SLAP Lesion: Difference between revisions
mNo edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- Venugopal Pawar | '''Original Editor '''- [[User:Kristin Sartore|Kristin Sartore]], [[User: Venugopal Pawar|Venugopal Pawar]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | |||
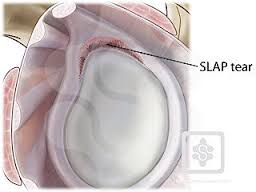
A SLAP tear or SLAP lesion is an injury to the glenoid labrum (fibrocartilaginous rim attached around the margin of the glenoid cavity). Tears of the superior labrum near to the origin of the long head of biceps were first described among throwing athletes by Andrews in 1985.<ref>ANDREWS JR et al., Glenoid labrum tears related to the long head of biceps. Am J Sports Med., 1985;13:337–341</ref>The label of ‘SLAP’, an abbreviation for superior labrum anterior and posterior, was coined by Snyder et al, who went on to create a classification system for these lesions.<ref>SNYDER SJ et al., SLAP lesions of the shoulder. Arthroscopy., 1990;6:274–279</ref><br> | |||
A total of four types of superior labral lesions involving the biceps anchor have been identified. Type I concerns degenerative fraying with no detachment of the biceps insertion. Type II is the most common type and represents a detachment of the superior labrum and biceps from the glenoid rim. Type III represents a bucket-handle tear of the labrum with an intact biceps tendon insertion to the bone. Finally, type IV lesions, the least common type represents an intra-substance tear of the biceps tendon with a bucket-handle tear of the superior aspect of the labrum.<ref name=":0">CHRISTOPHER C. et al., SLAP Lesions: An Update on Recognition and Treatment. J Orthop Sports Phys Ther, 2009; 39(2):71-80</ref> | |||
The Type II SLAP lesions have been further divided into three subtypes depending on whether the detachment of the labrum involves the anterior aspect of the labrum alone, the posterior aspect alone, or both aspects. The above classification system has been expanded to include an additional three types:<ref name=":0" /> | |||
*Type V: a [[Bankart lesion|Bankart lesion]] that extends superiorly to include a Type II SLAP lesion. | |||
*Type VI: an unstable flap tear of the labrum in conjunction with a biceps tendon separation. | |||
*Type VII: a superior labrum and biceps tendon separation that extends anteriorly, inferior to the middle glenohumeral ligament.<ref name=":0" /><br> | |||
Recently Nord and Ryu have added several previously unclassified lesions to the classification scheme. A Type VIII SLAP lesion is a SLAP extension along the posterior [[Glenoid Labrum|glenoid labrum]] as far as 6 o’clock. A Type IX lesion is a pan-labral SLAP injury extending the entire circumference of the glenoid. A Type X lesion is a superior labral tear associated with posterior-inferior labral tear (reverse bankart lesion ).<ref name=":1">POWELL S.E. et al., The Diagnosis, Classification, and Treatment of SLAP Lesions. Oper Tech Sports Med, 2012;20 (1):46 – 56</ref><br> | |||
[[Image:SLAP1.jpg]][[Image:SLAP2.jpg]] | |||
== Clinically Relevant Anatomy<br> == | == Clinically Relevant Anatomy<br> == | ||
A SLAP tear | The shoulder complex is one of the most sophisticated areas of the body. The shoulder is made up of five joints; the [[Acromioclavicular Joint|Acromioclavicular Joint]], the [[Sternoclavicular Joint|Sternoclavicular Joint]], the [[Glenohumeral Joint|Glenohumeral Joint]], [[Scapulothoracic Joint|Scapulothoracic Joint]] and Suprahumeral Joint and four linked bone groups; the clavicula, sternum, Scapula and the humerus which are related and work together.<ref name=":2">PEAT M., Functional anatomy of the schoulder complex. Phys Ther., 1986;66:1855-1865</ref><br>The major joint is the [[Glenohumeral Joint|Glenohumeral Joint]], which is also called the ‘ball in a socket’ joint because of the humeral head (ball) that articulates with the glenoid cavity (glenoid fossa of scapula or socket).<ref name=":2" />But the humeral head is larger than the fossa and so the socket covers only a quarter of the humeral head.<ref name=":3">CARMICHAEL S.W. et al., Anatomy of the Shoulder Joint. The Journal Of Orthopaedic And Sports Physical Therapy, 1985;6(4):225-228</ref><ref name=":2" /><br>A circumflexial rim of fibrocartilaginous tissue called labrum glenoidalis firmly attaches to the glenoid fossa thereby increasing the articular surface area and the stabilisation of the glenohumeral joint.<ref name=":2" /><ref name=":4">KOZIAK A. et al, Magnetic resonance arthrography assessment of the superior labrum using the BLC system: age-related changes mimicking SLAP-2 lesions. Skeletal Radiology, 2014;43: 1065 – 1070</ref> | ||
The long arm of the biceps inserts directly into the superior labrum, which also provides stabilisation to the superior part of the joint.<ref name=":1" /><ref name=":3" />In addition, the rotator_Cuff muscles are essential to ensure dynamic shoulder stability as they prevent excessive translations of the humeral head at the level of the glenoid fossa.<ref>MYERS J.B. et al., Sensorimotor deficits contributing to glenohumeral instability. Clin Orthop Relat Res,2002; 400:98–104</ref> | |||
Important variations in the normal anatomy of the labrum have been identified. Three distinct variations occur in over 10% of patients: | |||
# An isolated sublabral foramen, | |||
# A sublabral foramen with a cord-like middle glenohumeral ligament | |||
# A cordlike middle glenohumeral ligament without tissue at the anterosuperior labrum. The identification of these normal variants can help to prevent the misdiagnosis of labral lesions.<ref name=":1" /><br><br> | |||
[[Image:Labrum1.jpg]] | |||
== Epidemiology/Etiology == | |||
The age of the patient has an impact on the superior labrum. From the average age of 35, the superior labrum is less firmly attached to the glenoid than in people under the age of 30. In the age category 30 to 50, there are more chances of tears/defects in the superior and anterior-superior regions of the labrum (noted in cadavers). In the age category 60 years or older, circumferential lesions have been identified. Thus, we can conclude that there is an age-related effect in which the older the patient is, the more likely he will incur a SLAP lesion, due to age-related changes.<ref name=":4" /><br>In one study, half of the cases that had a SLAP lesion were 40 years old patients who showed signs and symptoms of instability after a history of acute trauma, repetitive injury, fall on an outstretched arm, or an injury from heavy lifting. Most of them had a type II SLAP lesion. They also noticed that the type II SLAP lesions in patients under 40 were associated with a bankart_lesion , other than a type II SLAP lesion in patients under 40 years old, whose SLAP lesion were associated with a tear of the supraspinatus tendon and osteoarthritis of the humeral head.<ref name=":1" /> | |||
There are a lot of different mechanisms of injury that can result in a SLAP lesion. The following causes have been found: <br> | |||
*repetitive throwing, | |||
*hyperextension, | |||
*a fall on an outstretched arm, | |||
*heavy lifting, | |||
*direct trauma. | |||
The two most common mechanisms are falling on an outstretched arm in which there is a superior compression, and a traction injury in the inferior direction.<ref name=":1" /> | |||
Falling on an outstretched arm is an acute traumatic superior compression force to the shoulder. In this situation the shoulder is abducted and slightly forward-flexed at the time of the impact. <br> | |||
A subsequent study found that the most common mechanism of injury was a fall or direct blow to the shoulder, occurring in 31% of patients. A significant number of patients with superior glenoid lesions and concomitant impingement or rotator cuff disease in the absence of trauma has also been identified. Indeed, Snyder et al found partial-thickness or full-thickness rotator cuff disease in 55 (40%) of 140 patients with SLAP lesions. Superior migration of the humeral head can result from a rotator cuff that is not effectively performing its role as a humeral head depressor. The superior labrum and biceps anchor could theoretically be gradually lifted off the glenoid as a result of chronic repetitive superior translation of the humeral head on the glenoid rim. Other authors supported the theory of an inferior traction mechanism on the basis of a sudden, traumatic, inferior pull on the arm or repetitive microtrauma from overhead sports activity with associated instability.<ref>HUIJBREGTS P.A., SLAP Lesions: Structure, Function, and Physical Therapy Diagnosis and Treatment. The Journal of Manual & Manipulative Therapy, 2001;9(2):71 – 83</ref><br> | |||
Throwers can have repetitive microtraumata. At the moment of the impact the glenohumeral contact point is shifted posterosuperiorly and increased shear forces are placed on the posterior-superior labrum, which results in a peel-back effect and eventually in a SLAP lesion.<ref name=":1" /><br> | |||
== Characteristics/Clinical Presentation == | |||
