Scapular Dyskinesia
This article is currently under review and may not be up to date. Please come back soon to see the finished work! (14/04/2023)
Introduction[edit | edit source]
The condition of abnormal mobility or function of the scapula is called scapular dyskinesis (SD).[1][2]
Scapular dyskinesis is not a specific injury in itself; rather it is hypothesized to be an alteration in scapular function as a reaction to changes within its bony and muscular environment.[3] Scapular winging is however a clinical observation wherein any part of the scapular departs excessively from the thorax soon after movement is initiated and persists in its disconnect fashion throughout the arm movement.
Scapular dyskinesis can be present in healthy individuals as in patients with shoulder pathology.[4] According to data reported in the literature, SD incidence is frequent in patients with shoulder diseases, including RC diseases, GH instability, impingement syndrome, and labral tears.[5]
Scapular Biomechanics[edit | edit source]
Typical movement of the scapula occurs in the sagittal, coronal, and transverse planes. The primary movements consist of two translations: superior/inferior, and protraction/ retraction, as well as three rotations: upward/downward, internal/external, and anterior/posterior. Upward rotation is primary and posterior tilt secondary during normal overhead UE elevation with internal/external rotation being minimal until 100°. [6],[7]
Review of the normal ratio of glenohumeral (GH) to scapulothoracic (ST) motion analysed by Doody et al[8] under three-dimensional analysis found that the ratio of GH to ST motion changes from 7.3: 1 in the first 30° of elevation to 0.78: 1 between 90 and 150°. Bagg and Forrest found a ratio of 4.4:1 during early phase, and 1.7:1 within 80 to 140° of shoulder elevation.[9]
Etiology[edit | edit source]
The causes of scapular dyskinesis can be split into three groups:
- Shoulder-related;
- Neck-related;
- Posture-related . [10]
1.Shoulder-related: The most common pathologies that are associated with some form of scapular dyskinesis are: (1) acromioclavicular instability, (2) shoulder impingement, (3) rotator cuff injuries, (4) glenoid labrum injuries, (5) clavicle fracture and (6) nerve-related. The common characteristic of all these pathologies is the disturbance of the scapulohumeral rhythm. [11][12]
The soft tissues that surround the shoulder have been linked to the development of altered scapular mechanics. The tightness of the muscles of the pectoral region promotes anterior translation of the shoulder girdle and consequently the scapula. [13] Furthermore, stiffness of the posterior aspect of the glenohumeral capsule shows an altered resting scapular position, further anteriorly compared to normal individuals, a similar pattern to shoulder impingement. [7]
2.Neck-related: There are two subtypes of neck pathologies that can affect the shoulder: a) “mechanical neck pain” syndromes and b) cervical nerve root-related syndromes. [10]
3.Posture-related: Excessive thoracic kyphosis and cervical lordosis alter the resting position of the scapula. Athletes are more susceptible to these changes. Depending on their sport, they develop core muscle imbalances that alter spinal curvatures and soft tissue tensions. [14]
Clinical Presentation[edit | edit source]
Burkhart et al [15] has used the acronym SICK to refer to the syndrome associated with scapular dyskinesia. “SICK” Scapula Syndrome refers to Scapular Malpositioning, Inferior medial border prominence, Coracoid pain and malposition and DysKinesis of scapular movement.
Symptoms of isolated SICK scapula: anterior shoulder pain (most common), posterior superior scapular pain, superior shoulder pain, proximal lateral arm pain or any combination of above. Posterosuperior scapular pain may radiate into the ipsilateral paraspinous cervical region or patient may complain of radicular/TOS type symptoms. The onset is almost always insidious.
