraspinatus weakness due to SD. [7]
Muscle Tests[edit | edit source]
Three muscle tests: manual resistance of the arm at 130° of flexion (targets the serratus anterior), [28] [29] manual resistance of the arm at 130-150° of abduction (targets the lower and middle trapezius),[28] and extension of the arm at the side (targets the rhomboids) [30]should be performed.
The distinction between these testing maneuvers and other muscle tests for the shoulder is that the clinician attempts to “break” the patient’s arm position and observe if the scapula is visibly moving out of position. The combination of both the break in position and scapular movement is suggestive of scapular muscle weakness. [31]
Core Evaluation[edit | edit source]
In the low row test, the patient is asked to place his or her arm in slight humeral extension and then instructed to resist movement of the arm into forward flexion. The examiner (positioned posterior to the patient) then instructs the patient to contract the gluteal muscles while applying the same anterior force on the arm. If strength increases with the gluteal contraction, this is an indication that scapular and shoulder muscle activation may be facilitated by involving hip and core strength, which suggests lower extremity/core strengthening should be included in the treatment plan for the shoulder. [31]
Physiotherapy Management[edit | edit source]
Conservative treatment in SD cases aims to restore scapular retraction, posterior tilt, and external rotation. Specific exercises for scapular rehabilitation include flexibility exercises to decrease scapular traction, and scapular stabilization exercises to optimize scapular kinematics. [7]
The traction on scapular posture can be reduced by performing exercises that increase muscle flexibility.[32] [33] Stretching exercises with shoulder horizontal abduction at 90◦ and 150◦ of elevation have been demonstrated to be useful in increasing pectoralis minor flexibility and the ER and posterior tilt of the scapula during forward elevation. [32][33][34]
Scapular stabilization exercises, based on stretching and strengthening, aim to improve muscle strength and joint position sense [35] [36] [37] The serratus anterior and trapezius muscles act as scapular stabilizers. The serratus anterior plays an essential role in determining scapular ER and posterior tilt, and the lower trapezius helps to stabilize the scapular position. Scapular stabilization exercises are based on closed and open kinetic chain exercises, including push-ups on a stable or unstable surface, lawnmower exercises, and resisted scapular retraction.[35] [37]
Push-ups on a stable surface improve the serratus anterior stretch and, when Red Cord slings are used, general muscle strength improvements are obtained[38]; the same exercise, performed on an unstable surface, increases the activation of the trapezius while decreasing the activation of the serratus anterior[39].
The upper and lower trapezius muscles can be better stimulated with upward rotation shrugs[40]. Specific shrug exercises may be beneficial to increase the upward rotation angle and the upper trapezius activity in subjects with SD and the corresponding scapular downward rotation syndrome[41]. Although they could be classified as short lever exercises, maneuvers such as scapular shrugging or elevation should be avoided in the first 4-6 weeks of rehabilitation. This is intentional to not overly bias the upper trapezius which could delay the restoration of balance amongst scapular muscle activation. [31]
In a review article[7] the effects of the Kinesio taping method have also been evaluated. For type II SD, the placement of Kinesio taping over the upper and lower trapezius muscles may rebalance the scapular muscles, increasing the upward scapular rotation[42]; on the other hand, they do not induce changes in the electromyographic activity of serratus anterior, upper and lower trapezius muscles. No alteration in isometric force during shoulder flexo-abduction and external rotation has been shown[43].
Presentations[edit | edit source]
 |
Advanced Exercises for the Upper Quarter: A How To Guide for Scapular Motor Control Rehabilitation
This presentation, created by Stephanie Pascoe as part of the OMPT Fellowship in 2010, describes a how to guide for scapulothoracic rehabilitation. It includes some great animations! |
References[edit | edit source]
- ↑ Depreli Ö, Angın E. Review of scapular movement disorders among office workers having ergonomic risk. Journal of back and musculoskeletal rehabilitation. 2018 Jan 1;31(2):371-80.
- ↑ Longo UG, Petrillo S, Candela V, Rizzello G, Loppini M, Maffulli N, Denaro V. Arthroscopic rotator cuff repair with and without subacromial decompression is safe and effective: a clinical study. BMC Musculoskeletal Disorders. 2020 Dec;21:1-8.