The most common complaint in patients that present with SLAP lesions is pain. Pain is typically intermittent and often associated with overhead movements.<ref name=":10">WILK K.E. et al, The recognition and treatment of superior labral (SLAP) lesions in the overhead athlete. Int. J. Sports Phys. Ther., 2013; 8(5): 579-600</ref>Isolated SLAP lesions are uncommon.<ref name=":11">HURI G. et al, Treatment of superior labrum anterior posterior lesions: a literature review. Acta Orthop Traumatol Turc., 2014;48(3): 290-297</ref>The majority of patients with SLAP lesions will also complain of:<br> | |||
*sensations of painful clicking and/or popping with shoulder movement<br> | |||
*loss of glenohumeral internal rotation range of motion<br> | |||
*pain with overhead motions<br> | |||
*loss of rotator cuff muscular strength and endurance<br> | |||
*loss of scapular stabiliser muscle strength and endurance<br> | |||
*inability to lie on the affected shoulder<ref name=":5">MANSKE R. et al., Superior labrum anterior to posterior (SLAP) rehabilitation in the overhead athlete. Phys Ther Sport., 2010;110-121</ref><br> | |||
Athletes performing overhead movements, especially pitchers, may develop “dead arm” syndrome in which they have a painful shoulder with throwing and can no longer throw with pre-injury velocity.<ref name=":6">KNESEK M. et al., Diagnosis and management of superior labral anterior posterior tears in throwing athlets. Am. J. Sports Med, 2013;41:444-460</ref>They may also report a loss of velocity and accuracy along with discomfort in the shoulder.<ref name=":5" /><br> | |||
== | It is important to keep in mind that the scapula is an important factor during shoulder movements. When the scapula does not perform its [[Scapulohumeral Rhythm|action properly]] there is a scapular malposition. This decreases the normal shoulder function.<ref name=":7">NURI A. et al., Superior labrum anterior to posterior lesionsof the shoulder: Diagnosis ans arthoscopic management. World J. Orthop., 2014; 5(3): 344-350</ref><ref name=":6" />It changes the activation of the scapular stabilising muscles. , which are the serratus anterior, rhomboid major and minor, levator scapulae and trapezius. The rotator-cuff muscles are important as well to anchor the scapula and guide the movement.<ref name=":7" /><ref>PAINE R. et al., The role of the scapula. Int. J. Sports. Phys. Ther., 2013;8(5):617-629</ref> <br> | ||
== Differential Diagnosis == | |||
The glenoid labrum is often involved in shoulder pathology. Sometimes morphological varieties can be confused with pathological aspects and therefore diagnosis should be established following careful analysis of the case history and a physical examination.<ref name=":8">CLAVERT P., Glenoid labrum pathology. Orthop Traumatol Surg Res., 2015;101(1):19-24</ref>There are two regions where anatomic variants can appear: the superior region, where it’s mostly related to age, and the anterosuperior region, where sometimes there is no labrum (12%) or a cord like ligament that is in continuity with the biceps footplate (13,5%).<ref name=":8" /> | |||
SLAP tear itself accounts for 80–90% of labral pathology in stable shoulder but it’s only found in 6% on arthroscopy. SLAP lesions are often seen in combination with other shoulder problems and this makes it difficult to diagnose.<ref>STETSON, W. (2010). SLAP Tear of the Shoulder. Retrieved from http://www.sportsmedicinedr.com/?page_id=715</ref>SLAP lesion is mostly combined with a lesion of the proximal head of the biceps because it attaches on the superior part of the labrum glenoidalis. It is associated with pain and instability and an inability of the patient to perform overhead movements.<ref name=":8" /> | |||
According to William F.B., SLAP lesions had an association of 43% with the medial sheath lesion. the author postulates that forces that affect the biceps anchor may also damage the pulley system of the bicipital sheath and, as such, this anatomic structure should be evaluated, especially when SLAP lesions are present.<ref>WILLIAM F.B., Correlation of the SLAP lesion with lesions of the medial sheath of the biceps tendon and intra-articular subscapularis tendon .Indian J Orthop. 2009 Oct-Dec; 43(4): 342–346</ref> | |||
Beside biceps tears, other problems, such as bursitis and rotator cuff tears, are often identified. In combination with SLAP lesions,<ref>WILK K.E. et al., Schoulder injuries in the overhead athlete. Journal of orthopaedic & sports physical therapy, 2009;39(2): 2009</ref><br>According to Morgan CD et al., Rotator cuff tears were present in 31% of patients whit SLAP lesion and were found to be lesion-location specific.<ref>MORGAN CD et al., Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears, Arthroscopy 1998 Sep;14(6):553-65</ref> | |||
Also suprascapular neuropathy secondary to cyst compression in the spinoglenoid notch may occur in association with SLAP tears.<ref>CHEN A.L. et al., Arthroscopic management of spinoglenoid cysts associated with SLAP lesions and suprascapular neuropathy. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 2003;19(6):15-21</ref> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
SLAP lesions are difficult to diagnose as they are very similar to those of instability and rotator cuff disorders. At first the clinician can test the tenderness to palpation at the rotator interval which can be helpful in the diagnostic procedure. The rotator interval is an anatomic space between the Supraspinatus tendon, the Subscapularis tendon and the processus coracoideus. This rotator interval has a triangular shape in which the supraspinatus is superiorly located, the subscapularis inferiorly and the processus coracoideus medially. It contains the coracohumeral and the superior glenohumeral ligament, the biceps tendon and the anterior joint capsule. If you know where these structures are situated, you can try to palpate the rotator interval.<ref>GASKILL T.R., The rotator interval: pathology and management, Journal of Arthroscopy and Related Surgery 2011, vol. 27, issue 4, p. 556-567</ref><br> | |||
This can be followed by these tests that are positive when there is a presence of a SLAP lesion: positive anterior drawer (53%), positive apprehension at 90° of abduction and maximal external rotation (86%), and positive relocation test (86%).<ref name=":1" /> | |||
In addition, several special tests can be used to help identify the presence of a SLAP lesion including the Clunk test, the crank test, O’ Briens, Anterior Slide test, Biceps Load I and II test, and the Active Compression test.<ref name=":1" /> | |||
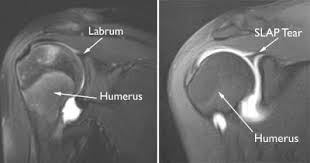
Another very important diagnostic element is the use of clear radiological and arthroscopic images of the labrum, which can help clinicians to distinguish the pathology from normal variation and make the correct diagnosis.<br>MRI is the most common imaging tool used to diagnose labral lesions, although it may not show a SLAP lesion. Therefore an MR arthrogram, where a contrast material gets injected into the shoulder, is also used. This is able to detect a SLAP tear better than a normal MRI scan.<ref>EK E. et al., Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tendonesis. Journal of Shoulder and Elbow surgery, 2014;23(7): 1059 – 1065</ref><br>Thus, MRA is more useful than conventional MRI and CT arthrography, and is a helpful technique in the diagnosis of SLAP tears. However, there is a great chance of false positive results due to a superior labral recess or sulcus, which is a normal variant, but can make the diagnosis more difficult.<ref>AMIN M. F. et al., The diagnostic value of magnetic resonance arthrography of the shoulder in detection and grading of SLAP lesions: Comparison with arthroscopic findings. European Journal of Radiology, 2012;81(3):2343 – 2347</ref> | |||
To describe the efficiency of MRA, several studies established the accuracy, specificity and sensitivity of MRA. Within every aspect the lowest and highest obtained numbers are described:<br>- Sensitivity (%): 82 – 95.6<br>- Specificity (%): 69 – 98<br>- Accuracy (%): 74 -90.19<ref>IQBAL H.J., Diagnostic value of MR Arthrogram in SLAP lesions of the shoulder, The Surgeon 2010, vol . 8, p. 303-309</ref><br><br> | |||
[[Image:Labrum MRI1.jpg]] | [[Image:Labrum MRI1.jpg]] | ||
== Outcome Measures == | |||
Rowe Score (version of 1988): | |||
*consists of 5 domains:<br> | |||
#pain<br> | |||
#stability<br> | |||
#function<br> | |||
#motion<br> | |||
#muscle strength<br> | |||
*Scoring:<br>< or = 49 = poor<br>50 - 69 =fair<br>70 - 84 = good<br>85 - 100 = excellent<ref name=":9">SKARE Ø. et al., Responsiveness of outcome measures in patients with superior labral anterior and posterior lesions. Shoulder & Elbow, 2014;6(4):262-272</ref><ref>JENSEN K.U. et al, Not all Rowe scores are the same! Which Rowe score do you use?, J Shoulder Elbow Surg., 2009;18(4):511-514</ref> | |||
Oxford Instability Shoulder Score (OISS): <br> | |||
*12-item questionnaire measuring:<br> | |||
#daily activities<br> | |||
#pain <br> | |||