Clinical Examination[edit | edit source]
Current tests and measures, while proven to be reliable, have not altogether shown strong validity by demonstrating correlation with biomechanical motion, symptoms, pathology, or outcomes.[16]
Recommendations for appropriate clinical measures include:
1. Determining the presence or absence of dyskinesia[edit | edit source]
A good screening tool for the presence of SD is the yes/no method that categorizes abnormal shoulder types I, II, and III of SD into the “yes” category and type IV into the “no” category. [17]
Kibler classification of scapular dysfunction: [12]
- Type I or Inferior dysfunction: The primary external visual feature is the prominence of the inferior angle as a result of anterior tilting of the scapula in the sagittal plane. Inferior pattern presentation is better visualised while in the hands-on-hips position or during eccentric lowering from overhead elevation. According to Kibler, Type 1 pattern is most commonly found in patients with rotator cuff dysfunction.
- Type 2 or Medial dysfunction: The primary external visual feature is the prominence of the entire medial scapular border due to internal rotation of the scapula in the transverse plane. As with Type 1, the Type 2 presentation becomes more evident in the hands-on-hips position and during active eccentric lowering from overhead. Medial pattern dysfunction most often occurs in patients with glenohumeral joint instability.
- Type 3 or Superior dysfunction: Characterised by excessive and early elevation of the scapula during UE elevation. This pattern has been referred to as compensatory shoulder hiking or shrug and is most often seen in patients with rotator cuff dysfunction and deltoid-rotator cuff force couple imbalances.[18]
It is recommended that to perform forward flexion/arm elevation with maximum elevation 3-5 times to reproduce dyskinesia. If the examiner isn't sure about the presence of dyskinesia a 3-5 pound weight is added in each hand and the subject is asked to perform 10 reps of arm elevation inflexion.[19][20] Scapular dyskinesia is more observable in the descent phase of arm motion, prominence of the medial border indicated a positive dyskinesis test.
2. Symptom altering tests[edit | edit source]
Scapular retraction test'.[21]This test evaluated the rotator cuff strength in scapular dyskinesia. Baseline AROM and pain are evaluated. This test is positive if the pain is reduced as the therapist assists active elevation by applying a posterior tilt and external rotation motion to the scapula. This application may be used in conjunction with other tests such as Neer's, Hawkin's-Kennedy, and Jobe's relocation.
Scapular assistance test'.[22] This test helps to evaluate scapular contributions to the existing shoulder pain based on alterations in motion. The baseline AROM and pain are evaluated. The therapist then applies an assist to scapular dynamics. This test is positive if ROM is increased or pain is reduced as the therapist manually assists scapular upward rotation during active UE elevation.
Lateral scapular Slide test (LSST) [23]: Measurements are taken from the spine of scapulae to T2/T3, Inferior angle of scapulae to T7/T9 and superior angle of scapulae to T2. The measurements are taken in 3 positions, (A) sitting/standing with arms resting on the side, (B) Hands on the waist, Thumbs Posteriorly (45 abduction), (C) 90 degrees abduction and maximal internal rotation. Measurement should not vary more than 1 to 1.5 cm, more the 1.5 cm difference is significant.
Isometric Scapular Pinch test: The patient in a standing position and is asked to actively squeeze or retract the scapulae together as hard as possible. Normal Response: An individual able to hold the squeeze for 15 to 20 sec without any burning pain or noticeable weakness. Positive: Burning pain present. Watch for: the patient relaxing the contraction.
Scapular Load test: As in position (2) for LSST, Manual load is applied in the anterior, posterior, inferior or superior direction to the arm, and the scapula should not move more than 1.5 cm.
Wall pushup test: The patient performs wall pushups 15 to 20 times. Weakness of scapular muscles (mainly serratus anterior) or winging usually shows up with 5 to 10 pushups. For stronger or younger populations, perform the test on the floor.