- ↑ Saini SS, Shah SS, Curtis AS. Scapular dyskinesis and the kinetic chain: recognizing dysfunction and treating injury in the tennis athlete. Current Reviews in Musculoskeletal Medicine. 2020 Dec;13:748-56.
- ↑ Humphrey CS, Sears BW, Curtin MJ. An anthropometric analysis to derive formulae for calculating the dimensions of anatomically shaped humeral heads. Journal of Shoulder and Elbow Surgery. 2016 Sep 1;25(9):1532-41.
- ↑ Kibler WB, Sciascia AD. Disorders of the scapula and their role in shoulder injury. Gewerbestrasse, Switzerland: Springer International Publishing. 2017:128-30.
- ↑ Teixeira DC, Alves L, Gutierres M. The role of scapular dyskinesis on rotator cuff tears: a narrative review of the current knowledge. EFORT Open Reviews. 2021 Oct;6(10):932.
- ↑ 7.0 7.1 7.2 7.3 Giuseppe LU, Laura RA, Berton A, Candela V, Massaroni C, Carnevale A, Stelitano G, Schena E, Nazarian A, DeAngelis J, Denaro V. Scapular dyskinesis: from basic science to ultimate treatment. International journal of environmental research and public health. 2020 Apr;17(8):2974.
- ↑ Ludewig PM et al. Motion of the shoulder complex during multiplaner humeral elevation. J Bone Joint Surg. Am.2009;91:378-389.
- ↑ 9.0 9.1 McClure PW et al. Direct 3-dimentional measurement of scapular kinematics during dynamic movements in vivo.J Shoulder Elbow Surg.2001:10:269-277.
- ↑ Doody SG et al.Shoulder movements during abduction in the scapular plane.Arch Phys Med Rehab.1970:595-604.
- ↑ Bagg SD, Forrest Wj. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane.Arch Phys Med Rehabil.1988:238-245.
- ↑ 12.0 12.1 Panagiotopoulos AC, Crowther IM. Scapular Dyskinesia, the forgotten culprit of shoulder pain and how to rehabilitate. SICOT-J. 2019;5.
- ↑ Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003 Apr 1;19(4):404-20.
- ↑ Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. British journal of sports medicine. 2010 Apr 1;44(5):300-5.
- ↑ Borstad JD. Resting position variables at the shoulder: evidence to support a posture-impairment association. Physical Therapy. 2006 Apr 1;86(4):549-57.
- ↑ Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. Journal of orthopaedic & sports physical therapy. 2005 Apr;35(4):227-38.
- ↑ Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clinical biomechanics. 2008 Feb 1;23(2):184-92.
- ↑ 18.0 18.1 The disabled throwing shoulder: spectrum of pathology part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitationfckLRBurkhart, Stephen S et al.fckLRArthroscopy , Volume 19 , Issue 6 , 641 - 661
- ↑ Pires ED, Camargo PR. Analysis of the kinetic chain in asymptomatic individuals with and without scapular dyskinesis. Clinical Biomechanics. 2018 May 1;54:8-15.
- ↑ Kuhn JE.Physical examination of the scapula -a systematic review.JOSPT.2009;39:A11.
- ↑ Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy: the journal of arthroscopic & related surgery. 2009 Nov 1;25(11):1240-8.
- ↑ Kopkow C, Lange T, Schmitt J, Kasten P. Interrater reliability of the modified scapular assistance test with and without handheld weights. Manual therapy. 2015 Dec 1;20(6):868-74.
- ↑ Kibler WB, Sciascia AD. Introduction to the second international conference on scapular dyskinesis in shoulder injury—the ‘Scapular summit’report of 2013. British journal of sports medicine. 2013 Sep 1;47(14):874-.
- ↑ Kibler BW, McMullen J. Scapular dyskinesis and its relation to shoulder pain. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2003 Mar 1;11(2):142-51.
- ↑ Kibler WB. The scapula in rotator cuff disease. Rotator Cuff Tear. 2012;57:27-40.
- ↑ 26.0 26.1 Kilber WB, Sciascia A (2010) Current concepts: scapular dyskinesis. British Journal of Sports Medicine. 44, 300–305. [CrossRef] [PubMed] [Google Scholar]
- ↑ Kibler BW, Sciascia A, Wilkes T. Scapular dyskinesis and its relation to shoulder injury. JAAOS-journal of the American academy of orthopaedic surgeons. 2012 Jun 1;20(6):364-72.