*The total score ranges from 12 to 60 (12 indicates the best possible function)<ref name=":9" /><ref>DAWSON J. et al., The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br 1999; 81: 420–426</ref>. | |||
*A link to the questionnaire is added to the resources list below. | |||
Western Ontario Shoulder Instability Index (WOSI): <br> | |||
*21-item questionnaire with a visual analogue scale covering four domains: | |||
#physical symptoms (10 items)<br> | |||
#sports, recreation, and work (4 items)<br> | |||
#lifestyle (4 items)<br> | |||
#emotions (3 items)<br> | |||
*The responses for each question are given on a scale from 0 to 100 (0 equals the best possible score and 100 equals the worst).<ref name=":9" /><ref>KIRKLEY A.G. et al., The development and evaluation of a disease-specific quality of life measurements tool for shoulder instability. The western Ontario shoulder instability index (WOSI). Am J Sports Med., 1998;26:764-772</ref> | |||
*A link to the questionnaire is added to the resources list below.<br> | |||
EuroQol (EQ-5D and EQ-VAS):<br> | |||
*EQ-5D covers five domains: | |||
#mobility<br> | |||
#self-care<br> | |||
#usual activities<br> | |||
#pain/discomfort<br> | |||
#anxiety/depression<br> | |||
*EQ-VAS is a Visual Analogue Scale to measure the current health state, ranging from 0 (worst health state) to 100 (best health state).<ref name=":9" /> | |||
*A link to the questionnaire is added to the resources list below. | |||
According to Skare et al (2014) the OISS, WOSI and the Rowe score are responsive in the evaluation of patients with SLAP lesions. They also documented that the OISS and Rowe score appear to be the most sensitive measures.<ref name=":9" /> | |||
== Examination<br> == | |||
Clinical examination to detect SLAP lesions is an extremely challenging procedure because the condition is frequently associated with other shoulder pathologies in patients presenting this type of condition.<ref name=":10" /><ref name=":7" /> | |||
As with most shoulder conditions, the history including the exact mechanism of injury should be documented.<ref name=":10" /><ref name=":5" /><ref name=":7" />It is important to keep in mind that while labral pathologies are frequently caused by overuse, the patient may also describe a single traumatic event.<ref name=":10" />The physical examination is also very important in determining the correct diagnosis.<ref name=":5" /><br>Physical examination of the shoulder with this condition starts with a careful evaluation of glenohumeral and scapulothracic range of motion.<ref name=":12">MESERVE B.B. et al., A meta-analysis examining clinical test utility for assessing superior labral anterior posterior lesions. American journal of sports medicine,2009;37:2252-2258</ref>According to Nuri et al., 2014: “Another important part of the physical examination is evaluation of scapular kinematics. There might be scapular dyskinesis which is described as altered scapular position and motion relative to the thoracic cage.<ref name=":7" /> | |||
There are numerous physical examination procedures described to detect the SLAP lesion. Here are the most common listed<ref name=":7" />: <br>1. [[Biceps Load II Test|Biceps load test II]]<ref name=":10" /><ref name=":5" /><ref name=":7" /><br>2. [[O'Briens Test|O’Brien test]]<ref name=":10" /><ref name=":5" /><ref name=":7" /><br>3. [[Apprehension Test|Anterior apprehension test]]<ref name=":5" /><br>4. [[Speeds Test]]t<ref name=":5" /><ref name=":7" /><br>5. [[Yergasons Test|Yergason’s test]]<ref name=":5" /><ref name=":13">BOILEAU P. et al., Arthroscopic treatment of Isolated Type II SLAP lesions. Am J Sports Med., 2009;37:929–936</ref><br>6. Compression rotation test<ref name=":5" /><br> {{#ev:youtube|YV5hm6tuSvI|300}} Snyder (Snyder et al., 1990) described that the test should be performed with the patients' elbow in supine position.<ref name=":5" />In the video, the therapist does not supine the elbow, which can lead to a different diagnosis. <br> | |||
7. Dynamic labral shear test<ref name=":11" /><ref name=":7" /><br> {{#ev:youtube|Vo7YBDwZAbk}}<ref>Physiotutors. Dynamic Labral Shear Test | SLAP Lesion. Available from: https://www.youtube.com/watch?v=Vo7YBDwZAbk</ref> Sensitivity: 89%<br>Specificity: 30%<br> <ref name=":7" /><br><br> | |||
A combination of 2 sensitive tests and 1 specific test is more efficient to diagnose a SLAP lesion. <br>The therapist can choose the 2 sensitive tests out of the following 3:<br> | |||
*Compression rotation test | |||
*O’Brien test | |||
*Anterior apprehension test | |||
For the specific test, the therapist may choose out of the 3 following:<br> | |||
*Speed’s test | |||
*Yergason’s test | |||
*Biceps load test II<ref name=":5" /><ref>OH, J. H. et al., The evaluation of various physical examinations for the diagnosis of type II superior labrum anterior and posterior lesion. American Journal of Sports Medicine, 2008;36:353-359</ref> | |||
If one of the three tests is positive, this will result in a sensitivity of about 75%. But if all three tests are positive this will result in a specificity of about 90%.<ref name=":5" /> | |||
When we consider some tests individually, one can consider the Speed’s test and O’Brien’s test helpful in the diagnosis of anterior lesions and the [[Jobes Relocation Test]] is often positive in a posterior lesion<ref name=":1" /><ref>COOK C. et al., Diagnostic accuracy of five orthopedic clinical tests for diagnosis of superior labrum anterior posterior (SLAP) lesion. J Shoulder Elbow Surg., 2012;21(1):13 – 22</ref> | |||
According to Meserve et al. (2009), the O’Brien test is the most sensitive test (47%-78%) and the Speed’s test the most specific (67%-99%).<ref name=":5" /> | |||
The specificity is usually higher than sensitivity, thus the special tests are better at ruling out a SLAP lesion rather than to confirm the presence of a SLAP lesion.<ref>SANDREY M.A., Special physical examination tests for superior labrum anterior-posterior shoulder tears: an examinatioin of clinical usefulness. Journal of Athl. Train., 2013;48(6):856-858</ref>There are studies who combined few of the tests but the data differ too much therefore it’s difficult to make a general conclusion.<ref name=":5" /><ref name=":7" /><ref name=":12" /> | |||
= | There is a lot of discussion about which test is most accurate, but most experts consider that arthroscopy is the best way to diagnose SLAP lesion.<ref name=":11" /><br> | ||
{{#ev:youtube|FRotc9Rx1Ak}}<ref>Physiotutors. SLAP Lesion Cluster. Available from: https://www.youtube.com/watch?v=FRotc9Rx1Ak</ref> | |||
<br> | |||
== Management | == Medical Management<br> == | ||
The surgical intervention depends on the type of labral lesion, but an advanced arthroscopic technique is most commonly used. Studies of surgical labral repairs show that they are generally good to excellent to allow the patient to return to a pre-injury level of function. Knowing the type of SLAP lesion is important for post-operative rehabilitation.<ref name=":7" /> | |||
*Type I: are treated with debridement. Straightforward arthroscopic shaving, without damaging the biceps anchor, is enough for the surgical treatment of this type of lesion.<ref name=":7" /> | |||
*Type II: can be treated with arthroscopic fixation of the superior labrum to establish biceps anchor stability. | |||
The major studies suggested an extremely high level of success in arthroscopic repairs. According to Morgan et al, 97% of patients who underwent arthroscopic repair of type II SLAP had good, and even excellent results. But clinical results of elite throwing athletes has shown that this is in fact not always the case.<ref name=":7" />Detachment of the superior labrum from the glenoid is recognised as a problematic injury in throwing athletes and others who engage in repetitive overhead activities. Luckily for these athletes, Samani JE et al., concluded that using an absorbable tack to repair type II SLAP lesions is an effective treatment, even in athletes with high demands and expectations for shoulder function.<ref>SAMANI J.E. et al., Arthroscopic stabilization of type II SLAP lesions using an absorbable tack. Arthroscopy., 2001;17:19–24</ref> | |||
= | For patients older than 36 years there is a higher chance of failure.<ref>PROVENCHER M.T. et al., A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med., 2013;41:880–886</ref>Because of unsatisfactory results in older patients, Boileau et al., suggested arthroscopic biceps tenodesis in these patients. They found that tenodesis is superior to the repair of type II SLAP tears in older population. Arthroscopic biceps tenodesis can be considered as an effective alternative to the repair of a type II SLAP lesion, allowing patients to return to a pre-surgical level of activity and sports participation. The results of biceps reinsertion are disappointing compared with biceps tenodesis. Furthermore, biceps tenodesis may provide a viable alternative for the salvage of a failed SLAP repair.<ref name=":13" /><br>However in another study by Alpert et al., it is shown that type II SLAP repairs using suture anchors can yield good to excellent results in patients older and younger than age 40. Their findings show no difference between the two age groups. So there are conflicting views in the literature about the repairs in the older patients.<ref>ALPERT J.M. et al., The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med., 2010;38:2299–2303</ref> | ||