3. Assessment of surrounding structures[edit | edit source]
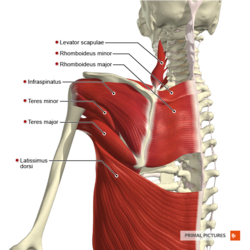
The structures around the scapula (thoracic spine, the acromioclavicular joint, rotator cuff muscles, two heads of the biceps and the glenoid labrum) are assessed. It is important to assess these structures thoroughly in order to exclude or confirm alternative causes of the symptoms. The assessor is looking for symptoms (pain, loss of function) in other structures, soft tissue laxity and muscle power. [24]
Manual muscle tests: For the middle and lower trapezius (manual resistance at 130-150degrees) and serratus anterior (manual resistance of the arm at 130degrees of flexion).
The infraspinatus strength test showed good reliability to assess infraspinatus weakness due to SD. [5]
Pectoralis minor muscle tightness: Current measures examine mm length at resting positions, not at maximal length. Unfortunately, there are no validated clinical measures to identify a patient as having a tight pectoralis minor muscle.
4. Static Measurements[edit | edit source]
Static measurements consist (1) infera: difference in vertical height of the superomedial scapular angle of the dropped scapula compared to contralateral angle. (2) Lateral displacement: difference of superomedial scapular angle from the midline (3) abduction: difference in angular degrees of medial scapular margin from plumb line.
5. Core Evaluation[edit | edit source]
The examiner stands behind the subject and asks the subject to contract the gluteal muscles while performing the low row test. The subject is asked to keep the shoulder extended and is asked to resist the anterior force offered by the therapist. If the strength of resistance the subject offers the therapist increases, it indicates that core and gluteal strengthening will aid scapular motion and strengthening of the core is hence indicated.[25]
6. Outcome Measures[edit | edit source]
Physiotherapy Management[edit | edit source]
Conservative treatment in SD cases aims to restore scapular retraction, posterior tilt, and ER.
Specific exercises for scapular rehabilitation include flexibility exercises to decrease scapular traction, and scapular stabilization exercises to optimize scapular kinematics. [5]
The traction on scapular posture can be reduced by performing exercises that increase muscle flexibility.[26] [27]Stretching exercises with shoulder horizontal abduction at 90◦ and 150◦ of elevation have been demonstrated to be useful in increasing pectoralis minor flexibility and the ER and posterior tilt of the scapula during forward elevation. [26][27][28]
Scapular stabilization exercises, based on stretching and strengthening, aim to improve muscle strength and joint position sense [29] [30] [31] The serratus anterior and trapezius muscles act as scapular stabilizers. The serratus anterior plays an essential role in determining scapular ER and posterior tilt, and the lower trapezius helps to stabilize the scapular position. Scapular stabilization exercises are based on closed and open kinetic chain exercises, including push-ups on a stable or unstable surface, lawnmower exercises and resisted scapular retraction.[29] [31]
Push-ups on a stable surface improve the serratus anterior stretch and, when Red Cord slings are used, general muscle strength improvements are obtained [32]; the same exercise, performed on an unstable surface, increases the activation of the trapezius, while decreasing the activation of the serratus anterior [33]. The upper and lower trapezius muscles can be better stimulated with upward rotation shrugs [34]. Specific shrug exercises may be beneficial to increase the upward rotation angle and the upper trapezius activity in subjects with SD and the corresponding scapular downward rotation syndrome [35].
In a review article [5] the effects of the Kinesio taping method have been evaluated. For type II SD, the placement of Kinesio taping over the upper and lower trapezius muscles may rebalance the scapular muscles, increasing the upward scapular rotation [36]; on the other hand, they do not induce changes in the electromyographic activity of serratus anterior, upper and lower trapezius muscles. No alteration in isometric force during shoulder flexo-abduction and external rotation has been shown [37].
Presentations[edit | edit source]
 |
Advanced Exercises for the Upper Quarter: A How To Guide for Scapular Motor Control Rehabilitation
This presentation, created by Stephanie Pascoe as part of the OMPT Fellowship in 2010, describes a how to guide for scapulothoracic rehabilitation. It includes some great animations! |
References[edit | edit source]
- ↑ Depreli Ö, Angın E. Review of scapular movement disorders among office workers having ergonomic risk. Journal of back and musculoskeletal rehabilitation. 2018 Jan 1;31(2):371-80.