- ↑ 28.0 28.1 Michener LA, Boardman ND, Pidcoe PE, Frith AM. Scapular muscle tests in subjects with shoulder pain and functional loss: reliability and construct validity. Physical therapy. 2005 Nov 1;85(11):1128-38.
- ↑ Ekstrom RA, Soderberg GL, Donatelli RA. Normalization procedures using maximum voluntary isometric contractions for the serratus anterior and trapezius muscles during surface EMG analysis. Journal of Electromyography and Kinesiology. 2005 Aug 1;15(4):418-28.
- ↑ Ginn KA, Halaki M, Cathers I. Revision of the Shoulder Normalization Tests is required to include rhomboid major and teres major. Journal of Orthopaedic Research. 2011 Dec;29(12):1846-9.
- ↑ 31.0 31.1 31.2 Sciascia A, Kibler WB. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. International Journal of Sports Physical Therapy. 2022;17(2):117.
- ↑ 32.0 32.1 Umehara J, Nakamura M, Nishishita S, Tanaka H, Kusano K, Ichihashi N. Scapular kinematic alterations during arm elevation with decrease in pectoralis minor stiffness after stretching in healthy individuals. Journal of shoulder and elbow surgery. 2018 Jul 1;27(7):1214-20.
- ↑ 33.0 33.1 Umehara J, Nakamura M, Fujita K, Kusano K, Nishishita S, Araki K, Tanaka H, Yanase K, Ichihashi N. Shoulder horizontal abduction stretching effectively increases shear elastic modulus of pectoralis minor muscle. Journal of shoulder and elbow surgery. 2017 Jul 1;26(7):1159-65.
- ↑ Morais N, Cruz J. The pectoralis minor muscle and shoulder movement-related impairments and pain: Rationale, assessment and management. Physical Therapy in Sport. 2016 Jan 1;17:1-3.
- ↑ 35.0 35.1 Struyf F, Nijs J, Meeus M, Roussel NA, Mottram S, Truijen S, Meeusen R. Does scapular positioning predict shoulder pain in recreational overhead athletes?. International journal of sports medicine. 2013 Jul 3:75-82.
- ↑ Başkurt Z, Başkurt F, Gelecek N, Özkan MH. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. Journal of back and musculoskeletal rehabilitation. 2011 Jan 1;24(3):173-9.
- ↑ 37.0 37.1 Turgut E, Duzgun I, Baltaci G. Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2017 Oct 1;98(10):1915-23.
- ↑ De Mey, K.; Danneels, L.; Cagnie, B.; Borms, D.; T’Jonck, Z.; Van Damme, E.; Cools, A.M. Shoulder muscle activation levels during four closed kinetic chain exercises with and without Redcord slings. J. Strength Cond. Res. 2014, 28, 1626–1635. [CrossRef]
- ↑ Pirauá AL, Pitangui AC, Silva JP, dos Passos MH, de Oliveira VM, Batista LD, de Araújo RC. Electromyographic analysis of the serratus anterior and trapezius muscles during push-ups on stable and unstable bases in subjects with scapular dyskinesis. Journal of Electromyography and Kinesiology. 2014 Oct 1;24(5):675-81.
- ↑ Pizzari T, Wickham J, Balster S, Ganderton C, Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clinical biomechanics. 2014 Feb 1;29(2):201-5.
- ↑ Lee JH, Cynn HS, Choi WJ, Jeong HJ, Yoon TL. Various shrug exercises can change scapular kinematics and scapular rotator muscle activities in subjects with scapular downward rotation syndrome. Human movement science. 2016 Feb 1;45:119-29.
- ↑ Huang TS, Ou HL, Lin JJ. Effects of trapezius kinesio taping on scapular kinematics and associated muscular activation in subjects with scapular dyskinesis. Journal of Hand Therapy. 2019 Jul 1;32(3):345-52.
- ↑ Intelangelo L, Bordachar D, Barbosa AW. Effects of scapular taping in young adults with shoulder pain and scapular dyskinesis. Journal of Bodywork and Movement Therapies. 2016 Jul 1;20(3):525-32.