*Type III: can easily be debrided by an arthroscopic shaver. There is no need to repair this type of injury. After the resection of the free fragment, a pain free shoulder can be established.<ref>HIGGINS L.D. et al., Superior labral lesions: anatomy, pathology, and treatment. Clin Orthop Relat Res., 2001;390:73–82</ref> | |||
*Type IV: can be repaired with multiple sutures. | |||
Field and Savoie reported 100% good results at an average follow-up of 21 months. Also Pagnani et al., reported that superior glenoid lesions with unstable biceps anchors (type IV lesions), which were stabilised with absorbable tacks obtained good results. At their 2-year follow-up, 86% of the patients had satisfactory results, and no complications were related to use of the tack. Stetson et al., presented the long-term results of 140 SLAP lesions with follow-up available on 130 patients at an average of 3.2 years. Type IV lesions in 17 patients (13%) were debrided.<ref>D’ALESSANDRO D.F. et al., Superior Labral Lesions: Diagnosis and Management. J Athl Train., 2000;35(3):286–292</ref> | |||
SLAP | <br>SLAP lesions are repaired by the use of portals. There are different portals: a posterior portal, a anteroinferior portal and a mid-glenoid portal. Similarly, O'Brien described the creation of a trans-rotator cuff portal for repair when the lesion is posterior to the biceps tendon, and Burkhart has advocated the use of a posterolateral portal (Port of Wilmington) as part of a SLAP repair. More recently, Nord et al. described the use of the Neviaser portal, a superior medial portal, as the working portal in SLAP repairs. There is no specific portal used for each type a SLAP lesion. The use of a certain portal is determined by a combination of location and the surgeon’s preference.<ref>XINNING L. et al., Management of type II superior labrum anterior posterior lesions: a review of the literature. 2010;6:16-22</ref><br><br> | ||
{{#ev:youtube|75ARVxXIRBE}} | |||
== Physical Therapy Management == | |||
Until now only one study looked at results from physical management on SLAP lesion. The study was a one year follow- up study of with 19 patients. It compared good shoulder function with the shoulder function of patient that followed successful conservative management in the form of scapular stabilization exercises and posterior capsular stretching. However the study acknowledges that more than half of the treatment of patients who were initially prescribed non operative management failed and these patients went on to undergo arthroscopic surgery.<ref name=":14">EDWARDS S.L. et al., Non operative treatment of superior labrum anterior posterior tears - improvements in pain function and quality of life. Am J Sports Med., 2010;38:1456–1461</ref> It is generally recognized that the majority of patients with symptomatic SLAP lesions will fail conservative management, particularly throwers.<ref name=":0" />Given that conservative management only seems to be successful in a few patients, mainly in type I SLAP lesions, it is only implemented in patients with this type of lesion or patients who do not wish to undergo surgery.<ref name=":0" /><br>In the first step of conservative management, patients should abstain from aggravating activities in order to provide relief to the pain and inflammation. If necessary, NSAID’s and intra-articular corticosteroid injections can be applied to help diminish complaints.<ref name=":0" /><ref name=":14" />This way, physical treatment can be started sooner. Strength, stability and motion are the components of shoulder function that should be focused on during rehabilitation.<ref>SACCOL M.F. et al., Shoulder rotator strength and torque steadiness in athletes with anterior shoulder instability or SLAP lesion. Journal of Science and Medicine in Sport, 2014;17(5): 463–468</ref>This course of treatment should focus on restoring strength of the rotator cuff, shoulder girdle, trunk, core and scapular musculature, restoring normal shoulder motion, and training to improve dynamic joint stability.<ref name=":0" /><br>Regaining GIRD is a crucial aspect in the rehabilitation of SLAP lesions.<ref name=":0" />By the use of posterior capsule stretching exercises, such as sleeper stretch and cross body adduction stretches, and exercises for scapula stabilisation, redevelopment of the internal rotation can be accomplished.<ref name=":14" /><ref name=":15">MAENHOUT A. et al., Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med., 2012;40(9):2105-2112</ref><br>By stretching the posterior capsule and restoring internal rotation, through posterior capsule stretching exercises, such as sleeper stretch and cross body adduction stretches, and exercises for scapula stabilisation , pathologic contact between the supraspinatus tendon and the posterosuperior labrum.<ref name=":14" /><ref name=":15" />can be prevented. The patient is eventually advanced to a strengthening phase, which includes trunk, core, rotator cuff, and scapular musculature. In throwing athletes, a progressive throwing program that is directed toward the patients' specific sport and position can be initiated after 3 months.<ref name=":0" /><br> | |||
Sixteen commonly used shoulder rehabilitation exercises can be chosen on the basis of several EMG studies and clinical recommendations regarding the rehabilitation of patients with SLAP lesions. <br>These exercises are:<br> | |||
*forward flexion in a side-lying position | |||
*prone extension | |||
*seated rowing | |||
*serratus punch (protraction with the elbow extended)<br> | |||
{{#ev:youtube|zxeEF2eMBRg|300}} | |||
*knee push-up plus<br> | |||
{{#ev:youtube|xzHVLqqUQRE|300}} | |||
*forward flexion in external rotation and forearm supination<br> | |||
*full can (elevation in the scapular plane in external rotation)<br> | |||
{{#ev:youtube|Tm6ASdJxWOY|300}} | |||
*internal rotation in 20° of abduction<br> | |||
*external rotation in 20° of abduction | |||
*internal rotation in 90° of abduction | |||
*external rotation in 90° of abduction | |||
*forearm supination, elbow flexion in forearm supination | |||
*uppercut (combined forward flexion of the shoulder and flexion and supination of the elbow) | |||
*internal rotation diagonal | |||
*external rotation diagonal | |||
These exercises, with increasing low to moderate activity, can be applied in the early and intermediate phases of nonoperative and postoperative treatment for patients with proximal biceps tendon disorders and SLAP lesions.<ref>COOLS A .M. et al., Rehabilitation Exercises for Athletes With Biceps Disorders and SLAP Lesions: A Continuum of Exercises With Increasing Loads on the Biceps. Am J Sports Med.,2014 ;42(6):1315-1322</ref> | |||
When conservative treatment fails, a surgical approach is in order.<ref name=":0" /> | |||
After surgery, for 3 to 4 weeks, the shoulder of the patient is placed in a sling, which immobilises the shoulder in internal rotation and leads to general loss of motion and stiffness.<ref name=":0" /><ref name=":11" />Postoperative rehabilitation is determined by the type of SLAP lesion, the chosen surgical procedure and other concomitant pathologies and procedures performed.<ref name=":0" /><br>Generally pendulum and elbow range-of-motion exercises are allowed during the period of immobilization. External rotation must absolutely be avoided and abduction limited to 60°. Assisted and passive techniques are used at 4 weeks post-operative to increase shoulder mobility. Between week 4 and 8, internal and external rotation ROM are progressively increased to 90° of shoulder abduction. Resistance exercises can be initiated at approximately 8 weeks post-operative, in which scapular strengthening should be emphasized. Since the metabolism of cartilage depends partly on its mechanical environment, resistance training can contribute to gaining mobility. However, the achievement of adequate shoulder mobility is an important condition to begin resistance training. At month 4 to 6, dependent on the type of sport practiced, patients should be able to start sport-specific training and gradually return to their former level of activity.<ref name=":0" /><br>SLAP lesion repair often fails, and biceps tenodesis or tenotomy seems to be an acceptable alternative treatment for SLAP lesions. Furthermore, this technique has now become the most preferable treatment for failed SLAP repairs.<ref>WEBER S.C., Surgical management of the failed SLAP repair. Sports Med Arthrosc.,2010;18:162-166</ref>The indications for biceps tenodesis as the index procedure for a symptomatic SLAP lesion depends on: <br> | |||
*the patient’s age | |||
*activity level | |||
*arm dominance | |||
*type of sport.<ref name=":11" /> | |||