- ↑ Longo UG, Petrillo S, Candela V, Rizzello G, Loppini M, Maffulli N, Denaro V. Arthroscopic rotator cuff repair with and without subacromial decompression is safe and effective: a clinical study. BMC Musculoskeletal Disorders. 2020 Dec;21:1-8.
- ↑ Saini SS, Shah SS, Curtis AS. Scapular dyskinesis and the kinetic chain: recognizing dysfunction and treating injury in the tennis athlete. Current Reviews in Musculoskeletal Medicine. 2020 Dec;13:748-56.
- ↑ Teixeira DC, Alves L, Gutierres M. The role of scapular dyskinesis on rotator cuff tears: a narrative review of the current knowledge. EFORT Open Reviews. 2021 Oct;6(10):932.
- ↑ 5.0 5.1 5.2 5.3 Giuseppe LU, Laura RA, Berton A, Candela V, Massaroni C, Carnevale A, Stelitano G, Schena E, Nazarian A, DeAngelis J, Denaro V. Scapular dyskinesis: from basic science to ultimate treatment. International journal of environmental research and public health. 2020 Apr;17(8):2974.
- ↑ Ludewig PM et al. Motion of the shoulder complex during multiplaner humeral elevation. J Bone Joint Surg. Am.2009;91:378-389.
- ↑ 7.0 7.1 McClure PW et al. Direct 3-dimentional measurement of scapular kinematics during dynamic movements in vivo.J Shoulder Elbow Surg.2001:10:269-277.
- ↑ Doody SG et al.Shoulder movements during abduction in the scapular plane.Arch Phys Med Rehab.1970:595-604.
- ↑ Bagg SD, Forrest Wj. A biomechanical analysis of scapular rotation during arm abduction in the scapular plane.Arch Phys Med Rehabil.1988:238-245.
- ↑ 10.0 10.1 Panagiotopoulos AC, Crowther IM. Scapular Dyskinesia, the forgotten culprit of shoulder pain and how to rehabilitate. SICOT-J. 2019;5.
- ↑ Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology Part I: pathoanatomy and biomechanics. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2003 Apr 1;19(4):404-20.
- ↑ 12.0 12.1 Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. British journal of sports medicine. 2010 Apr 1;44(5):300-5.
- ↑ Borstad JD. Resting position variables at the shoulder: evidence to support a posture-impairment association. Physical Therapy. 2006 Apr 1;86(4):549-57.
- ↑ Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clinical biomechanics. 2008 Feb 1;23(2):184-92.
- ↑ The disabled throwing shoulder: spectrum of pathology part III: the SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitationfckLRBurkhart, Stephen S et al.fckLRArthroscopy , Volume 19 , Issue 6 , 641 - 661
- ↑ Kuhn JE.Physical examination of the scapula -a systematic review.JOSPT.2009;39:A11.
- ↑ Uhl TL, Kibler WB, Gecewich B, Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy: the journal of arthroscopic & related surgery. 2009 Nov 1;25(11):1240-8.
- ↑ Inman VT et al.Observation on the function of the shoulder joint.J Bone Joint Surg.1944;26:1-30.
- ↑ McClure PW, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis: Part 1: Reliability. J Athl Train. 2009;44(2):160-164.
- ↑ Tate AR, McClure PW, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis: Part 2: Validity. J Athl Train. 2009;44(2):165-173.
- ↑ Tate AR et al. Effect of the scapular repositioning test on shoulder impingement symptoms and elevation strength in overhead athletes.JOSPT.2008;38:4-11.
- ↑ Rabin et al. The intertester reliability of the scapular assistance test.JOSPT.2006;36:653-660.