If a biceps tenodesis is performed a minimum of 10 weeks is recommended without biceps activity to allow the repaired soft tissue to fully incorporate into the bone tunnels.<ref name=":5" /><br><br><br> | |||
== Key Evidence == | |||
== Resources <br> == | == Resources <br> == | ||
* Dutton Mark. Orthopaedic examination, evaluation, and intervention. New York: McGraw Hill; 2004. | |||
* Dessaur WA. (2008). Diagnostic Accuracy of Clinical Testing for Superior Labral Anterior Posterior Lesions: A Systematic Review Journal of Orthopaedic and Sports | |||
* Robert Manske, Daniel Prohaska. Superior labrum anterior to posterior (SLAP) rehabilitation in the overhead athlete. Physical Therapy in Sport 11, 2010, p.110-121.(Table 4). '''Rehablitation following arthroscopic type II SLAP repair.'''<br><u>Note</u>: Strength training first weeks: 13 repetitions - 4 sequences – 1 to 3 minutes of rest between sequences<br> Strength training, build up to: 20 repetitions – 3 sequences – 1 minute of rest between sequences<br> Stretching: Total stretching time = 30 seconds for each stretch → 3x10” – 2x15” – 1x30” (build up) <br>30 to 60 seconds of rest between each stretch | |||
*http://www.ouh.nhs.uk/shoulderandelbow/information/documents/OSI_Score13.pdf | |||
*http://www.orthopaedicscore.com/scorepages/oxford_wosi_score.html | |||
*http://www.wirral.nhs.uk/document_uploads/Commissioning/Appendix3-EQ5D3L.pdf | |||
*http://www.euroqol.org/ | |||
*http://www.rheumatologynetwork.com/articles/taking-closer-look-rotator-cuff-disorders/page/0/2<br> | |||
== | == Clinical bottom line<br> == | ||
SLAP lesions are lesions of the superior labrum in which there are several types described. A SLAP lesion is mainly caused by a fall on an outstretched arm where there is an important superior compression on the labrum which causes a tear of the labrum. A typical symptom is intermittent pain that also occurs in overhead movements. To diagnose this condition it is important to use several different tests and not only one. Physical examination is not easy because of the fact that SLAP lesions are often associated with other shoulder pathologies. For the physical examination the therapist uses the tests described in ‘Diagnostic Procedures’, but apart from that he can also test the glenohumeral and scapulothracic range of motion because there could occur a dyskinesis caused by the SLAP lesion. For the treatment of SLAP lesion one uses often a medical treatment where the surgeon uses advanced arthroscopic techniques. But a physical treatment is also possible. This includes stretching, strengthening, and stabilisation exercises.<br>It is important to note that every treatment depends on the type of the SLAP lesion and that conservative treatment may fail and is not suited to every patient.<br><br> | |||
== Case Studies == | |||
== Recent Related Research == | |||
<div class="researchbox"> | <div class="researchbox"> | ||
<rss>http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1nESb63TAKHoQUHW0i5DZbXKJYglsJko7_TQHWRNxhFvxXKA0</rss> | |||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:EIM_Residency_Project]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Shoulder]] [[Category:Shoulder_Conditions]] [[Category:Sports_Injuries]] | |||
Revision as of 22:05, 3 February 2018
Original Editor - Kristin Sartore, Venugopal Pawar
Top Contributors - Venugopal Pawar, Lucinda hampton, Fasuba Ayobami, Rachael Lowe, Kim Jackson, Admin, WikiSysop, Claire Knott, Amrita Patro, Wanda van Niekerk and Vasileios Tyros
Definition/Description[edit | edit source]
A SLAP tear or SLAP lesion is an injury to the glenoid labrum (fibrocartilaginous rim attached around the margin of the glenoid cavity). Tears of the superior labrum near to the origin of the long head of biceps were first described among throwing athletes by Andrews in 1985.[1]The label of ‘SLAP’, an abbreviation for superior labrum anterior and posterior, was coined by Snyder et al, who went on to create a classification system for these lesions.[2]
A total of four types of superior labral lesions involving the biceps anchor have been identified. Type I concerns degenerative fraying with no detachment of the biceps insertion. Type II is the most common type and represents a detachment of the superior labrum and biceps from the glenoid rim. Type III represents a bucket-handle tear of the labrum with an intact biceps tendon insertion to the bone. Finally, type IV lesions, the least common type represents an intra-substance tear of the biceps tendon with a bucket-handle tear of the superior aspect of the labrum.[3]
The Type II SLAP lesions have been further divided into three subtypes depending on whether the detachment of the labrum involves the anterior aspect of the labrum alone, the posterior aspect alone, or both aspects. The above classification system has been expanded to include an additional three types:[3]
- Type V: a Bankart lesion that extends superiorly to include a Type II SLAP lesion.
- Type VI: an unstable flap tear of the labrum in conjunction with a biceps tendon separation.
- Type VII: a superior labrum and biceps tendon separation that extends anteriorly, inferior to the middle glenohumeral ligament.[3]
Recently Nord and Ryu have added several previously unclassified lesions to the classification scheme. A Type VIII SLAP lesion is a SLAP extension along the posterior glenoid labrum as far as 6 o’clock. A Type IX lesion is a pan-labral SLAP injury extending the entire circumference of the glenoid. A Type X lesion is a superior labral tear associated with posterior-inferior labral tear (reverse bankart lesion ).[4]

Clinically Relevant Anatomy
[edit | edit source]
The shoulder complex is one of the most sophisticated areas of the body. The shoulder is made up of five joints; the Acromioclavicular Joint, the Sternoclavicular Joint, the Glenohumeral Joint, Scapulothoracic Joint and Suprahumeral Joint and four linked bone groups; the clavicula, sternum, Scapula and the humerus which are related and work together.[5]
The major joint is the Glenohumeral Joint, which is also called the ‘ball in a socket’ joint because of the humeral head (ball) that articulates with the glenoid cavity (glenoid fossa of scapula or socket).[5]But the humeral head is larger than the fossa and so the socket covers only a quarter of the humeral head.[6][5]
A circumflexial rim of fibrocartilaginous tissue called labrum glenoidalis firmly attaches to the glenoid fossa thereby increasing the articular surface area and the stabilisation of the glenohumeral joint.[5][7]
The long arm of the biceps inserts directly into the superior labrum, which also provides stabilisation to the superior part of the joint.[4][6]In addition, the rotator_Cuff muscles are essential to ensure dynamic shoulder stability as they prevent excessive translations of the humeral head at the level of the glenoid fossa.[8]
Important variations in the normal anatomy of the labrum have been identified. Three distinct variations occur in over 10% of patients:
- An isolated sublabral foramen,
- A sublabral foramen with a cord-like middle glenohumeral ligament
- A cordlike middle glenohumeral ligament without tissue at the anterosuperior labrum. The identification of these normal variants can help to prevent the misdiagnosis of labral lesions.[4]
Epidemiology/Etiology[edit | edit source]
The age of the patient has an impact on the superior labrum. From the average age of 35, the superior labrum is less firmly attached to the glenoid than in people under the age of 30. In the age category 30 to 50, there are more chances of tears/defects in the superior and anterior-superior regions of the labrum (noted in cadavers). In the age category 60 years or older, circumferential lesions have been identified. Thus, we can conclude that there is an age-related effect in which the older the patient is, the more likely he will incur a SLAP lesion, due to age-related changes.[7]
In one study, half of the cases that had a SLAP lesion were 40 years old patients who showed signs and symptoms of instability after a history of acute trauma, repetitive injury, fall on an outstretched arm, or an injury from heavy lifting. Most of them had a type II SLAP lesion. They also noticed that the type II SLAP lesions in patients under 40 were associated with a bankart_lesion , other than a type II SLAP lesion in patients under 40 years old, whose SLAP lesion were associated with a tear of the supraspinatus tendon and osteoarthritis of the humeral head.[4]
There are a lot of different mechanisms of injury that can result in a SLAP lesion. The following causes have been found:
- repetitive throwing,
- hyperextension,
- a fall on an outstretched arm,
- heavy lifting,
- direct trauma.
The two most common mechanisms are falling on an outstretched arm in which there is a superior compression, and a traction injury in the inferior direction.[4]
Falling on an outstretched arm is an acute traumatic superior compression force to the shoulder. In this situation the shoulder is abducted and slightly forward-flexed at the time of the impact.
A subsequent study found that the most common mechanism of injury was a fall or direct blow to the shoulder, occurring in 31% of patients. A significant number of patients with superior glenoid lesions and concomitant impingement or rotator cuff disease in the absence of trauma has also been identified. Indeed, Snyder et al found partial-thickness or full-thickness rotator cuff disease in 55 (40%) of 140 patients with SLAP lesions. Superior migration of the humeral head can result from a rotator cuff that is not effectively performing its role as a humeral head depressor. The superior labrum and biceps anchor could theoretically be gradually lifted off the glenoid as a result of chronic repetitive superior translation of the humeral head on the glenoid rim. Other authors supported the theory of an inferior traction mechanism on the basis of a sudden, traumatic, inferior pull on the arm or repetitive microtrauma from overhead sports activity with associated instability.[9]
Throwers can have repetitive microtraumata. At the moment of the impact the glenohumeral contact point is shifted posterosuperiorly and increased shear forces are placed on the posterior-superior labrum, which results in a peel-back effect and eventually in a SLAP lesion.[4]
Characteristics/Clinical Presentation[edit | edit source]
The most common complaint in patients that present with SLAP lesions is pain. Pain is typically intermittent and often associated with overhead movements.[10]Isolated SLAP lesions are uncommon.[11]The majority of patients with SLAP lesions will also complain of:
- sensations of painful clicking and/or popping with shoulder movement
- loss of glenohumeral internal rotation range of motion
- pain with overhead motions
- loss of rotator cuff muscular strength and endurance
- loss of scapular stabiliser muscle strength and endurance
- inability to lie on the affected shoulder[12]
Athletes performing overhead movements, especially pitchers, may develop “dead arm” syndrome in which they have a painful shoulder with throwing and can no longer throw with pre-injury velocity.[13]They may also report a loss of velocity and accuracy along with discomfort in the shoulder.[12]
It is important to keep in mind that the scapula is an important factor during shoulder movements. When the scapula does not perform its action properly there is a scapular malposition. This decreases the normal shoulder function.[14][13]It changes the activation of the scapular stabilising muscles. , which are the serratus anterior, rhomboid major and minor, levator scapulae and trapezius. The rotator-cuff muscles are important as well to anchor the scapula and guide the movement.[14][15]
Differential Diagnosis[edit | edit source]
The glenoid labrum is often involved in shoulder pathology. Sometimes morphological varieties can be confused with pathological aspects and therefore diagnosis should be established following careful analysis of the case history and a physical examination.[16]There are two regions where anatomic variants can appear: the superior region, where it’s mostly related to age, and the anterosuperior region, where sometimes there is no labrum (12%) or a cord like ligament that is in continuity with the biceps footplate (13,5%).[16]
SLAP tear itself accounts for 80–90% of labral pathology in stable shoulder but it’s only found in 6% on arthroscopy. SLAP lesions are often seen in combination with other shoulder problems and this makes it difficult to diagnose.[17]SLAP lesion is mostly combined with a lesion of the proximal head of the biceps because it attaches on the superior part of the labrum glenoidalis. It is associated with pain and instability and an inability of the patient to perform overhead movements.[16]
According to William F.B., SLAP lesions had an association of 43% with the medial sheath lesion. the author postulates that forces that affect the biceps anchor may also damage the pulley system of the bicipital sheath and, as such, this anatomic structure should be evaluated, especially when SLAP lesions are present.[18]
Beside biceps tears, other problems, such as bursitis and rotator cuff tears, are often identified. In combination with SLAP lesions,[19]
According to Morgan CD et al., Rotator cuff tears were present in 31% of patients whit SLAP lesion and were found to be lesion-location specific.[20]
Also suprascapular neuropathy secondary to cyst compression in the spinoglenoid notch may occur in association with SLAP tears.[21]
Diagnostic Procedures[edit | edit source]
SLAP lesions are difficult to diagnose as they are very similar to those of instability and rotator cuff disorders. At first the clinician can test the tenderness to palpation at the rotator interval which can be helpful in the diagnostic procedure. The rotator interval is an anatomic space between the Supraspinatus tendon, the Subscapularis tendon and the processus coracoideus. This rotator interval has a triangular shape in which the supraspinatus is superiorly located, the subscapularis inferiorly and the processus coracoideus medially. It contains the coracohumeral and the superior glenohumeral ligament, the biceps tendon and the anterior joint capsule. If you know where these structures are situated, you can try to palpate the rotator interval.[22]
This can be followed by these tests that are positive when there is a presence of a SLAP lesion: positive anterior drawer (53%), positive apprehension at 90° of abduction and maximal external rotation (86%), and positive relocation test (86%).[4]
In addition, several special tests can be used to help identify the presence of a SLAP lesion including the Clunk test, the crank test, O’ Briens, Anterior Slide test, Biceps Load I and II test, and the Active Compression test.[4]
Another very important diagnostic element is the use of clear radiological and arthroscopic images of the labrum, which can help clinicians to distinguish the pathology from normal variation and make the correct diagnosis.
MRI is the most common imaging tool used to diagnose labral lesions, although it may not show a SLAP lesion. Therefore an MR arthrogram, where a contrast material gets injected into the shoulder, is also used. This is able to detect a SLAP tear better than a normal MRI scan.[23]
Thus, MRA is more useful than conventional MRI and CT arthrography, and is a helpful technique in the diagnosis of SLAP tears. However, there is a great chance of false positive results due to a superior labral recess or sulcus, which is a normal variant, but can make the diagnosis more difficult.[24]
To describe the efficiency of MRA, several studies established the accuracy, specificity and sensitivity of MRA. Within every aspect the lowest and highest obtained numbers are described:
- Sensitivity (%): 82 – 95.6
- Specificity (%): 69 – 98
- Accuracy (%): 74 -90.19[25]
Outcome Measures[edit | edit source]
Rowe Score (version of 1988):
- consists of 5 domains:
- pain
- stability
- function
- motion
- muscle strength
Oxford Instability Shoulder Score (OISS):
- 12-item questionnaire measuring:
- daily activities
- pain
- The total score ranges from 12 to 60 (12 indicates the best possible function)[26][28].
- A link to the questionnaire is added to the resources list below.
Western Ontario Shoulder Instability Index (WOSI):
- 21-item questionnaire with a visual analogue scale covering four domains:
- physical symptoms (10 items)
- sports, recreation, and work (4 items)
- lifestyle (4 items)
- emotions (3 items)
- The responses for each question are given on a scale from 0 to 100 (0 equals the best possible score and 100 equals the worst).[26][29]
- A link to the questionnaire is added to the resources list below.
EuroQol (EQ-5D and EQ-VAS):
- EQ-5D covers five domains:
- mobility
- self-care
- usual activities
- pain/discomfort
- anxiety/depression
- EQ-VAS is a Visual Analogue Scale to measure the current health state, ranging from 0 (worst health state) to 100 (best health state).[26]
- A link to the questionnaire is added to the resources list below.
According to Skare et al (2014) the OISS, WOSI and the Rowe score are responsive in the evaluation of patients with SLAP lesions. They also documented that the OISS and Rowe score appear to be the most sensitive measures.[26]
Examination
[edit | edit source]
Clinical examination to detect SLAP lesions is an extremely challenging procedure because the condition is frequently associated with other shoulder pathologies in patients presenting this type of condition.[10][14]
As with most shoulder conditions, the history including the exact mechanism of injury should be documented.[10][12][14]It is important to keep in mind that while labral pathologies are frequently caused by overuse, the patient may also describe a single traumatic event.[10]The physical examination is also very important in determining the correct diagnosis.[12]
Physical examination of the shoulder with this condition starts with a careful evaluation of glenohumeral and scapulothracic range of motion.[30]According to Nuri et al., 2014: “Another important part of the physical examination is evaluation of scapular kinematics. There might be scapular dyskinesis which is described as altered scapular position and motion relative to the thoracic cage.[14]
There are numerous physical examination procedures described to detect the SLAP lesion. Here are the most common listed[14]:
1. Biceps load test II[10][12][14]
2. O’Brien test[10][12][14]
3. Anterior apprehension test[12]
4. Speeds Testt[12][14]
5. Yergason’s test[12][31]
6. Compression rotation test[12]
Snyder (Snyder et al., 1990) described that the test should be performed with the patients' elbow in supine position.[12]In the video, the therapist does not supine the elbow, which can lead to a different diagnosis.
7. Dynamic labral shear test[11][14]
[32] Sensitivity: 89%
Specificity: 30%
[14]
A combination of 2 sensitive tests and 1 specific test is more efficient to diagnose a SLAP lesion.
The therapist can choose the 2 sensitive tests out of the following 3:
- Compression rotation test
- O’Brien test
- Anterior apprehension test
For the specific test, the therapist may choose out of the 3 following:
If one of the three tests is positive, this will result in a sensitivity of about 75%. But if all three tests are positive this will result in a specificity of about 90%.[12]
When we consider some tests individually, one can consider the Speed’s test and O’Brien’s test helpful in the diagnosis of anterior lesions and the Jobes Relocation Test is often positive in a posterior lesion[4][34]
According to Meserve et al. (2009), the O’Brien test is the most sensitive test (47%-78%) and the Speed’s test the most specific (67%-99%).[12]
The specificity is usually higher than sensitivity, thus the special tests are better at ruling out a SLAP lesion rather than to confirm the presence of a SLAP lesion.[35]There are studies who combined few of the tests but the data differ too much therefore it’s difficult to make a general conclusion.[12][14][30]
There is a lot of discussion about which test is most accurate, but most experts consider that arthroscopy is the best way to diagnose SLAP lesion.[11]
Medical Management
[edit | edit source]
The surgical intervention depends on the type of labral lesion, but an advanced arthroscopic technique is most commonly used. Studies of surgical labral repairs show that they are generally good to excellent to allow the patient to return to a pre-injury level of function. Knowing the type of SLAP lesion is important for post-operative rehabilitation.[14]
- Type I: are treated with debridement. Straightforward arthroscopic shaving, without damaging the biceps anchor, is enough for the surgical treatment of this type of lesion.[14]
- Type II: can be treated with arthroscopic fixation of the superior labrum to establish biceps anchor stability.