- ↑ Odom CJ, Taylor AB, Hurd CE, Denegar CR. Measurement of scapular asymmetry and assessment of shoulder dysfunction using the lateral scapular slide test: a reliability and validity study. Physical therapy. 2001 Feb 1;81(2):799-809.
- ↑ Kilber WB, Sciascia A (2010) Current concepts: scapular dyskinesis. British Journal of Sports Medicine. 44, 300–305. [CrossRef] [PubMed] [Google Scholar]
- ↑ Sciascia A, Kibler WB. Current Views of Scapular Dyskinesis and its Possible Clinical Relevance. International Journal of Sports Physical Therapy. 2022;17(2):117.
- ↑ 26.0 26.1 Umehara J, Nakamura M, Nishishita S, Tanaka H, Kusano K, Ichihashi N. Scapular kinematic alterations during arm elevation with decrease in pectoralis minor stiffness after stretching in healthy individuals. Journal of shoulder and elbow surgery. 2018 Jul 1;27(7):1214-20.
- ↑ 27.0 27.1 Umehara J, Nakamura M, Fujita K, Kusano K, Nishishita S, Araki K, Tanaka H, Yanase K, Ichihashi N. Shoulder horizontal abduction stretching effectively increases shear elastic modulus of pectoralis minor muscle. Journal of shoulder and elbow surgery. 2017 Jul 1;26(7):1159-65.
- ↑ Morais N, Cruz J. The pectoralis minor muscle and shoulder movement-related impairments and pain: Rationale, assessment and management. Physical Therapy in Sport. 2016 Jan 1;17:1-3.
- ↑ 29.0 29.1 Struyf F, Nijs J, Meeus M, Roussel NA, Mottram S, Truijen S, Meeusen R. Does scapular positioning predict shoulder pain in recreational overhead athletes?. International journal of sports medicine. 2013 Jul 3:75-82.
- ↑ Başkurt Z, Başkurt F, Gelecek N, Özkan MH. The effectiveness of scapular stabilization exercise in the patients with subacromial impingement syndrome. Journal of back and musculoskeletal rehabilitation. 2011 Jan 1;24(3):173-9.
- ↑ 31.0 31.1 Turgut E, Duzgun I, Baltaci G. Effects of scapular stabilization exercise training on scapular kinematics, disability, and pain in subacromial impingement: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2017 Oct 1;98(10):1915-23.
- ↑ De Mey, K.; Danneels, L.; Cagnie, B.; Borms, D.; T’Jonck, Z.; Van Damme, E.; Cools, A.M. Shoulder muscle activation levels during four closed kinetic chain exercises with and without Redcord slings. J. Strength Cond. Res. 2014, 28, 1626–1635. [CrossRef]
- ↑ Pirauá AL, Pitangui AC, Silva JP, dos Passos MH, de Oliveira VM, Batista LD, de Araújo RC. Electromyographic analysis of the serratus anterior and trapezius muscles during push-ups on stable and unstable bases in subjects with scapular dyskinesis. Journal of Electromyography and Kinesiology. 2014 Oct 1;24(5):675-81.
- ↑ Pizzari T, Wickham J, Balster S, Ganderton C, Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clinical biomechanics. 2014 Feb 1;29(2):201-5.
- ↑ Lee JH, Cynn HS, Choi WJ, Jeong HJ, Yoon TL. Various shrug exercises can change scapular kinematics and scapular rotator muscle activities in subjects with scapular downward rotation syndrome. Human movement science. 2016 Feb 1;45:119-29.
- ↑ Huang TS, Ou HL, Lin JJ. Effects of trapezius kinesio taping on scapular kinematics and associated muscular activation in subjects with scapular dyskinesis. Journal of Hand Therapy. 2019 Jul 1;32(3):345-52.
- ↑ Intelangelo L, Bordachar D, Barbosa AW. Effects of scapular taping in young adults with shoulder pain and scapular dyskinesis. Journal of Bodywork and Movement Therapies. 2016 Jul 1;20(3):525-32.