The major studies suggested an extremely high level of success in arthroscopic repairs. According to Morgan et al, 97% of patients who underwent arthroscopic repair of type II SLAP had good, and even excellent results. But clinical results of elite throwing athletes has shown that this is in fact not always the case.[14]Detachment of the superior labrum from the glenoid is recognised as a problematic injury in throwing athletes and others who engage in repetitive overhead activities. Luckily for these athletes, Samani JE et al., concluded that using an absorbable tack to repair type II SLAP lesions is an effective treatment, even in athletes with high demands and expectations for shoulder function.[37]
For patients older than 36 years there is a higher chance of failure.[38]Because of unsatisfactory results in older patients, Boileau et al., suggested arthroscopic biceps tenodesis in these patients. They found that tenodesis is superior to the repair of type II SLAP tears in older population. Arthroscopic biceps tenodesis can be considered as an effective alternative to the repair of a type II SLAP lesion, allowing patients to return to a pre-surgical level of activity and sports participation. The results of biceps reinsertion are disappointing compared with biceps tenodesis. Furthermore, biceps tenodesis may provide a viable alternative for the salvage of a failed SLAP repair.[31]
However in another study by Alpert et al., it is shown that type II SLAP repairs using suture anchors can yield good to excellent results in patients older and younger than age 40. Their findings show no difference between the two age groups. So there are conflicting views in the literature about the repairs in the older patients.[39]
- Type III: can easily be debrided by an arthroscopic shaver. There is no need to repair this type of injury. After the resection of the free fragment, a pain free shoulder can be established.[40]
- Type IV: can be repaired with multiple sutures.
Field and Savoie reported 100% good results at an average follow-up of 21 months. Also Pagnani et al., reported that superior glenoid lesions with unstable biceps anchors (type IV lesions), which were stabilised with absorbable tacks obtained good results. At their 2-year follow-up, 86% of the patients had satisfactory results, and no complications were related to use of the tack. Stetson et al., presented the long-term results of 140 SLAP lesions with follow-up available on 130 patients at an average of 3.2 years. Type IV lesions in 17 patients (13%) were debrided.[41]
SLAP lesions are repaired by the use of portals. There are different portals: a posterior portal, a anteroinferior portal and a mid-glenoid portal. Similarly, O'Brien described the creation of a trans-rotator cuff portal for repair when the lesion is posterior to the biceps tendon, and Burkhart has advocated the use of a posterolateral portal (Port of Wilmington) as part of a SLAP repair. More recently, Nord et al. described the use of the Neviaser portal, a superior medial portal, as the working portal in SLAP repairs. There is no specific portal used for each type a SLAP lesion. The use of a certain portal is determined by a combination of location and the surgeon’s preference.[42]
Physical Therapy Management[edit | edit source]
Until now only one study looked at results from physical management on SLAP lesion. The study was a one year follow- up study of with 19 patients. It compared good shoulder function with the shoulder function of patient that followed successful conservative management in the form of scapular stabilization exercises and posterior capsular stretching. However the study acknowledges that more than half of the treatment of patients who were initially prescribed non operative management failed and these patients went on to undergo arthroscopic surgery.[43] It is generally recognized that the majority of patients with symptomatic SLAP lesions will fail conservative management, particularly throwers.[3]Given that conservative management only seems to be successful in a few patients, mainly in type I SLAP lesions, it is only implemented in patients with this type of lesion or patients who do not wish to undergo surgery.[3]
In the first step of conservative management, patients should abstain from aggravating activities in order to provide relief to the pain and inflammation. If necessary, NSAID’s and intra-articular corticosteroid injections can be applied to help diminish complaints.[3][43]This way, physical treatment can be started sooner. Strength, stability and motion are the components of shoulder function that should be focused on during rehabilitation.[44]This course of treatment should focus on restoring strength of the rotator cuff, shoulder girdle, trunk, core and scapular musculature, restoring normal shoulder motion, and training to improve dynamic joint stability.[3]
Regaining GIRD is a crucial aspect in the rehabilitation of SLAP lesions.[3]By the use of posterior capsule stretching exercises, such as sleeper stretch and cross body adduction stretches, and exercises for scapula stabilisation, redevelopment of the internal rotation can be accomplished.[43][45]
By stretching the posterior capsule and restoring internal rotation, through posterior capsule stretching exercises, such as sleeper stretch and cross body adduction stretches, and exercises for scapula stabilisation , pathologic contact between the supraspinatus tendon and the posterosuperior labrum.[43][45]can be prevented. The patient is eventually advanced to a strengthening phase, which includes trunk, core, rotator cuff, and scapular musculature. In throwing athletes, a progressive throwing program that is directed toward the patients' specific sport and position can be initiated after 3 months.[3]
Sixteen commonly used shoulder rehabilitation exercises can be chosen on the basis of several EMG studies and clinical recommendations regarding the rehabilitation of patients with SLAP lesions.
These exercises are:
- forward flexion in a side-lying position
- prone extension
- seated rowing
- serratus punch (protraction with the elbow extended)
- knee push-up plus
- forward flexion in external rotation and forearm supination
- full can (elevation in the scapular plane in external rotation)
- internal rotation in 20° of abduction
- external rotation in 20° of abduction
- internal rotation in 90° of abduction
- external rotation in 90° of abduction
- forearm supination, elbow flexion in forearm supination
- uppercut (combined forward flexion of the shoulder and flexion and supination of the elbow)
- internal rotation diagonal
- external rotation diagonal
These exercises, with increasing low to moderate activity, can be applied in the early and intermediate phases of nonoperative and postoperative treatment for patients with proximal biceps tendon disorders and SLAP lesions.[46]
When conservative treatment fails, a surgical approach is in order.[3]
After surgery, for 3 to 4 weeks, the shoulder of the patient is placed in a sling, which immobilises the shoulder in internal rotation and leads to general loss of motion and stiffness.[3][11]Postoperative rehabilitation is determined by the type of SLAP lesion, the chosen surgical procedure and other concomitant pathologies and procedures performed.[3]
Generally pendulum and elbow range-of-motion exercises are allowed during the period of immobilization. External rotation must absolutely be avoided and abduction limited to 60°. Assisted and passive techniques are used at 4 weeks post-operative to increase shoulder mobility. Between week 4 and 8, internal and external rotation ROM are progressively increased to 90° of shoulder abduction. Resistance exercises can be initiated at approximately 8 weeks post-operative, in which scapular strengthening should be emphasized. Since the metabolism of cartilage depends partly on its mechanical environment, resistance training can contribute to gaining mobility. However, the achievement of adequate shoulder mobility is an important condition to begin resistance training. At month 4 to 6, dependent on the type of sport practiced, patients should be able to start sport-specific training and gradually return to their former level of activity.[3]
SLAP lesion repair often fails, and biceps tenodesis or tenotomy seems to be an acceptable alternative treatment for SLAP lesions. Furthermore, this technique has now become the most preferable treatment for failed SLAP repairs.[47]The indications for biceps tenodesis as the index procedure for a symptomatic SLAP lesion depends on:
- the patient’s age
- activity level
- arm dominance
- type of sport.[11]
If a biceps tenodesis is performed a minimum of 10 weeks is recommended without biceps activity to allow the repaired soft tissue to fully incorporate into the bone tunnels.[12]
Key Evidence[edit | edit source]
Resources
[edit | edit source]
- Dutton Mark. Orthopaedic examination, evaluation, and intervention. New York: McGraw Hill; 2004.
- Dessaur WA. (2008). Diagnostic Accuracy of Clinical Testing for Superior Labral Anterior Posterior Lesions: A Systematic Review Journal of Orthopaedic and Sports
- Robert Manske, Daniel Prohaska. Superior labrum anterior to posterior (SLAP) rehabilitation in the overhead athlete. Physical Therapy in Sport 11, 2010, p.110-121.(Table 4). Rehablitation following arthroscopic type II SLAP repair.
Note: Strength training first weeks: 13 repetitions - 4 sequences – 1 to 3 minutes of rest between sequences
Strength training, build up to: 20 repetitions – 3 sequences – 1 minute of rest between sequences
Stretching: Total stretching time = 30 seconds for each stretch → 3x10” – 2x15” – 1x30” (build up)
30 to 60 seconds of rest between each stretch
- http://www.ouh.nhs.uk/shoulderandelbow/information/documents/OSI_Score13.pdf
- http://www.orthopaedicscore.com/scorepages/oxford_wosi_score.html
- http://www.wirral.nhs.uk/document_uploads/Commissioning/Appendix3-EQ5D3L.pdf
- http://www.euroqol.org/
- http://www.rheumatologynetwork.com/articles/taking-closer-look-rotator-cuff-disorders/page/0/2
Clinical bottom line
[edit | edit source]
SLAP lesions are lesions of the superior labrum in which there are several types described. A SLAP lesion is mainly caused by a fall on an outstretched arm where there is an important superior compression on the labrum which causes a tear of the labrum. A typical symptom is intermittent pain that also occurs in overhead movements. To diagnose this condition it is important to use several different tests and not only one. Physical examination is not easy because of the fact that SLAP lesions are often associated with other shoulder pathologies. For the physical examination the therapist uses the tests described in ‘Diagnostic Procedures’, but apart from that he can also test the glenohumeral and scapulothracic range of motion because there could occur a dyskinesis caused by the SLAP lesion. For the treatment of SLAP lesion one uses often a medical treatment where the surgeon uses advanced arthroscopic techniques. But a physical treatment is also possible. This includes stretching, strengthening, and stabilisation exercises.
It is important to note that every treatment depends on the type of the SLAP lesion and that conservative treatment may fail and is not suited to every patient.
Case Studies[edit | edit source]
Recent Related Research[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1nESb63TAKHoQUHW0i5DZbXKJYglsJko7_TQHWRNxhFvxXKA0: Error parsing XML for RSS
References[edit | edit source]
- ↑ ANDREWS JR et al., Glenoid labrum tears related to the long head of biceps. Am J Sports Med., 1985;13:337–341
- ↑ SNYDER SJ et al., SLAP lesions of the shoulder. Arthroscopy., 1990;6:274–279
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 CHRISTOPHER C. et al., SLAP Lesions: An Update on Recognition and Treatment. J Orthop Sports Phys Ther, 2009; 39(2):71-80
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 POWELL S.E. et al., The Diagnosis, Classification, and Treatment of SLAP Lesions. Oper Tech Sports Med, 2012;20 (1):46 – 56
- ↑ 5.0 5.1 5.2 5.3 PEAT M., Functional anatomy of the schoulder complex. Phys Ther., 1986;66:1855-1865
- ↑ 6.0 6.1 CARMICHAEL S.W. et al., Anatomy of the Shoulder Joint. The Journal Of Orthopaedic And Sports Physical Therapy, 1985;6(4):225-228
- ↑ 7.0 7.1 KOZIAK A. et al, Magnetic resonance arthrography assessment of the superior labrum using the BLC system: age-related changes mimicking SLAP-2 lesions. Skeletal Radiology, 2014;43: 1065 – 1070
- ↑ MYERS J.B. et al., Sensorimotor deficits contributing to glenohumeral instability. Clin Orthop Relat Res,2002; 400:98–104
- ↑ HUIJBREGTS P.A., SLAP Lesions: Structure, Function, and Physical Therapy Diagnosis and Treatment. The Journal of Manual & Manipulative Therapy, 2001;9(2):71 – 83
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 WILK K.E. et al, The recognition and treatment of superior labral (SLAP) lesions in the overhead athlete. Int. J. Sports Phys. Ther., 2013; 8(5): 579-600
- ↑ 11.0 11.1 11.2 11.3 11.4 HURI G. et al, Treatment of superior labrum anterior posterior lesions: a literature review. Acta Orthop Traumatol Turc., 2014;48(3): 290-297
- ↑ 12.00 12.01 12.02 12.03 12.04 12.05 12.06 12.07 12.08 12.09 12.10 12.11 12.12 12.13 12.14 12.15 MANSKE R. et al., Superior labrum anterior to posterior (SLAP) rehabilitation in the overhead athlete. Phys Ther Sport., 2010;110-121
- ↑ 13.0 13.1 KNESEK M. et al., Diagnosis and management of superior labral anterior posterior tears in throwing athlets. Am. J. Sports Med, 2013;41:444-460
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 14.14 NURI A. et al., Superior labrum anterior to posterior lesionsof the shoulder: Diagnosis ans arthoscopic management. World J. Orthop., 2014; 5(3): 344-350
- ↑ PAINE R. et al., The role of the scapula. Int. J. Sports. Phys. Ther., 2013;8(5):617-629
- ↑ 16.0 16.1 16.2 CLAVERT P., Glenoid labrum pathology. Orthop Traumatol Surg Res., 2015;101(1):19-24
- ↑ STETSON, W. (2010). SLAP Tear of the Shoulder. Retrieved from http://www.sportsmedicinedr.com/?page_id=715
- ↑ WILLIAM F.B., Correlation of the SLAP lesion with lesions of the medial sheath of the biceps tendon and intra-articular subscapularis tendon .Indian J Orthop. 2009 Oct-Dec; 43(4): 342–346
- ↑ WILK K.E. et al., Schoulder injuries in the overhead athlete. Journal of orthopaedic & sports physical therapy, 2009;39(2): 2009
- ↑ MORGAN CD et al., Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears, Arthroscopy 1998 Sep;14(6):553-65
- ↑ CHEN A.L. et al., Arthroscopic management of spinoglenoid cysts associated with SLAP lesions and suprascapular neuropathy. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 2003;19(6):15-21
- ↑ GASKILL T.R., The rotator interval: pathology and management, Journal of Arthroscopy and Related Surgery 2011, vol. 27, issue 4, p. 556-567
- ↑ EK E. et al., Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tendonesis. Journal of Shoulder and Elbow surgery, 2014;23(7): 1059 – 1065
- ↑ AMIN M. F. et al., The diagnostic value of magnetic resonance arthrography of the shoulder in detection and grading of SLAP lesions: Comparison with arthroscopic findings. European Journal of Radiology, 2012;81(3):2343 – 2347
- ↑ IQBAL H.J., Diagnostic value of MR Arthrogram in SLAP lesions of the shoulder, The Surgeon 2010, vol . 8, p. 303-309
- ↑ 26.0 26.1 26.2 26.3 26.4 SKARE Ø. et al., Responsiveness of outcome measures in patients with superior labral anterior and posterior lesions. Shoulder & Elbow, 2014;6(4):262-272
- ↑ JENSEN K.U. et al, Not all Rowe scores are the same! Which Rowe score do you use?, J Shoulder Elbow Surg., 2009;18(4):511-514
- ↑ DAWSON J. et al., The assessment of shoulder instability. The development and validation of a questionnaire. J Bone Joint Surg Br 1999; 81: 420–426
- ↑ KIRKLEY A.G. et al., The development and evaluation of a disease-specific quality of life measurements tool for shoulder instability. The western Ontario shoulder instability index (WOSI). Am J Sports Med., 1998;26:764-772
- ↑ 30.0 30.1 MESERVE B.B. et al., A meta-analysis examining clinical test utility for assessing superior labral anterior posterior lesions. American journal of sports medicine,2009;37:2252-2258
- ↑ 31.0 31.1 BOILEAU P. et al., Arthroscopic treatment of Isolated Type II SLAP lesions. Am J Sports Med., 2009;37:929–936
- ↑ Physiotutors. Dynamic Labral Shear Test | SLAP Lesion. Available from: https://www.youtube.com/watch?v=Vo7YBDwZAbk
- ↑ OH, J. H. et al., The evaluation of various physical examinations for the diagnosis of type II superior labrum anterior and posterior lesion. American Journal of Sports Medicine, 2008;36:353-359
- ↑ COOK C. et al., Diagnostic accuracy of five orthopedic clinical tests for diagnosis of superior labrum anterior posterior (SLAP) lesion. J Shoulder Elbow Surg., 2012;21(1):13 – 22
- ↑ SANDREY M.A., Special physical examination tests for superior labrum anterior-posterior shoulder tears: an examinatioin of clinical usefulness. Journal of Athl. Train., 2013;48(6):856-858
- ↑ Physiotutors. SLAP Lesion Cluster. Available from: https://www.youtube.com/watch?v=FRotc9Rx1Ak
- ↑ SAMANI J.E. et al., Arthroscopic stabilization of type II SLAP lesions using an absorbable tack. Arthroscopy., 2001;17:19–24
- ↑ PROVENCHER M.T. et al., A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med., 2013;41:880–886
- ↑ ALPERT J.M. et al., The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med., 2010;38:2299–2303
- ↑ HIGGINS L.D. et al., Superior labral lesions: anatomy, pathology, and treatment. Clin Orthop Relat Res., 2001;390:73–82
- ↑ D’ALESSANDRO D.F. et al., Superior Labral Lesions: Diagnosis and Management. J Athl Train., 2000;35(3):286–292
- ↑ XINNING L. et al., Management of type II superior labrum anterior posterior lesions: a review of the literature. 2010;6:16-22
- ↑ 43.0 43.1 43.2 43.3 EDWARDS S.L. et al., Non operative treatment of superior labrum anterior posterior tears - improvements in pain function and quality of life. Am J Sports Med., 2010;38:1456–1461
- ↑ SACCOL M.F. et al., Shoulder rotator strength and torque steadiness in athletes with anterior shoulder instability or SLAP lesion. Journal of Science and Medicine in Sport, 2014;17(5): 463–468
- ↑ 45.0 45.1 MAENHOUT A. et al., Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med., 2012;40(9):2105-2112
- ↑ COOLS A .M. et al., Rehabilitation Exercises for Athletes With Biceps Disorders and SLAP Lesions: A Continuum of Exercises With Increasing Loads on the Biceps. Am J Sports Med.,2014 ;42(6):1315-1322
- ↑ WEBER S.C., Surgical management of the failed SLAP repair. Sports Med Arthrosc.,2010;18:162-166







